Sunday 31 August 2014
What makes MS UK far superior than MS Society,
They supply lots of alternative information based on very relevant studies, some that I have previously looked into.
CCSVI ?????????????? - MS Society???
Why the MS Society have not conducted its own comprehensive study into this subject, I do not know. CCSVI is a symptom of a misaligned Atlas. The Society raise millions and do nothing constructive with that money in regards to CCSVI research.
I ask the question WHY ?
I ask the question WHY ?
Info on MS UK - Alison Peebles - PPMS -Korean Physiotherapy Clinic- Chongsu LeeTherapist technique - yet again I rest my case
Every week Brendan Hilton steps into a high-pressure chamber, pulls a mask over his face and breathes in a high dose of oxygen. The 32-year-old, who suffers from multiple sclerosis, has found that the treatment eases symptoms of the incurable disease.
In the UK and Ireland about 5,000 patients regularly have oxygen therapy lasting about an hour in chambers holding up to 12 people.
It uses the same technology as in the pressurised cabins of passenger jets and some research suggests that delivering high doses of pure oxygen can reduce inflammation which is a key feature of MS.
The treatment is offered at more than 60 centres throughout the UK, each run as an individual charity.
"I feel energised and sleep better after having oxygen," says Brendan, a former car mechanic who was diagnosed with the disease seven years ago. He initially noticed that he was suffering from double vision but it took six years for the cause to be established.
"I was playing pool on holiday and couldn't see the balls properly," he explains. "I was also suffering from headaches. It happened again at work about a year later." Tests revealed a swelling on the nerve ending behind the eye. It was treated purely as a vision problem but is one of the first signs of MS.
Brendan adds: "It would flare up occasionally, then my mum pointed out that I was crossing my feet when I was walking. I realised it was due to a weakness in my right hip."
Finally following an MRI scan Brendan was called in urgently by a neurologist and told he had MS, a condition that affects the central nervous system including the brain, spinal cord and optic nerves.
"My first reaction was disbelief and I thought they had mixed up my medical records," says Brendan. "I didn't know much about MS and assumed I would end up in a wheelchair but as I learned more, I was determined to get on with life."
Brendan improved his diet, began exercising more and now rarely drinks alcohol. He also heard about the network of more than 60 MS Therapy Centres in the UK. They offer a range of treatments including oxygen therapy.
"I am open-minded and oxygen therapy made a lot of sense," says Brendan. "If you have an accident, oxygen is the first thing they give you. It's not a cure but I've no doubt that it helps."
Some studies suggest the treatment helps ease symptoms such as incontinence, pain and fatigue. However oxygen therapy divides medical opinion and is not available on the NHS for MS.
The use of oxygen to treat MS was introduced in the UK in Dundee in 1982. For reasons that are not clear but may be linked to lifestyle and climate, Scotland has one of the highest rates of MS in the world.
Petra Kliempt, co-ordinator for MS Therapy Centres, says: "Oxygen is the body's antibiotic. It helps against infection and the inflammation caused by MS."
The chambers used at the centres deliver air which is pressurised at twice the normal atmospheric level. This allows high doses of oxygen to reach and repair damaged tissue.
Some studies suggest that over a long period oxygen can slow the effects of MS. It is also claimed that the therapy can stimulate the production of stem cells which may allow some of the damage caused by MS to be repaired. Treatment tends to be more successful if begun soon after diagnosis.
Hyperbaric oxygen therapy was first used in 1887 to treat pneumonia and since the 1930s for deep-sea divers suffering from decompression sickness. It has also been used to help treat a range of illnesses and conditions including stroke, diabetes and brain injury.
Other studies have cast doubt on the treatment but Petra adds: "There are clear benefits and no side effects. I have not encountered any MS patients who report no improvement and for some it is dramatic. People have reported that the effects are like having a fog cleared from around their brain.
"However oxygen treatment is not a cure and people need to be realistic. If you are in a wheelchair it's not going to get you walking again. We do believe this treatment should be made available on the NHS but there is a lack of awareness among GPs while others are sceptical about the importance of using oxygen in treatment."
Ed Holloway of the MS Society says: "Some people with MS who receive hyperbaric oxygen therapy have found that it helps to improve their symptoms but others haven't found any benefit. There have been a number of studies looking into its potential benefits but overall they haven't found any clear evidence that it is an effective treatment."
Most patients have an intensive introductory course of 20 hour-long sessions then scale back depending on their symptoms. Anyone having the treatment is asked to make a small donation. There are about 100,000 MS sufferers in the UK so oxygen therapy is still only being used by a fraction. The condition occurs most commonly in people aged between 20 and 40 and twice as many women as men are affected.
Brendan, who has the relapsingremitting form of MS, has oxygen therapy at a centre near his home in Hereford alongside conventional drug treatment. Although he still struggles with his balance due to leg weakness his condition is now more stable and he is able to enjoy hobbies including fishing. Next year he is due to get married to Helen, a supervisor at the centre.
He says: "If I miss a session I really notice the difference. Even with oxygen treatment I still have times when I can't face the world and just have to take it easy.
"However when you have an incurable condition anything that works for you has to be worth it."
Source: The Daily Express Copyright ©2014 Northern and Shell Media Publications (07/01/14)
In the UK and Ireland about 5,000 patients regularly have oxygen therapy lasting about an hour in chambers holding up to 12 people.
It uses the same technology as in the pressurised cabins of passenger jets and some research suggests that delivering high doses of pure oxygen can reduce inflammation which is a key feature of MS.
The treatment is offered at more than 60 centres throughout the UK, each run as an individual charity.
"I feel energised and sleep better after having oxygen," says Brendan, a former car mechanic who was diagnosed with the disease seven years ago. He initially noticed that he was suffering from double vision but it took six years for the cause to be established.
"I was playing pool on holiday and couldn't see the balls properly," he explains. "I was also suffering from headaches. It happened again at work about a year later." Tests revealed a swelling on the nerve ending behind the eye. It was treated purely as a vision problem but is one of the first signs of MS.
Brendan adds: "It would flare up occasionally, then my mum pointed out that I was crossing my feet when I was walking. I realised it was due to a weakness in my right hip."
Finally following an MRI scan Brendan was called in urgently by a neurologist and told he had MS, a condition that affects the central nervous system including the brain, spinal cord and optic nerves.
