Chronic Inflammatory Demyelinating Polyradiculoneuropathy
- Author: Richard A Lewis, MD; Chief Editor: Nicholas Lorenzo, MD, CPE more...
Practice Essentials
The term chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) has been used to identify patients with a chronically progressive or relapsing symmetric sensorimotor disorder with cytoalbuminologic dissociation and interstitial and perivascular endoneurial infiltration by lymphocytes and macrophages. It can be considered the chronic equivalent of acute inflammatory demyelinating polyradiculoneuropathy, the most common form of Guillain-Barré syndrome.
Symptoms reported include the following:
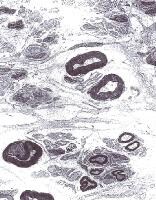 Electron micrograph of the peripheral nerve of a patient with chronic inflammatory demyelinating polyradiculoneuropathy. Note "onion bulb" formation in the myelin sheath of the nerve fibers due to continuous demyelination and remyelination. Courtesy of A. Sima, MD, Department of Pathology, Wayne State University.
Electron micrograph of the peripheral nerve of a patient with chronic inflammatory demyelinating polyradiculoneuropathy. Note "onion bulb" formation in the myelin sheath of the nerve fibers due to continuous demyelination and remyelination. Courtesy of A. Sima, MD, Department of Pathology, Wayne State University.
Signs and symptoms
CIDP typically starts insidiously and evolves slowly, in either a slowly progressive or a relapsing manner, with partial or complete recovery between recurrences; periods of worsening and improvement usually last weeks or months. Most experts consider the necessary duration of symptoms to be greater than 8 weeks for the diagnosis of CIDP to be made.Symptoms reported include the following:
- Preceding infection (infrequent)
- Initial limb weakness, both proximal and distal
- Sensory symptoms (eg, tingling and numbness of hands and feet)
- Motor symptoms (usually predominant)
- In about 16% of patients, a relatively acute or subacute onset of symptoms
- In children, usually a more precipitous onset of symptoms
- Symptoms of autonomic system dysfunction (eg, orthostatic dizziness)
- Signs of cranial nerve (CN) involvement (eg, facial muscle paralysis or diplopia)
- Gait abnormalities
- Motor deficits (eg, symmetric weakness of both proximal and distal muscles in upper and lower extremities)
- Diminished or absent deep tendon reflexes
- Sensory deficits (typically in stocking-glove distribution)
- Impaired coordination
Diagnosis
Laboratory studies that may be helpful include the following:- Cerebrospinal fluid analysis: Elevated protein levels are common (80% of patients); 10% of patients also have mild lymphocytic pleocytosis and increased gamma globulin
- Complete blood count (CBC), erythrocyte sedimentation rate (ESR), antinuclear antibody (ANA) level, biochemistry profile, and serum and urine immunoelectrophoresis (to exclude associated systemic disorders)
- In certain instances, genetic testing
- MRI of the spine with gadolinium enhancement
- Electromyography (EMG) is a critical test to determine whether the disorder is truly a peripheral neuropathy and whether the neuropathy is demyelinating
- Peripheral (sural) nerve biopsy: This is considered when the diagnosis is not completely clear, when other causes cannot be excluded, or when profound axonal involvement is observed on EMG; biopsy was once commonly recommended for most patients before immunosuppressive therapy, but current guidelines no longer recommend it
Management
Principles of treatment are as follows:- CIDP must be treated to prevent accumulating disability that necessitates physical and occupational therapy, orthotic devices, and long-term treatment
- Close follow-up care is necessary to adjust treatment
- Surgical and orthopedic consultation may be required for sural nerve biopsy or in severe disease with joint deformities
- Consultation with a neurologist is warranted
- Consultation with a physical medicine and rehabilitation specialist is appropriate for physical and occupational therapy and evaluation for orthotic devices
- Other consultations may be necessary if associated diseases are present
- Physical therapy and an active lifestyle should be encouraged
Image library
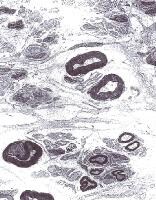 Electron micrograph of the peripheral nerve of a patient with chronic inflammatory demyelinating polyradiculoneuropathy. Note "onion bulb" formation in the myelin sheath of the nerve fibers due to continuous demyelination and remyelination. Courtesy of A. Sima, MD, Department of Pathology, Wayne State University.
