The CCSVI procedure was originally thought to work via expanding a narrowed jugular vein, thus restoring proper flow of blood in the veins draining the central nervous system, but researchers have been unable reproduce these results in subsequent studies, calling the entire CCSVI as a cause of MS theory into question, and to date, there is still no conclusive evidence that CCSVI is a cause of MS, or even that it is a symptomatic condition in its own right.
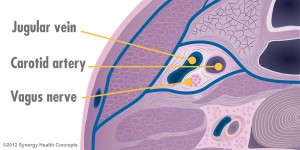 However, while the debate over CCSVI and MS continues, new data suggests that Dr. Zamboni may have gotten it right in looking at the veins for treatment, but it might not be venous abnormalities that are the real problem, with a team of California-based researchers contending that it is the nerves surrounding the veins not the veins themselves that are being treated by ballooning, with expansion of the jugular vein leading to stimulation of the autonomic nerve fibers, which run alongside the jugular and are responsible for communication between the brain and the central nervous system. They say that ongoing research and a growing body of clinical data strongly indicate that Dr. Zamboni’s CCSVI procedure may be the first viable treatment for an even more pervasive problem — dysautonomia — which is seen not only in almost all MS patients but also in patients diagnosed with a long list of other diseases and conditions. As a result, they believe the CCSVI procedure is better described by the term TVAM (Transvascular Autonomic Modulation).
However, while the debate over CCSVI and MS continues, new data suggests that Dr. Zamboni may have gotten it right in looking at the veins for treatment, but it might not be venous abnormalities that are the real problem, with a team of California-based researchers contending that it is the nerves surrounding the veins not the veins themselves that are being treated by ballooning, with expansion of the jugular vein leading to stimulation of the autonomic nerve fibers, which run alongside the jugular and are responsible for communication between the brain and the central nervous system. They say that ongoing research and a growing body of clinical data strongly indicate that Dr. Zamboni’s CCSVI procedure may be the first viable treatment for an even more pervasive problem — dysautonomia — which is seen not only in almost all MS patients but also in patients diagnosed with a long list of other diseases and conditions. As a result, they believe the CCSVI procedure is better described by the term TVAM (Transvascular Autonomic Modulation). The new study, published in the June, 2014 edition of the Journal of Endovascular sheds light on the positive effect of CCSVI on the sympathetic nervous system, explaining how researchers were able to pinpoint how the procedure improved abnormal sympathetic function found in patients with many chronic conditions including Multiple Sclerosis.
The new study, published in the June, 2014 edition of the Journal of Endovascular sheds light on the positive effect of CCSVI on the sympathetic nervous system, explaining how researchers were able to pinpoint how the procedure improved abnormal sympathetic function found in patients with many chronic conditions including Multiple Sclerosis.Titled “Transvascular Autonomic Modulation: A Modified Balloon Angioplasty Technique for the Treatment of Autonomic Dysfunction in Multiple Sclerosis Patients” (Journal of Endovascular Therapy: June 2014, Vol. 21, No. 3, pp. 417-428), the study coauthored by Newport Beach, California based Interventional Radiologist, Michael Arata, MD, and his research associate, Zohara Sternberg, PhD, compares the efficacy of the TVAM procedure vs. traditional balloon angioplasty in improving cardiovascular autonomic nervous system (ANS) dysfunction in Multiple Sclerosis (MS) patients. Drs. Arata and Sternberg report that they found using an angioplasty balloon to stimulate vein-associated nerves increased sympathetic activity shows promise for patients who suffer from MS.
They note that twenty-one MS patients (11 men; mean age 48.713.0 years) who presented with symptoms of cardiovascular ANS dysfunction underwent TVAM and were compared with age/sex-matched MS patients (10 men; 49.311.1 years) in the same stages of the disease who presented with chronic cerebrospinal venous insufficiency (CCSVI) and who underwent venous balloon angioplasty.
The coauthors observe that in this instance, TVAM involved the coupling of balloon angioplasty of the internal jugular veins with application of external manual compression and dilation of the azygos and renal veins; unlike traditional angioplasty for CCSVI, which treats only abnormal veins (50% stenosis or static valve), all targeted vessels were treated with TVAM regardless of the presence of an abnormality. The effect of TVAM on ANS function was indicated by determining heart rate variability based on the electrocardiographic R-R interval lengths using vector analysis to derive the mean circular resultant (MCR) and the expiration/inspiration (E/I) ratio, the Valsalva ratio, and the 30:15 postural ratio at 24 hours after intervention.