"My first reaction was disbelief and I thought they had mixed up my medical records," says Brendan. "I didn't know much about MS and assumed I would end up in a wheelchair but as I learned more, I was determined to get on with life."
Brendan improved his diet, began exercising more and now rarely drinks alcohol. He also heard about the network of more than 60 MS Therapy Centres in the UK. They offer a range of treatments including oxygen therapy.
"I am open-minded and oxygen therapy made a lot of sense," says Brendan. "If you have an accident, oxygen is the first thing they give you. It's not a cure but I've no doubt that it helps."
Some studies suggest the treatment helps ease symptoms such as incontinence, pain and fatigue. However oxygen therapy divides medical opinion and is not available on the NHS for MS.
The use of oxygen to treat MS was introduced in the UK in Dundee in 1982. For reasons that are not clear but may be linked to lifestyle and climate, Scotland has one of the highest rates of MS in the world.
Petra Kliempt, co-ordinator for MS Therapy Centres, says: "Oxygen is the body's antibiotic. It helps against infection and the inflammation caused by MS."
The chambers used at the centres deliver air which is pressurised at twice the normal atmospheric level. This allows high doses of oxygen to reach and repair damaged tissue.
Some studies suggest that over a long period oxygen can slow the effects of MS. It is also claimed that the therapy can stimulate the production of stem cells which may allow some of the damage caused by MS to be repaired. Treatment tends to be more successful if begun soon after diagnosis.
Hyperbaric oxygen therapy was first used in 1887 to treat pneumonia and since the 1930s for deep-sea divers suffering from decompression sickness. It has also been used to help treat a range of illnesses and conditions including stroke, diabetes and brain injury.
Other studies have cast doubt on the treatment but Petra adds: "There are clear benefits and no side effects. I have not encountered any MS patients who report no improvement and for some it is dramatic. People have reported that the effects are like having a fog cleared from around their brain.
"However oxygen treatment is not a cure and people need to be realistic. If you are in a wheelchair it's not going to get you walking again. We do believe this treatment should be made available on the NHS but there is a lack of awareness among GPs while others are sceptical about the importance of using oxygen in treatment."
Ed Holloway of the MS Society says: "Some people with MS who receive hyperbaric oxygen therapy have found that it helps to improve their symptoms but others haven't found any benefit. There have been a number of studies looking into its potential benefits but overall they haven't found any clear evidence that it is an effective treatment."
Most patients have an intensive introductory course of 20 hour-long sessions then scale back depending on their symptoms. Anyone having the treatment is asked to make a small donation. There are about 100,000 MS sufferers in the UK so oxygen therapy is still only being used by a fraction. The condition occurs most commonly in people aged between 20 and 40 and twice as many women as men are affected.
Brendan, who has the relapsingremitting form of MS, has oxygen therapy at a centre near his home in Hereford alongside conventional drug treatment. Although he still struggles with his balance due to leg weakness his condition is now more stable and he is able to enjoy hobbies including fishing. Next year he is due to get married to Helen, a supervisor at the centre.
He says: "If I miss a session I really notice the difference. Even with oxygen treatment I still have times when I can't face the world and just have to take it easy.
"However when you have an incurable condition anything that works for you has to be worth it."
Source: The Daily Express Copyright ©2014 Northern and Shell Media Publications (07/01/14)
Actress tells of revolutionary M S treatment(29/07/13)
Actress Alison Peebles has spoken of a huge improvement in her multiple sclerosis after a revolutionary new treatment.
She had been expecting the primary progressive multiple sclerosis that has blighted her life to quickly leave her dependent on the use of a wheelchair.
However, the leading Scottish actress, whose TV credits include BBC's River City and Shetland, believes a new physiotherapy has greatly improved the quality of her life – and delayed the need for a chair.
Peebles, from Wester Hailes, has been receiving treatment from the Korean Physiotherapy Clinic In Edinburgh, where therapist Chongsu Lee uses a technique that involves gentle manipulation of the spine and surrounding soft tissue to release tension.
It is claimed that as tension around the spine gradually eases off, blood and lymph circulation and nerve function improve.
"The benefits of the treatment have been quite dramatic," said Peebles, who has starred as Lady Macbeth on stage. "I was collapsing all the time as I had poor balance and strength. I was mentally and physically exhausted.
"Now, after 18 weeks of treatment, my walking, balance and vision are hugely improved and my body is much more flexible. I still use a crutch, but if I continue like this, I feel optimistic that I can keep on my feet and delay the imminent need for a wheelchair."
Peebles, 53, a co-founder of the Communicado Theatre Company, has suffered from primary progressive MS, which is characterised by a worsening of symptoms, since 2001.
She wrote and performed the 2012 theatre play My Shrinking Life as a response to her disability, and as a reflection on what it means to play a part in which she was unwillingly cast.
The actress and director continues to work. She will direct the play Bite The Bullet , by Sandy Nelson and Keith Warwick, at the Edinburgh Fringe in August. "I am more supple," I am standing straighter, and I have more energy," she added.
Scientists recently reported they may be a step closer to repairing the damage caused by MS.
Researchers at Edinburgh and Cambridge universities have pinpointed a process that helps to produce more myelin – the sheath surrounding the central nervous system.
Scotland has the highest prevalence of MS in the world, with about 10,500 people affected.
Source: heraldscotland © Copyright 2013 Herald
She had been expecting the primary progressive multiple sclerosis that has blighted her life to quickly leave her dependent on the use of a wheelchair.
However, the leading Scottish actress, whose TV credits include BBC's River City and Shetland, believes a new physiotherapy has greatly improved the quality of her life – and delayed the need for a chair.
Peebles, from Wester Hailes, has been receiving treatment from the Korean Physiotherapy Clinic In Edinburgh, where therapist Chongsu Lee uses a technique that involves gentle manipulation of the spine and surrounding soft tissue to release tension.
It is claimed that as tension around the spine gradually eases off, blood and lymph circulation and nerve function improve.
"The benefits of the treatment have been quite dramatic," said Peebles, who has starred as Lady Macbeth on stage. "I was collapsing all the time as I had poor balance and strength. I was mentally and physically exhausted.
"Now, after 18 weeks of treatment, my walking, balance and vision are hugely improved and my body is much more flexible. I still use a crutch, but if I continue like this, I feel optimistic that I can keep on my feet and delay the imminent need for a wheelchair."
Peebles, 53, a co-founder of the Communicado Theatre Company, has suffered from primary progressive MS, which is characterised by a worsening of symptoms, since 2001.