Electron micrograph of the peripheral nerve of a patient with chronic inflammatory demyelinating polyradiculoneuropathy. Note "onion bulb" formation in the myelin sheath of the nerve fibers due to continuous demyelination and remyelination. Courtesy of A. Sima, MD, Department of Pathology, Wayne State University. Background
Chronic inflammatory demyelinating polyradiculoneuropathy is presumed to occur because of immunologic antibody-mediated reaction along with interstitial and perivascular infiltration of the endoneurium with inflammatory T cells and macrophages. The consequence is a segmental demyelination of peripheral nerves.
Human leukocyte antigens Dw3, DRw3, A1, and B8 occur more frequently in patients with CIDP than in the healthy population.
Cytoalbuminologic dissociation is a characteristic finding in cerebrospinal fluid (CSF) pointing to nerve root involvement. Occasionally, CSF studies reveal mild lymphocytic pleocytosis and elevation of gamma globulin level, but this is observed most frequently in HIV-positive patients.
The term chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) has been used to identify patients with a chronically progressive or relapsing symmetric sensorimotor disorder with cytoalbuminologic dissociation and interstitial and perivascular endoneurial infiltration by lymphocytes and macrophages. In many ways, CIDP can be considered the chronic equivalent of acute inflammatory demyelinating polyradiculoneuropathy (AIDP), the most common form of Guillain-Barré syndrome (GBS).
A number of variants of CIDP have been described that have immune or inflammatory aspects and electrophysiologic and/or pathologic evidence of demyelination in common. No consensus exists on the best approach to the nomenclature of these disorders. CIDP is a major subset of chronic acquired demyelinating polyneuropathies (CADP). In this context, CIDP is considered when patients have a symmetric proximal and distal motor predominant disorder.
CIDP variants include patients with predominantly sensory symptoms, those with a distal symmetric disorder (DADS), those with multifocal sensorimotor neuropathy or sensorimotor mononeuropathy multiplex with prominent conduction block (also known as Lewis-Sumner neuropathy), and those with CIDP with associated CNS demyelination or with other systemic disorders.
The following disorders are considered distinct from CIDP because they have specific pathophysiologic features and respond to treatments differently than do patients with CIDP: Demyelinating neuropathies associated with immunoglobulin M (IgM) paraproteins, including those with anti–myelin-associated glycoprotein (MAG) antibodies; polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, and skin changes (POEMS) syndrome; and multifocal motor neuropathy.
Human leukocyte antigens Dw3, DRw3, A1, and B8 occur more frequently in patients with CIDP than in the healthy population.
Cytoalbuminologic dissociation is a characteristic finding in cerebrospinal fluid (CSF) pointing to nerve root involvement. Occasionally, CSF studies reveal mild lymphocytic pleocytosis and elevation of gamma globulin level, but this is observed most frequently in HIV-positive patients.
The term chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) has been used to identify patients with a chronically progressive or relapsing symmetric sensorimotor disorder with cytoalbuminologic dissociation and interstitial and perivascular endoneurial infiltration by lymphocytes and macrophages. In many ways, CIDP can be considered the chronic equivalent of acute inflammatory demyelinating polyradiculoneuropathy (AIDP), the most common form of Guillain-Barré syndrome (GBS).
A number of variants of CIDP have been described that have immune or inflammatory aspects and electrophysiologic and/or pathologic evidence of demyelination in common. No consensus exists on the best approach to the nomenclature of these disorders. CIDP is a major subset of chronic acquired demyelinating polyneuropathies (CADP). In this context, CIDP is considered when patients have a symmetric proximal and distal motor predominant disorder.
CIDP variants include patients with predominantly sensory symptoms, those with a distal symmetric disorder (DADS), those with multifocal sensorimotor neuropathy or sensorimotor mononeuropathy multiplex with prominent conduction block (also known as Lewis-Sumner neuropathy), and those with CIDP with associated CNS demyelination or with other systemic disorders.
The following disorders are considered distinct from CIDP because they have specific pathophysiologic features and respond to treatments differently than do patients with CIDP: Demyelinating neuropathies associated with immunoglobulin M (IgM) paraproteins, including those with anti–myelin-associated glycoprotein (MAG) antibodies; polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, and skin changes (POEMS) syndrome; and multifocal motor neuropathy.
Pathophysiology
Chronic inflammatory demyelinating polyradiculoneuropathy is presumed to occur because of immunologic antibody-mediated reaction along with interstitial and perivascular infiltration of the endoneurium with inflammatory T cells and macrophages. The consequence is a segmental demyelination of peripheral nerves.
