Table 1. Summary of Central Connections, Components, Function, and Peripheral Distribution of the Vagus Nerve (Open Table in a new window)
| Components | Function | Central connection | Cell bodies | Peripheral distribution |
| Branchial motor (efferent special visceral) | Swallowing, phonation | Nucleus ambiguus | Nucleus ambiguus | Pharyngeal branches, superior and inferior laryngeal nerves |
| Visceral motor (efferent general visceral) | Involuntary muscle and gland control | Dorsal motor nucleus X | Dorsal motor nucleus X | Cardiac, pulmonary, esophageal, gastric, celiac plexuses, and muscles, and glands of the digestive tract |
| Visceral sensory (afferent general visceral) | Visceral sensibility | Nucleus tractus solitarius | Inferior ganglion X | Cervical, thoracic, abdominal fibers, and carotid and aortic bodies |
| Visceral sensory (afferent special visceral) | Taste | Nucleus tractus solitarius | Inferior ganglion X | Branches to epiglottis and taste buds |
| General sensory (afferent general somatic) | Cutaneous sensibility | Nucleus spinal tract V | Superior ganglion X | Auricular branch to external ear, meatus, and tympanic membrane |
Exit from the brain
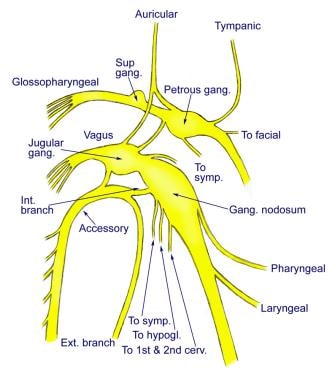
The vagus nerve exits from the medulla oblongata in the groove between the olive and the inferior cerebellar peduncle. It leaves the skull through the middle compartment of the jugular foramen, where it has upper and lower ganglionic swellings, which are the sensory ganglia of the nerve. The superior ganglion (jugular) is less than 0.5 cm in diameter, while the inferior (nodose) ganglion is larger (2.5 cm) and lies 1 cm distal to the superior ganglion (see the image below). The vagus nerve is joined by the cranial root of the accessory nerve (cranial nerve XI), just below the inferior ganglion. (See the images below.)[1, 2, 3, 4]
Course of the vagus nerve
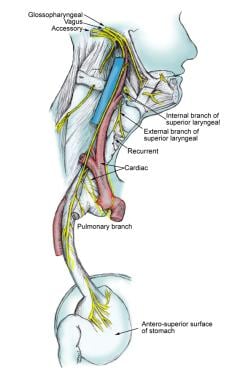
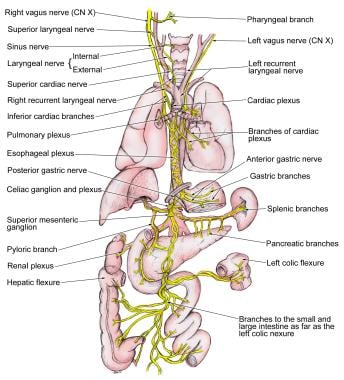
The vagus nerve descends vertically within the carotid sheath posterolateral to the internal and common carotid arteries and medial to the internal jugular vein (IJV) at the root of the neck.The right vagus crosses in front of the first part of the subclavian artery and then travels into the fat behind the innominate vessels. It then reaches the thorax on the right side of the trachea, which separates it from the right pleura. It then inclines behind the hilum of the right lung and courses medially toward the esophagus to form the esophageal plexus with the left vagus nerve. (See the image below.)
The left vagus crosses in front of the left subclavian artery to enter the thorax between the left common carotid and subclavian arteries. It descends on the left side of the aortic arch, which separates it from the left pleura, and travels behind the phrenic nerve. It courses behind the root of the left lung and then deviates medially and downwards to reach the esophagus and form the esophageal plexus by joining the opposite (right) vagus nerve.
Similarly, the posterior gastric nerve is formed mainly from the right vagus but contains fibers from the left vagus nerve. The gastric nerves supply all abdominal organs and the gastrointestinal tract ending just before the left colonic (splenic) flexure (see the images below).