She wrote and performed the 2012 theatre play My Shrinking Life as a response to her disability, and as a reflection on what it means to play a part in which she was unwillingly cast.
The actress and director continues to work. She will direct the play Bite The Bullet , by Sandy Nelson and Keith Warwick, at the Edinburgh Fringe in August. "I am more supple," I am standing straighter, and I have more energy," she added.
Scientists recently reported they may be a step closer to repairing the damage caused by MS.
Researchers at Edinburgh and Cambridge universities have pinpointed a process that helps to produce more myelin – the sheath surrounding the central nervous system.
Scotland has the highest prevalence of MS in the world, with about 10,500 people affected.
Source: heraldscotland © Copyright 2013 Herald
Info on MS UK - Bacteria and viruses - Parkinson's and MS
Bacteria and viruses

Could the first sign of Parkinson's and multiple sclerosis be a dodgy tummy? (23/06/14)
Anxiety or anticipation can often lead to a feeling of ‘butterflies in the stomach’ – which usually dissipates along with the source of the consternation.
But scientists have discovered that the nerve pathways between the gut and the brain that cause this phenomenon may also be linked to degenerative illnesses such as Parkinson’s disease and multiple sclerosis (MS), as well as some mental health problems.
Dr Anton Emmanuel, consultant neuro-gastroenterologist at University College London and the National Hospital for Neurology, explained: ‘The gut and brain share the same nerve chemistry and have a dialogue.
'That’s why when you feel stress and other strong emotions, such as fear, it leads to gastrointestinal symptoms, like rushing to the loo.’
A new study suggests that brain disease can be caused by an unhealthy gut because these signals also travel in the opposite direction.
The study, which was published in the journal Movement Disorders, found that sufferers of Parkinson’s disease had a higher prevalence of a condition called small intestinal bacterial overgrowth, or SIBO.
In SIBO, normally harmless bacteria proliferate in large numbers in the small intestine.
Symptoms include excess gas, abdominal bloating, diarrhoea and abdominal pain. Nobody is sure how many people have it, as it often goes undiagnosed or is confused with irritable bowel syndrome, but estimates are of up to 300,000 British sufferers.
And the researchers suggest that the bacteria may produce chemicals that affect the nerves in the gut, which pass on the damage to the brain – and result in Parkinson’s and MS. Dr Emmanuel said: ‘We now think that neurological diseases such as MS and Parkinson’s are linked to the gut being more leaky, permitting pathogens into the bloodstream and causing an antibody response. Either the pathogens, directly, or the immune response, indirectly, may damage nerve tissue.’
The damaged nerves then transmit these detrimental signals to the brain.
In Parkinson’s, a small part of the brain becomes progressively damaged over many years, something that affects mainly older people. MS is the most common neurological disease in young adults and occurs when the immune system attacks the nervous system.
The two diseases affect about 100,000 and 127,00 people in the UK respectively. Both have wide-ranging symptoms, affecting movement as well as causing tiredness, pain and depression. There are drugs that can ease symptoms, but no cure or even treatments that significantly slow down progression of the diseases.
Scientists hope that this discovery will pave the way for new treatments for both these disabling conditions.
They are now mapping the ‘bacterial genome’, which will identify the bacteria in an individual’s gut – something they hope will ultimately allow doctors to prescribe tailored treatments for leakiness of the gut, improving neurological symptoms in turn.
Until then, the doctors’ body United European Gastroenterology urges people to maintain a healthy diet, including foods that boost good bacteria and encourage efficient digestion. This may have an especially positive effect on mood disorders such as anxiety and depression.
They recommend eating plenty of fibre and probiotics such as live yogurt, as well as limiting sugar, processed foods, animal fat and the use of antibiotics, antacids and anti-inflammatories, as these cause imbalances in the gut.
Source: The Daily Mail © Associated Newspapers Ltd (23/06/14)
But scientists have discovered that the nerve pathways between the gut and the brain that cause this phenomenon may also be linked to degenerative illnesses such as Parkinson’s disease and multiple sclerosis (MS), as well as some mental health problems.
Dr Anton Emmanuel, consultant neuro-gastroenterologist at University College London and the National Hospital for Neurology, explained: ‘The gut and brain share the same nerve chemistry and have a dialogue.
'That’s why when you feel stress and other strong emotions, such as fear, it leads to gastrointestinal symptoms, like rushing to the loo.’
A new study suggests that brain disease can be caused by an unhealthy gut because these signals also travel in the opposite direction.
The study, which was published in the journal Movement Disorders, found that sufferers of Parkinson’s disease had a higher prevalence of a condition called small intestinal bacterial overgrowth, or SIBO.
In SIBO, normally harmless bacteria proliferate in large numbers in the small intestine.
Symptoms include excess gas, abdominal bloating, diarrhoea and abdominal pain. Nobody is sure how many people have it, as it often goes undiagnosed or is confused with irritable bowel syndrome, but estimates are of up to 300,000 British sufferers.
And the researchers suggest that the bacteria may produce chemicals that affect the nerves in the gut, which pass on the damage to the brain – and result in Parkinson’s and MS. Dr Emmanuel said: ‘We now think that neurological diseases such as MS and Parkinson’s are linked to the gut being more leaky, permitting pathogens into the bloodstream and causing an antibody response. Either the pathogens, directly, or the immune response, indirectly, may damage nerve tissue.’
The damaged nerves then transmit these detrimental signals to the brain.
In Parkinson’s, a small part of the brain becomes progressively damaged over many years, something that affects mainly older people. MS is the most common neurological disease in young adults and occurs when the immune system attacks the nervous system.
The two diseases affect about 100,000 and 127,00 people in the UK respectively. Both have wide-ranging symptoms, affecting movement as well as causing tiredness, pain and depression. There are drugs that can ease symptoms, but no cure or even treatments that significantly slow down progression of the diseases.
Scientists hope that this discovery will pave the way for new treatments for both these disabling conditions.
They are now mapping the ‘bacterial genome’, which will identify the bacteria in an individual’s gut – something they hope will ultimately allow doctors to prescribe tailored treatments for leakiness of the gut, improving neurological symptoms in turn.
Until then, the doctors’ body United European Gastroenterology urges people to maintain a healthy diet, including foods that boost good bacteria and encourage efficient digestion. This may have an especially positive effect on mood disorders such as anxiety and depression.