They found that left renal vein compression was common among the TVAM patients and resulted in 50% luminal compromise in 10 of 21 patients. A, and overall, 18 patients met the diagnostic criteria for CCSVI with at least one lesion >50%, but only 10 lesions were considered treatable by traditional balloon angioplasty. After intervention, they report that R-R interval values, including the 30:15 postural ratio (p=0.01), the MCR (p=0.1), and E/I ratio (p=0.1), were higher for the TVAM patients compared to the control group, and the safety profile of the TVAM procedure was similar to that of traditional balloon angioplasty.
Drs. Arata and Sternberg conclude that the combination of balloon angioplasty of anatomically normal veins coupled with external compression during dilation of these veins can improve indicators of ANS dysfunction, reporting that the safety and efficacy of TVAM in MS patients observed in this pilot study is encouraging, paving the way for the treatment of dysautonomia in pathological states other than MS.
However, they caution that the long-term effects of cerebral venous distension are currently unknown, and one cannot exclude the possibility that the increase in vagal activity post angioplasty may further disturb the autonomic balance in selected MS patients who initially present with reduced sympathetic ANS function, and additional study and replication of these results are required.
 A graduate of UCSF School of Medicine, Dr. Arata has spent more than a decade performing angioplasty and has been at the forefront of research for CCSVI. “There is a possibility that improved autonomic function may diminish symptoms and have an impact on the course of the disease,” comments Dr. Arata, who serves as Medical Director at Synergy Health Concepts in Newport Beach. He is the most experienced CCSVI physician in the United States having performed more than 2000 procedures on patients with autonomic-associated disease, claiming a high clinical (patient response) success rate in excess of 90% in a recent study group.
A graduate of UCSF School of Medicine, Dr. Arata has spent more than a decade performing angioplasty and has been at the forefront of research for CCSVI. “There is a possibility that improved autonomic function may diminish symptoms and have an impact on the course of the disease,” comments Dr. Arata, who serves as Medical Director at Synergy Health Concepts in Newport Beach. He is the most experienced CCSVI physician in the United States having performed more than 2000 procedures on patients with autonomic-associated disease, claiming a high clinical (patient response) success rate in excess of 90% in a recent study group.“The current study demonstrates the procedure’s effect on autonomic function, offering an explanation for why patients may see symptom improvement with venous ballooning even though separate studies have failed to show a relationship between venous obstruction and Multiple Sclerosis. The mechanism of symptom improvement is improved autonomic tone rather than relief of flow obstruction,” says Dr. Arata.

Synergy Health Concepts, located in Newport Beach, CA, is a state-of-the-art medical center for CCSVI diagnosis and treatment, fully equipped with four patient examination rooms, three procedure rooms, and seven pre-procedural and post-procedural recovery suites. SHC’s state-of-the-art 3 Tesla MRI and ultrasound machines enable the clinicians to obtain the best imaging possible for patients, and SNC claims to be the only practice using autonomic testing as a core component of the diagnostic evaluation.
SHC reports maintaining a a 99 percent technical success rate in more than 2000 procedures performed, and a clinical (patient response) success rate in excess of 90%, and that in patients showing autonomic symptoms who test positive for autonomic dysfunction who are approved for the procedure, symptom relief begins during and directly after the procedure, and is durable in excess of 2 years for more than 75% of patients.
The CCSVI procedure (TVAM) is performed on an outpatient basis at Synergy Health’s state-of-the-art medical center. The patient will receive conscious sedation to maintain comfort throughout the procedure, and the procedure will typically take under an hour to perform. The primary treatment is an endovascular procedure in which a catheter is inserted via a small incision and threaded up into the jugular vein. A balloon is then inflated via the catheter, expanding the jugular vein in much the same way that coronary angioplasty expands narrowed arteries of the heart.
SVI says the majority of their patients (about 75 percent) have a durable response, some lasting over three years and beyond with no degradation or relapse, and this cohort is able to maintain benefits of the procedure seen from day one. However, the remaining 25 percent of patients don’t respond to treatment as well, with about 10 percent experiencing no benefits at all post procedure.
No comments:
Post a Comment