Human leukocyte antigens Dw3, DRw3, A1, and B8 occur more frequently in patients with CIDP than in the healthy population.
Cytoalbuminologic dissociation is a characteristic finding in cerebrospinal fluid (CSF) pointing to nerve root involvement. Occasionally, CSF studies reveal mild lymphocytic pleocytosis and elevation of gamma globulin level, but this is observed most frequently in HIV-positive patients.
Human leukocyte antigens Dw3, DRw3, A1, and B8 occur more frequently in patients with CIDP than in the healthy population.
Cytoalbuminologic dissociation is a characteristic finding in cerebrospinal fluid (CSF) pointing to nerve root involvement. Occasionally, CSF studies reveal mild lymphocytic pleocytosis and elevation of gamma globulin level, but this is observed most frequently in HIV-positive patients.
Frequency
International
CIDP is uncommon. The estimated prevalence of CIDP in populations from the UK, Australia, Italy, Norway, and Japan is 0.8-7.7 per 100,000. A 2009 study showed that the incidence and prevalence is variable depending on diagnostic criteria. In Rutland, UK on May 1, 2008, the prevalence of CIDP was 4.77/100,000 if the EFNS/PNS criteria were used but only 1.97 per 100,000 if the AAN criteria were used. Similarly the annual incidence was 0.7 per 100,000 using the EFNS criteria and 0.35 using the AAN criteria.[1]Mortality/Morbidity
Chronic inflammatory demyelinating polyradiculoneuropathy most commonly has an insidious onset and either chronic progressive or relapsing course. Occasionally, complete remissions occur. Quadriplegia, respiratory failure, and death have been described but are rare.
Race
No racial predilection has been identified.Sex
Both sexes are affected. Of CADP variants, multifocal motor neuropathy has a male predominance of at least 2:1 based on a survey of the largest case series.Age
Chronic inflammatory demyelinating polyradiculoneuropathy may occur at any age, but it is more common in the fifth and sixth decades. Relapsing course is associated with younger age of patients (third and fourth decades). CIDP has been described in childhood.
Previous
Proceed to Clinical Presentation
Contributor Information and Disclosures
Author
Richard A Lewis, MD Professor and Associate Chairman of Neurology, Department of Neurology, Wayne State University School of Medicine Richard A Lewis, MD is a member of the following medical societies: American Academy of Neurology, American Association of Neuromuscular and Electrodiagnostic Medicine, American Neurological Association, and Peripheral Nerve Society
Disclosure: GBS/CIDP FI Grant/research funds Other; Baxter Consulting fee Consulting; Baxter Grant/research funds None; CSL Behring Consulting fee Consulting
Specialty Editor Board
Dianna Quan, MD Professor of Neurology, Director, Electromyography Laboratory, University of Colorado School of Medicine Dianna Quan, MD is a member of the following medical societies: American Academy of Neurology, American Association of Neuromuscular and Electrodiagnostic Medicine, and Phi Beta Kappa
Disclosure: e-medicine Honoraria Other; Pfizer Grant/research funds Independent contractor; Alnylam Grant/research funds Independent contractor
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference
Disclosure: Medscape Salary Employment
Florian P Thomas, MD, MA, PhD, Drmed Director, Regional MS Center of Excellence, St Louis Veterans Affairs Medical Center; Director, National MS Society Multiple Sclerosis Center; Director, Neuropathy Association Center of Excellence, Professor, Department of Neurology and Psychiatry, Associate Professor, Institute for Molecular Virology, St Louis University School of Medicine
Florian P Thomas, MD, MA, PhD, Drmed is a member of the following medical societies: American Academy of Neurology, American Neurological Association, American Paraplegia Society, Consortium of Multiple Sclerosis Centers, National Multiple Sclerosis Society, and Sigma Xi
Disclosure: Nothing to disclose.