They recommend eating plenty of fibre and probiotics such as live yogurt, as well as limiting sugar, processed foods, animal fat and the use of antibiotics, antacids and anti-inflammatories, as these cause imbalances in the gut.
Source: The Daily Mail © Associated Newspapers Ltd (23/06/14)
(info on MS UK) - People with MS may have a higher risk of developing cancer - I rest my case
Patients with MS may suffer a high risk of developing cancer - study(16/01/14)
The study reported in the European Journal of Neurology claims that people suffering from multiple sclerosis, an autoimmune disease affecting nerves in brain and spinal cord, have a higher risk of developing cancer, especially breast cancer.
Studies conducted earlier claimed that people with autoimmune disease may suffer from a greater risk of developing cancer but most of the studies detected no association between multiple sclerosis (MS) and cancer. Since this latest finding contradicts the previous findings, researchers say that additional research is required to determine whether or not there is a link between the disease and cancer.
For the study, researchers evaluated the data retrieved from the National Health Insurance System of Taiwan. They assessed the information on 1292 people who were diagnosed with MS between 1997 and 2010. They further matched each MS patient with four healthy people who were not diagnosed with the condition.
MS that is not considered as a fatal disease is a chronic and unpredictable disease. It normally affects people between the ages of 20 and 50. This autoimmune disease causes extreme fatigue, blindness, paralysis, poor coordination and more. There are more than 2.5 million people around the world living with MS.
This investigation was led by Li-Min Sun, MD, of the Zuoying Branch of Kaohsiung Armed Forces General Hospital in Kaohsiung, Taiwan.
"Our study was a nationwide population-based cohort study, and it revealed unexpected findings," said Dr. Sun
The researchers noticed that those with MS suffered 85 percent higher risk of developing cancer when compared to the control group. There was a twofold higher risk of developing breast cancer when compared to the control group.
This study suggests that those with MS should be monitored closely in order to ensure the early detection of cancer.
Unsure of why the results of this study differs from the previous studies, Dr. Sun notes says, "The underlying genetic and environmental factors in Taiwan, which differ from those of western countries, might play an undetermined role. Additional large-scale studies will help improve our understanding."
Studies conducted earlier claimed that people with autoimmune disease may suffer from a greater risk of developing cancer but most of the studies detected no association between multiple sclerosis (MS) and cancer. Since this latest finding contradicts the previous findings, researchers say that additional research is required to determine whether or not there is a link between the disease and cancer.
For the study, researchers evaluated the data retrieved from the National Health Insurance System of Taiwan. They assessed the information on 1292 people who were diagnosed with MS between 1997 and 2010. They further matched each MS patient with four healthy people who were not diagnosed with the condition.
MS that is not considered as a fatal disease is a chronic and unpredictable disease. It normally affects people between the ages of 20 and 50. This autoimmune disease causes extreme fatigue, blindness, paralysis, poor coordination and more. There are more than 2.5 million people around the world living with MS.
This investigation was led by Li-Min Sun, MD, of the Zuoying Branch of Kaohsiung Armed Forces General Hospital in Kaohsiung, Taiwan.
"Our study was a nationwide population-based cohort study, and it revealed unexpected findings," said Dr. Sun
The researchers noticed that those with MS suffered 85 percent higher risk of developing cancer when compared to the control group. There was a twofold higher risk of developing breast cancer when compared to the control group.
This study suggests that those with MS should be monitored closely in order to ensure the early detection of cancer.
Unsure of why the results of this study differs from the previous studies, Dr. Sun notes says, "The underlying genetic and environmental factors in Taiwan, which differ from those of western countries, might play an undetermined role. Additional large-scale studies will help improve our understanding."
When are they going to stop chopping and changing their minds, when will they realise they have got the "ms" thing wrong
#1
Back in limbo land ? : /
Righto, a weird one this. You know about me and how over the last 2 or more years I've had MS symptoms. I had MRI, this showed lesions. Well, last month I had another MRI. I'm told by my doctor, 'I'm sorry, it's MS' ? Well....this is where it starts getting weird.
I had an appointment with my Crohn's disease specialist. Me and my husband told him that I wanted to come off Humira ( my Crohns treatment) as I'd been on it for 6 years and as my Crohns was fine, why not? He looked at my new MRI results. He said ' it's not MS' !!!! After bursting into tears, I asked how is that and he said, the lesions have not changed since the last MRI. The LP showed no signs, and the eye test and flashy light thing all showed negative,; this is the first time we have been told these results, some of them were done 2 years ago !
so, after the most relief I think I've EVER felt in my life, we chatted about the possibility that the Humira may have caused the lesions in my brain and the Neuro symptoms. I mean, every symptom is classic of MS ( probably why they told me I had it). So ! The upshot of it is, I am now off my injections to see if it is the injections causing it. I've been told that I should see an improvement within the month if it's the Humira. Meanwhile, I'm going to be going through the worst withdrawal until it gets out of my system. I've got 2 months without the treatment, if my condition improves...there's our answer. If not, by that time I will be seeing my Neuro. Now it's just time to wait and see.
when I last saw my Neuro, he said ' if it's not MS, it's one of 2 other things that aren't so nice'. Well, I'm hoping that that isn't the case now after the new MRI. As for my doctor who told me I have MS....he got that one wrong!
I hope this essay(lol) gives hope to others. They got it so wrong with me, despite them telling me that I have MS. Of course, I'm being objective at the same time until I hear it from my Neuro's mouth, I'm not daft. But, I do have the glimpse of hope that I've not had before.
i will keep you all updated as I hear any news, but I'm keeping my fingers crossed :)
i hope you are all alright
xxxx
I had an appointment with my Crohn's disease specialist. Me and my husband told him that I wanted to come off Humira ( my Crohns treatment) as I'd been on it for 6 years and as my Crohns was fine, why not? He looked at my new MRI results. He said ' it's not MS' !!!! After bursting into tears, I asked how is that and he said, the lesions have not changed since the last MRI. The LP showed no signs, and the eye test and flashy light thing all showed negative,; this is the first time we have been told these results, some of them were done 2 years ago !
so, after the most relief I think I've EVER felt in my life, we chatted about the possibility that the Humira may have caused the lesions in my brain and the Neuro symptoms. I mean, every symptom is classic of MS ( probably why they told me I had it). So ! The upshot of it is, I am now off my injections to see if it is the injections causing it. I've been told that I should see an improvement within the month if it's the Humira. Meanwhile, I'm going to be going through the worst withdrawal until it gets out of my system. I've got 2 months without the treatment, if my condition improves...there's our answer. If not, by that time I will be seeing my Neuro. Now it's just time to wait and see.
when I last saw my Neuro, he said ' if it's not MS, it's one of 2 other things that aren't so nice'. Well, I'm hoping that that isn't the case now after the new MRI. As for my doctor who told me I have MS....he got that one wrong!