Vagus nerve branches in the jugular foramen
The meningeal branch arises at the superior ganglion and reenters the cranium through the jugular foramen to supply the posterior fossa dura.Vagus nerve branches in the neck
The branches in the next consist of the following:- Pharyngeal branches
- Superior laryngeal nerve
- Recurrent laryngeal nerve
- Superior cardiac nerve
The pharyngeal branches arise from the inferior ganglion and contain sensory and motor fibers. The motor fibers are contributed by cranial nerve XI. They reach the middle constrictor muscle after crossing between the external and internal carotid arteries. They reach the pharyngeal plexus formed by cranial nerve IX and the sympathetic chain. Branches of the pharyngeal plexus supply the pharyngeal muscles and mucous membrane and palate except for the tensor palatini muscle.
Superior laryngeal nerve
The superior laryngeal nerve passes between the external and internal carotid arteries at the level of crossing of cranial nerve XII. At the tip of the hyoid, the superior laryngeal nerve divides into the external and internal branches. The internal laryngeal nerve pierces the thyrohyoid membrane to enter the larynx. The external nerve passes inferiorly with the superior thyroid vessels to the inferior pharyngeal constrictor muscle. The cricothyroid muscle is supplied by the external branch of the superior laryngeal nerve. The internal branch of the superior laryngeal supplies most of the mucosa above the glottis. It is divided into the following 3 divisions:
- First division - Supplies mucosa of the laryngeal surface of the epiglottis
- Middle division - Supplies the mucosa of the true and false vocal folds, as well as the aryepiglottic fold
- Inferior division - Supplies the arytenoid mucosa, anterior wall of the hypopharynx, upper esophageal sphincter, and part of the subglottis (the major part of the subglottis is innervated by the ipsilateral recurrent nerve)
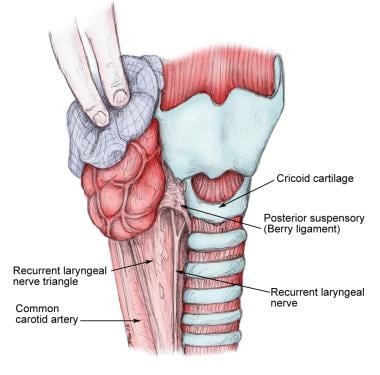
The recurrent laryngeal nerve is also known as the inferior laryngeal nerve. The right nerve branches from the vagus at the root of the neck around the right subclavian artery. It courses superiorly in the tracheoesophageal groove to enter the larynx between the cricopharyngeus and the esophagus.
The main trunk of the recurrent lies in a triangle bound laterally by the common carotid artery, the IJV, and the vagus nerve and medially by the trachea and esophagus. The recurrent nerve passes under the posterior suspensory ligament of Berry (located on either side of the trachea, extending from the cricoid cartilage and the first 2 tracheal rings to the posteromedial aspect of the thyroid gland), before entering the larynx (see the image below). A few variations may occur in this area (see Natural Variants).
All the intrinsic laryngeal musculature is supplied by the ipsilateral recurrent nerve except the cricothyroid muscle, which is supplied by the superior laryngeal nerve. The interarytenoid muscle is the only one that receives a bilateral supply (ie, from the left and right recurrent laryngeal nerves).
Superior cardiac nerve
The superior cardiac nerve is made up of 2-3 branches. They communicate with the sympathetic fibers.
Vagus nerve branches in the thorax
The inferior cardiac branch is also called the ramus cardiaci inferiors. On the right side, it arises from the trunk of the vagus as it lies beside the trachea. On the left side, it originates from the recurrent laryngeal nerve only. These branches end in the deep part of the cardiac plexus.The esophageal branches are anterior and posterior branches. Together they form the esophageal plexus. The posterior surface of the pericardium is supplied by filaments from this plexus.
Vagus nerve branches in the abdomen
The gastric branches (rami gastrici) supply the stomach. The right vagus forms the posterior gastric plexus and the left forms the anterior gastric plexus. The branches lie on the posteroinferior and the anterosuperior surfaces, respectively.The hepatic branches originate from the left vagus. They join the hepatic plexus and through it are distributed to the liver.
No comments:
Post a Comment