Selim R Benbadis, MD Professor, Director of Comprehensive Epilepsy Program, Departments of Neurology and Neurosurgery, Tampa General Hospital, University of South Florida College of Medicine
Selim R Benbadis, MD is a member of the following medical societies: American Academy of Neurology, American Academy of Sleep Medicine, American Clinical Neurophysiology Society, American Epilepsy Society, and American Medical Association
Disclosure: UCB Pharma Honoraria Speaking, consulting; Lundbeck Honoraria Speaking, consulting; Cyberonics Honoraria Speaking, consulting; Glaxo Smith Kline Honoraria Speaking, consulting; Sleepmed/DigiTrace Honoraria Consulting; Sunovion Consulting fee None; Supernus Speaking, consulting; Upsher-Smith Grant/research funds None
Chief Editor
Nicholas Lorenzo, MD, CPE Chairman and CEO, Neurology Specialists and Consultants; Former Senior Vice President, Founding Executive Director, Continuing Medical Education, Gannett Education (Division Gannett Healthcare Group) Nicholas Lorenzo, MD, CPE is a member of the following medical societies: Alpha Omega Alpha, American Academy of Neurology, and American College of Physician Executives
Disclosure: Nothing to disclose.
Additional Contributors
The authors and editors of Medscape Reference gratefully acknowledge the contributions of previous author Marina Zvartau-Hind, MD, PhD, to the development and writing of this article.
References
- Rajabally YA, Simpson BS, Beri S, Bankart J, Gosalakkal JA. Epidemiologic variability of chronic inflammatory demyelinating polyneuropathy with different diagnostic criteria: study of a UK population. Muscle Nerve. Apr 2009;39(4):432-8. [Medline].
- Hughes RA, Donofrio P, Bril V, et al. Intravenous immune globulin (10% caprylate-chromatography purified) for the treatment of chronic inflammatory demyelinating polyradiculoneuropathy (ICE study): a randomised placebo-controlled trial. Lancet Neurol. Feb 2008;7(2):136-44. [Medline].
- Eftimov F, Vermeulen M, van Doorn PA, Brusse E, van Schaik IN. Long-term remission of CIDP after pulsed dexamethasone or short-term prednisolone treatment. Neurology. Apr 3 2012;78(14):1079-84. [Medline].
- Gorson KC, van Schaik IN, Merkies IS, et al. Chronic inflammatory demyelinating polyneuropathy disease activity status: recommendations for clinical research standards and use in clinical practice. J Peripher Nerv Syst. Dec 2010;15(4):326-33. [Medline].
- Barnett MH, Pollard JD, Davies L, McLeod JG. Cyclosporin A in resistant chronic inflammatory demyelinating polyradiculoneuropathy. Muscle Nerve. Apr 1998;21(4):454-60. [Medline].
- Barohn RJ, Kissel JT, Warmolts JR, Mendell JR. Chronic inflammatory demyelinating polyradiculoneuropathy. Clinical characteristics, course, and recommendations for diagnostic criteria. Arch Neurol. Aug 1989;46(8):878-84. [Medline].
- Barohn RJ, Saperstein DS. Guillain-Barré syndrome and chronic inflammatory demyelinating polyneuropathy. Semin Neurol. 1998;18(1):49-61. [Medline].
- Bouchard C, Lacroix C, Plante V, et al. Clinicopathologic findings and prognosis of chronic inflammatory demyelinating polyneuropathy. Neurology. Feb 1999;52(3):498-503. [Medline].
- Bromberg MB. Comparison of electrodiagnostic criteria for primary demyelination in chronic polyneuropathy. Muscle Nerve. Oct 1991;14(10):968-76. [Medline].
- Chassande B, Leger JM, Younes-Chennoufi AB, et al. Peripheral neuropathy associated with IgM monoclonal gammopathy: correlations between M-protein antibody activity and clinical/electrophysiological features in 40 cases. Muscle Nerve. Jan 1998;21(1):55-62. [Medline].
- Chaudhry V. Multifocal motor neuropathy. Semin Neurol. 1998;18(1):73-81. [Medline].
- Dalakas MC, Quarles RH, Farrer RG, et al. A controlled study of intravenous immunoglobulin in demyelinating neuropathy with IgM gammopathy. Ann Neurol. Nov 1996;40(5):792-5. [Medline].
- Donofrio PD. Chronic inflammatory demyelinating polyradiculoneuropathy: new views and guidelines. J Peripher Nerv Syst. Sep 2005;10(3):217-9. [Medline].
- Dyck PJ, Daube J, O'Brien P, et al. Plasma exchange in chronic inflammatory demyelinating polyradiculoneuropathy. N Engl J Med. Feb 20 1986;314(8):461-5. [Medline].
- Dyck PJ, Lais AC, Ohta M, Bastron JA, Okazaki H, Groover RV. Chronic inflammatory polyradiculoneuropathy. Mayo Clin Proc. Nov 1975;50(11):621-37. [Medline].