I hope this essay(lol) gives hope to others. They got it so wrong with me, despite them telling me that I have MS. Of course, I'm being objective at the same time until I hear it from my Neuro's mouth, I'm not daft. But, I do have the glimpse of hope that I've not had before.
i will keep you all updated as I hear any news, but I'm keeping my fingers crossed :)
i hope you are all alright
xxxx
Is CIDP just yet another misdiagnosis
Chronic Inflammatory Demyelinating Polyradiculoneuropathy
- Author: Richard A Lewis, MD; Chief Editor: Nicholas Lorenzo, MD, CPE more...
Practice Essentials
The term chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) has been used to identify patients with a chronically progressive or relapsing symmetric sensorimotor disorder with cytoalbuminologic dissociation and interstitial and perivascular endoneurial infiltration by lymphocytes and macrophages. It can be considered the chronic equivalent of acute inflammatory demyelinating polyradiculoneuropathy, the most common form of Guillain-Barré syndrome.
Symptoms reported include the following:
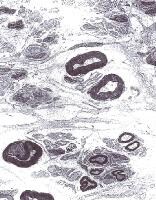 Electron micrograph of the peripheral nerve of a patient with chronic inflammatory demyelinating polyradiculoneuropathy. Note "onion bulb" formation in the myelin sheath of the nerve fibers due to continuous demyelination and remyelination. Courtesy of A. Sima, MD, Department of Pathology, Wayne State University.
Electron micrograph of the peripheral nerve of a patient with chronic inflammatory demyelinating polyradiculoneuropathy. Note "onion bulb" formation in the myelin sheath of the nerve fibers due to continuous demyelination and remyelination. Courtesy of A. Sima, MD, Department of Pathology, Wayne State University.
Signs and symptoms
CIDP typically starts insidiously and evolves slowly, in either a slowly progressive or a relapsing manner, with partial or complete recovery between recurrences; periods of worsening and improvement usually last weeks or months. Most experts consider the necessary duration of symptoms to be greater than 8 weeks for the diagnosis of CIDP to be made.Symptoms reported include the following:
- Preceding infection (infrequent)
- Initial limb weakness, both proximal and distal
- Sensory symptoms (eg, tingling and numbness of hands and feet)
- Motor symptoms (usually predominant)
- In about 16% of patients, a relatively acute or subacute onset of symptoms
- In children, usually a more precipitous onset of symptoms
- Symptoms of autonomic system dysfunction (eg, orthostatic dizziness)
- Signs of cranial nerve (CN) involvement (eg, facial muscle paralysis or diplopia)
- Gait abnormalities
- Motor deficits (eg, symmetric weakness of both proximal and distal muscles in upper and lower extremities)
- Diminished or absent deep tendon reflexes
- Sensory deficits (typically in stocking-glove distribution)
- Impaired coordination
Diagnosis
Laboratory studies that may be helpful include the following:- Cerebrospinal fluid analysis: Elevated protein levels are common (80% of patients); 10% of patients also have mild lymphocytic pleocytosis and increased gamma globulin
- Complete blood count (CBC), erythrocyte sedimentation rate (ESR), antinuclear antibody (ANA) level, biochemistry profile, and serum and urine immunoelectrophoresis (to exclude associated systemic disorders)
- In certain instances, genetic testing
- MRI of the spine with gadolinium enhancement
- Electromyography (EMG) is a critical test to determine whether the disorder is truly a peripheral neuropathy and whether the neuropathy is demyelinating
- Peripheral (sural) nerve biopsy: This is considered when the diagnosis is not completely clear, when other causes cannot be excluded, or when profound axonal involvement is observed on EMG; biopsy was once commonly recommended for most patients before immunosuppressive therapy, but current guidelines no longer recommend it
Management
Principles of treatment are as follows:- CIDP must be treated to prevent accumulating disability that necessitates physical and occupational therapy, orthotic devices, and long-term treatment
- Close follow-up care is necessary to adjust treatment
- Surgical and orthopedic consultation may be required for sural nerve biopsy or in severe disease with joint deformities
- Consultation with a neurologist is warranted
- Consultation with a physical medicine and rehabilitation specialist is appropriate for physical and occupational therapy and evaluation for orthotic devices
- Other consultations may be necessary if associated diseases are present
- Physical therapy and an active lifestyle should be encouraged
Image library
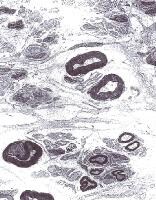 Electron micrograph of the peripheral nerve of a patient with chronic inflammatory demyelinating polyradiculoneuropathy. Note "onion bulb" formation in the myelin sheath of the nerve fibers due to continuous demyelination and remyelination. Courtesy of A. Sima, MD, Department of Pathology, Wayne State University.
Electron micrograph of the peripheral nerve of a patient with chronic inflammatory demyelinating polyradiculoneuropathy. Note "onion bulb" formation in the myelin sheath of the nerve fibers due to continuous demyelination and remyelination. Courtesy of A. Sima, MD, Department of Pathology, Wayne State University. Background
Chronic inflammatory demyelinating polyradiculoneuropathy is presumed to occur because of immunologic antibody-mediated reaction along with interstitial and perivascular infiltration of the endoneurium with inflammatory T cells and macrophages. The consequence is a segmental demyelination of peripheral nerves.
Human leukocyte antigens Dw3, DRw3, A1, and B8 occur more frequently in patients with CIDP than in the healthy population.
Cytoalbuminologic dissociation is a characteristic finding in cerebrospinal fluid (CSF) pointing to nerve root involvement. Occasionally, CSF studies reveal mild lymphocytic pleocytosis and elevation of gamma globulin level, but this is observed most frequently in HIV-positive patients.
The term chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) has been used to identify patients with a chronically progressive or relapsing symmetric sensorimotor disorder with cytoalbuminologic dissociation and interstitial and perivascular endoneurial infiltration by lymphocytes and macrophages. In many ways, CIDP can be considered the chronic equivalent of acute inflammatory demyelinating polyradiculoneuropathy (AIDP), the most common form of Guillain-Barré syndrome (GBS).
A number of variants of CIDP have been described that have immune or inflammatory aspects and electrophysiologic and/or pathologic evidence of demyelination in common. No consensus exists on the best approach to the nomenclature of these disorders. CIDP is a major subset of chronic acquired demyelinating polyneuropathies (CADP). In this context, CIDP is considered when patients have a symmetric proximal and distal motor predominant disorder.
CIDP variants include patients with predominantly sensory symptoms, those with a distal symmetric disorder (DADS), those with multifocal sensorimotor neuropathy or sensorimotor mononeuropathy multiplex with prominent conduction block (also known as Lewis-Sumner neuropathy), and those with CIDP with associated CNS demyelination or with other systemic disorders.
The following disorders are considered distinct from CIDP because they have specific pathophysiologic features and respond to treatments differently than do patients with CIDP: Demyelinating neuropathies associated with immunoglobulin M (IgM) paraproteins, including those with anti–myelin-associated glycoprotein (MAG) antibodies; polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, and skin changes (POEMS) syndrome; and multifocal motor neuropathy.
Human leukocyte antigens Dw3, DRw3, A1, and B8 occur more frequently in patients with CIDP than in the healthy population.
Cytoalbuminologic dissociation is a characteristic finding in cerebrospinal fluid (CSF) pointing to nerve root involvement. Occasionally, CSF studies reveal mild lymphocytic pleocytosis and elevation of gamma globulin level, but this is observed most frequently in HIV-positive patients.
The term chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) has been used to identify patients with a chronically progressive or relapsing symmetric sensorimotor disorder with cytoalbuminologic dissociation and interstitial and perivascular endoneurial infiltration by lymphocytes and macrophages. In many ways, CIDP can be considered the chronic equivalent of acute inflammatory demyelinating polyradiculoneuropathy (AIDP), the most common form of Guillain-Barré syndrome (GBS).
A number of variants of CIDP have been described that have immune or inflammatory aspects and electrophysiologic and/or pathologic evidence of demyelination in common. No consensus exists on the best approach to the nomenclature of these disorders. CIDP is a major subset of chronic acquired demyelinating polyneuropathies (CADP). In this context, CIDP is considered when patients have a symmetric proximal and distal motor predominant disorder.
CIDP variants include patients with predominantly sensory symptoms, those with a distal symmetric disorder (DADS), those with multifocal sensorimotor neuropathy or sensorimotor mononeuropathy multiplex with prominent conduction block (also known as Lewis-Sumner neuropathy), and those with CIDP with associated CNS demyelination or with other systemic disorders.
The following disorders are considered distinct from CIDP because they have specific pathophysiologic features and respond to treatments differently than do patients with CIDP: Demyelinating neuropathies associated with immunoglobulin M (IgM) paraproteins, including those with anti–myelin-associated glycoprotein (MAG) antibodies; polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, and skin changes (POEMS) syndrome; and multifocal motor neuropathy.
Pathophysiology
Chronic inflammatory demyelinating polyradiculoneuropathy is presumed to occur because of immunologic antibody-mediated reaction along with interstitial and perivascular infiltration of the endoneurium with inflammatory T cells and macrophages. The consequence is a segmental demyelination of peripheral nerves.
Human leukocyte antigens Dw3, DRw3, A1, and B8 occur more frequently in patients with CIDP than in the healthy population.
Cytoalbuminologic dissociation is a characteristic finding in cerebrospinal fluid (CSF) pointing to nerve root involvement. Occasionally, CSF studies reveal mild lymphocytic pleocytosis and elevation of gamma globulin level, but this is observed most frequently in HIV-positive patients.
Human leukocyte antigens Dw3, DRw3, A1, and B8 occur more frequently in patients with CIDP than in the healthy population.
Cytoalbuminologic dissociation is a characteristic finding in cerebrospinal fluid (CSF) pointing to nerve root involvement. Occasionally, CSF studies reveal mild lymphocytic pleocytosis and elevation of gamma globulin level, but this is observed most frequently in HIV-positive patients.
Frequency
International
CIDP is uncommon. The estimated prevalence of CIDP in populations from the UK, Australia, Italy, Norway, and Japan is 0.8-7.7 per 100,000. A 2009 study showed that the incidence and prevalence is variable depending on diagnostic criteria. In Rutland, UK on May 1, 2008, the prevalence of CIDP was 4.77/100,000 if the EFNS/PNS criteria were used but only 1.97 per 100,000 if the AAN criteria were used. Similarly the annual incidence was 0.7 per 100,000 using the EFNS criteria and 0.35 using the AAN criteria.[1]Mortality/Morbidity
Chronic inflammatory demyelinating polyradiculoneuropathy most commonly has an insidious onset and either chronic progressive or relapsing course. Occasionally, complete remissions occur. Quadriplegia, respiratory failure, and death have been described but are rare.
Race
No racial predilection has been identified.Sex
Both sexes are affected. Of CADP variants, multifocal motor neuropathy has a male predominance of at least 2:1 based on a survey of the largest case series.Age
Chronic inflammatory demyelinating polyradiculoneuropathy may occur at any age, but it is more common in the fifth and sixth decades. Relapsing course is associated with younger age of patients (third and fourth decades). CIDP has been described in childhood.
Previous
Proceed to Clinical Presentation
Contributor Information and Disclosures
Author
Richard A Lewis, MD Professor and Associate Chairman of Neurology, Department of Neurology, Wayne State University School of Medicine Richard A Lewis, MD is a member of the following medical societies: American Academy of Neurology, American Association of Neuromuscular and Electrodiagnostic Medicine, American Neurological Association, and Peripheral Nerve Society
Disclosure: GBS/CIDP FI Grant/research funds Other; Baxter Consulting fee Consulting; Baxter Grant/research funds None; CSL Behring Consulting fee Consulting
Specialty Editor Board
Dianna Quan, MD Professor of Neurology, Director, Electromyography Laboratory, University of Colorado School of Medicine Dianna Quan, MD is a member of the following medical societies: American Academy of Neurology, American Association of Neuromuscular and Electrodiagnostic Medicine, and Phi Beta Kappa
Disclosure: e-medicine Honoraria Other; Pfizer Grant/research funds Independent contractor; Alnylam Grant/research funds Independent contractor
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference
Disclosure: Medscape Salary Employment
Florian P Thomas, MD, MA, PhD, Drmed Director, Regional MS Center of Excellence, St Louis Veterans Affairs Medical Center; Director, National MS Society Multiple Sclerosis Center; Director, Neuropathy Association Center of Excellence, Professor, Department of Neurology and Psychiatry, Associate Professor, Institute for Molecular Virology, St Louis University School of Medicine
Florian P Thomas, MD, MA, PhD, Drmed is a member of the following medical societies: American Academy of Neurology, American Neurological Association, American Paraplegia Society, Consortium of Multiple Sclerosis Centers, National Multiple Sclerosis Society, and Sigma Xi
Disclosure: Nothing to disclose.
Selim R Benbadis, MD Professor, Director of Comprehensive Epilepsy Program, Departments of Neurology and Neurosurgery, Tampa General Hospital, University of South Florida College of Medicine
Selim R Benbadis, MD is a member of the following medical societies: American Academy of Neurology, American Academy of Sleep Medicine, American Clinical Neurophysiology Society, American Epilepsy Society, and American Medical Association
Disclosure: UCB Pharma Honoraria Speaking, consulting; Lundbeck Honoraria Speaking, consulting; Cyberonics Honoraria Speaking, consulting; Glaxo Smith Kline Honoraria Speaking, consulting; Sleepmed/DigiTrace Honoraria Consulting; Sunovion Consulting fee None; Supernus Speaking, consulting; Upsher-Smith Grant/research funds None
Chief Editor
Nicholas Lorenzo, MD, CPE Chairman and CEO, Neurology Specialists and Consultants; Former Senior Vice President, Founding Executive Director, Continuing Medical Education, Gannett Education (Division Gannett Healthcare Group) Nicholas Lorenzo, MD, CPE is a member of the following medical societies: Alpha Omega Alpha, American Academy of Neurology, and American College of Physician Executives
Disclosure: Nothing to disclose.
Additional Contributors
The authors and editors of Medscape Reference gratefully acknowledge the contributions of previous author Marina Zvartau-Hind, MD, PhD, to the development and writing of this article.
References
- Rajabally YA, Simpson BS, Beri S, Bankart J, Gosalakkal JA. Epidemiologic variability of chronic inflammatory demyelinating polyneuropathy with different diagnostic criteria: study of a UK population. Muscle Nerve. Apr 2009;39(4):432-8. [Medline].
- Hughes RA, Donofrio P, Bril V, et al. Intravenous immune globulin (10% caprylate-chromatography purified) for the treatment of chronic inflammatory demyelinating polyradiculoneuropathy (ICE study): a randomised placebo-controlled trial. Lancet Neurol. Feb 2008;7(2):136-44. [Medline].
- Eftimov F, Vermeulen M, van Doorn PA, Brusse E, van Schaik IN. Long-term remission of CIDP after pulsed dexamethasone or short-term prednisolone treatment. Neurology. Apr 3 2012;78(14):1079-84. [Medline].
- Gorson KC, van Schaik IN, Merkies IS, et al. Chronic inflammatory demyelinating polyneuropathy disease activity status: recommendations for clinical research standards and use in clinical practice. J Peripher Nerv Syst. Dec 2010;15(4):326-33. [Medline].
- Barnett MH, Pollard JD, Davies L, McLeod JG. Cyclosporin A in resistant chronic inflammatory demyelinating polyradiculoneuropathy. Muscle Nerve. Apr 1998;21(4):454-60. [Medline].
- Barohn RJ, Kissel JT, Warmolts JR, Mendell JR. Chronic inflammatory demyelinating polyradiculoneuropathy. Clinical characteristics, course, and recommendations for diagnostic criteria. Arch Neurol. Aug 1989;46(8):878-84. [Medline].
- Barohn RJ, Saperstein DS. Guillain-Barré syndrome and chronic inflammatory demyelinating polyneuropathy. Semin Neurol. 1998;18(1):49-61. [Medline].
- Bouchard C, Lacroix C, Plante V, et al. Clinicopathologic findings and prognosis of chronic inflammatory demyelinating polyneuropathy. Neurology. Feb 1999;52(3):498-503. [Medline].
- Bromberg MB. Comparison of electrodiagnostic criteria for primary demyelination in chronic polyneuropathy. Muscle Nerve. Oct 1991;14(10):968-76. [Medline].
- Chassande B, Leger JM, Younes-Chennoufi AB, et al. Peripheral neuropathy associated with IgM monoclonal gammopathy: correlations between M-protein antibody activity and clinical/electrophysiological features in 40 cases. Muscle Nerve. Jan 1998;21(1):55-62. [Medline].
- Chaudhry V. Multifocal motor neuropathy. Semin Neurol. 1998;18(1):73-81. [Medline].
- Dalakas MC, Quarles RH, Farrer RG, et al. A controlled study of intravenous immunoglobulin in demyelinating neuropathy with IgM gammopathy. Ann Neurol. Nov 1996;40(5):792-5. [Medline].
- Donofrio PD. Chronic inflammatory demyelinating polyradiculoneuropathy: new views and guidelines. J Peripher Nerv Syst. Sep 2005;10(3):217-9. [Medline].
- Dyck PJ, Daube J, O'Brien P, et al. Plasma exchange in chronic inflammatory demyelinating polyradiculoneuropathy. N Engl J Med. Feb 20 1986;314(8):461-5. [Medline].
- Dyck PJ, Lais AC, Ohta M, Bastron JA, Okazaki H, Groover RV. Chronic inflammatory polyradiculoneuropathy. Mayo Clin Proc. Nov 1975;50(11):621-37. [Medline].
- Dyck PJ, Litchy WJ, Kratz KM, et al. A plasma exchange versus immune globulin infusion trial in chronic inflammatory demyelinating polyradiculoneuropathy. Ann Neurol. Dec 1994;36(6):838-45. [Medline].
- Erdmann PG, van Meeteren NL, Kalmijn S, Wokke JH, Helders PJ, van den Berg LH. Functional health status of patients with chronic inflammatory neuropathies. J Peripher Nerv Syst. Jun 2005;10(2):181-9. [Medline].
- European Federation of Neurological Societies/Peripheral Nerve Society Guideline on management of chronic inflammatory demyelinating polyradiculoneuropathy. Report of a joint task force of the European Federation of Neurological Societies and the Peripheral Nerve Society. J Peripher Nerv Syst. Sep 2005;10(3):220-8. [Medline].
- Good JL, Chehrenama M, Mayer RF, Koski CL. Pulse cyclophosphamide therapy in chronic inflammatory demyelinating polyneuropathy. Neurology. Dec 1998;51(6):1735-8. [Medline].
- Gorson KC, Allam G, Ropper AH. Chronic inflammatory demyelinating polyneuropathy: clinical features and response to treatment in 67 consecutive patients with and without a monoclonal gammopathy. Neurology. Feb 1997;48(2):321-8. [Medline].
- Hadden RD, Hughes RA. Treatment of immune-mediated inflammatory neuropathies. Curr Opin Neurol. Oct 1999;12(5):573-9. [Medline].
- Hobson-Webb LD, Donofrio PD. Inflammatory neuropathies: an update on evaluation and treatment. Curr Rheumatol Rep. Oct 2005;7(5):348-55. [Medline].
- Jann S, Beretta S, Bramerio MA. Different types of chronic inflammatory demyelinating polyneuropathy have a different clinical course and response to treatment. Muscle Nerve. Sep 2005;32(3):351-6. [Medline].
- Korinthenberg R. Chronic inflammatory demyelinating polyradiculoneuropathy in children and their response to treatment. Neuropediatrics. Aug 1999;30(4):190-6. [Medline].
- Léger JM, Behin A. Multifocal motor neuropathy. Curr Opin Neurol. Oct 2005;18(5):567-73. [Medline].
- Mahattanakul W, Crawford TO, Griffin JW, Goldstein JM, Cornblath DR. Treatment of chronic inflammatory demyelinating polyneuropathy with cyclosporin-A. J Neurol Neurosurg Psychiatry. Feb 1996;60(2):185-7. [Medline]. [Full Text].
- Markvardsen LH, Debost JC, Harbo T, Sindrup SH, Andersen H, Christiansen I, et al. Subcutaneous immunoglobulin in responders to intravenous therapy with chronic inflammatory demyelinating polyradiculoneuropathy. Eur J Neurol. Jan 7 2013;[Medline].
- Mendell JR, Barohn RJ, Freimer ML, et al. Randomized controlled trial of IVIg in untreated chronic inflammatory demyelinating polyradiculoneuropathy. Neurology. Feb 27 2001;56(4):445-9. [Medline].
- Notermans NC, Franssen H, Eurelings M, Van der Graaf Y, Wokke JH. Diagnostic criteria for demyelinating polyneuropathy associated with monoclonal gammopathy. Muscle Nerve. Jan 2000;23(1):73-9. [Medline].
- Rotta FT, Sussman AT, Bradley WG, Ram Ayyar D, Sharma KR, Shebert RT. The spectrum of chronic inflammatory demyelinating polyneuropathy. J Neurol Sci. Feb 15 2000;173(2):129-39. [Medline].
- Saperstein DS, Amato AA, Wolfe GI, et al. Multifocal acquired demyelinating sensory and motor neuropathy: the Lewis-Sumner syndrome. Muscle Nerve. May 1999;22(5):560-6. [Medline].
- Saperstein DS, Katz JS, Amato AA, Barohn RJ. Clinical spectrum of chronic acquired demyelinating polyneuropathies. Muscle Nerve. Mar 2001;24(3):311-24. [Medline].
- Stamboulis E, Katsaros N, Koutsis G, Iakovidou H, Giannakopoulou A, Simintzi I. Clinical and subclinical autonomic dysfunction in chronic inflammatory demyelinating polyradiculoneuropathy. Muscle Nerve. Jan 2006;33(1):78-84. [Medline].
- Uncini A, De Angelis MV, Di Muzio A, et al. Chronic inflammatory demyelinating polyneuropathy in diabetics: motor conductions are important in the differential diagnosis with diabetic polyneuropathy. Clin Neurophysiol. Apr 1999;110(4):705-11. [Medline].
- Visudtibhan A, Chiemchanya S, Visudhiphan P. Cyclosporine in chronic inflammatory demyelinating polyradiculoneuropathy. Pediatr Neurol. Nov 2005;33(5):368-72. [Medline].
Electromyography of a patient with chronic inflammatory demyelinating polyradiculoneuropathy illustrating conduction block, temporal dispersion of compound muscle action potential, prolonged distal latencies, and slowed conduction.
Prolonged F wave latencies (normal is < 31).
Electron micrograph of the peripheral nerve of a patient with chronic inflammatory demyelinating polyradiculoneuropathy. Note "onion bulb" formation in the myelin sheath of the nerve fibers due to continuous demyelination and remyelination. Courtesy of A. Sima, MD, Department of Pathology, Wayne State University.
Read more about Chronic Inflammatory Demyelinating Polyradiculoneuropathy on Medscape
Atlas C-1 Twisted causing PCS symptoms
Atlas C-1 Twisted Causing PCS Symptoms
 |
Thread Tools
 |
Display Modes

|
|
|
|
|
|
|
|
Subscribe to:
Posts (Atom)








Hope your future news is a good, I'll keep my figers crossed too!
Rosina x
I hope that your lesions will go away when you are off the treatment. Your first neuro probably didnt realise that your treatment can cause lesions and MS symptoms.
I hope all goes well
Moyna xx
I hope that what I have been through is remembered for people in the future so they don't have to go through this. This is all presuming that the Humira has caused this in the first place.xx
All the best and keep us posted. xx
I notice you say you've been on Humira for six years. As the consultant been monitoring you over the last six years, while you've been taking the drug, given that he will be aware that demyelination can be caused by this drug. Were you made aware of the side efects before agreeing to take it?
Noreen xx
the Neuro researched the drug and didn't say much at all. He saw my condition and results of reflexes are odd so pressed on testing. So all in all I'm just waiting to see if I improve after I've come off the drug and got over the withdrawal. I've got a backup treatment of steroids in the cupboard if the Crohns flares when I come off it and there's a new drug out if I need it. When I was recommended the Humira I had to sign a form but I cannot remember how nasty they said the side effects were, the state I was in I would have tried anything :s
the MRI (according to the doc) said no presence of demyelination , just lesions from what he could see. He did say he was no expert on brain things but it was brilliant news nonetheless . Xxx
i hope you are all alright and coping with the warm spell we are having, though as I'm looking out the window it looks like rain...plants won't need watering ;)
thanks again
xxxxxx