- Dyck PJ, Litchy WJ, Kratz KM, et al. A plasma exchange versus immune globulin infusion trial in chronic inflammatory demyelinating polyradiculoneuropathy. Ann Neurol. Dec 1994;36(6):838-45. [Medline].
- Erdmann PG, van Meeteren NL, Kalmijn S, Wokke JH, Helders PJ, van den Berg LH. Functional health status of patients with chronic inflammatory neuropathies. J Peripher Nerv Syst. Jun 2005;10(2):181-9. [Medline].
- European Federation of Neurological Societies/Peripheral Nerve Society Guideline on management of chronic inflammatory demyelinating polyradiculoneuropathy. Report of a joint task force of the European Federation of Neurological Societies and the Peripheral Nerve Society. J Peripher Nerv Syst. Sep 2005;10(3):220-8. [Medline].
- Good JL, Chehrenama M, Mayer RF, Koski CL. Pulse cyclophosphamide therapy in chronic inflammatory demyelinating polyneuropathy. Neurology. Dec 1998;51(6):1735-8. [Medline].
- Gorson KC, Allam G, Ropper AH. Chronic inflammatory demyelinating polyneuropathy: clinical features and response to treatment in 67 consecutive patients with and without a monoclonal gammopathy. Neurology. Feb 1997;48(2):321-8. [Medline].
- Hadden RD, Hughes RA. Treatment of immune-mediated inflammatory neuropathies. Curr Opin Neurol. Oct 1999;12(5):573-9. [Medline].
- Hobson-Webb LD, Donofrio PD. Inflammatory neuropathies: an update on evaluation and treatment. Curr Rheumatol Rep. Oct 2005;7(5):348-55. [Medline].
- Jann S, Beretta S, Bramerio MA. Different types of chronic inflammatory demyelinating polyneuropathy have a different clinical course and response to treatment. Muscle Nerve. Sep 2005;32(3):351-6. [Medline].
- Korinthenberg R. Chronic inflammatory demyelinating polyradiculoneuropathy in children and their response to treatment. Neuropediatrics. Aug 1999;30(4):190-6. [Medline].
- Léger JM, Behin A. Multifocal motor neuropathy. Curr Opin Neurol. Oct 2005;18(5):567-73. [Medline].
- Mahattanakul W, Crawford TO, Griffin JW, Goldstein JM, Cornblath DR. Treatment of chronic inflammatory demyelinating polyneuropathy with cyclosporin-A. J Neurol Neurosurg Psychiatry. Feb 1996;60(2):185-7. [Medline]. [Full Text].
- Markvardsen LH, Debost JC, Harbo T, Sindrup SH, Andersen H, Christiansen I, et al. Subcutaneous immunoglobulin in responders to intravenous therapy with chronic inflammatory demyelinating polyradiculoneuropathy. Eur J Neurol. Jan 7 2013;[Medline].
- Mendell JR, Barohn RJ, Freimer ML, et al. Randomized controlled trial of IVIg in untreated chronic inflammatory demyelinating polyradiculoneuropathy. Neurology. Feb 27 2001;56(4):445-9. [Medline].
- Notermans NC, Franssen H, Eurelings M, Van der Graaf Y, Wokke JH. Diagnostic criteria for demyelinating polyneuropathy associated with monoclonal gammopathy. Muscle Nerve. Jan 2000;23(1):73-9. [Medline].
- Rotta FT, Sussman AT, Bradley WG, Ram Ayyar D, Sharma KR, Shebert RT. The spectrum of chronic inflammatory demyelinating polyneuropathy. J Neurol Sci. Feb 15 2000;173(2):129-39. [Medline].
- Saperstein DS, Amato AA, Wolfe GI, et al. Multifocal acquired demyelinating sensory and motor neuropathy: the Lewis-Sumner syndrome. Muscle Nerve. May 1999;22(5):560-6. [Medline].
- Saperstein DS, Katz JS, Amato AA, Barohn RJ. Clinical spectrum of chronic acquired demyelinating polyneuropathies. Muscle Nerve. Mar 2001;24(3):311-24. [Medline].
- Stamboulis E, Katsaros N, Koutsis G, Iakovidou H, Giannakopoulou A, Simintzi I. Clinical and subclinical autonomic dysfunction in chronic inflammatory demyelinating polyradiculoneuropathy. Muscle Nerve. Jan 2006;33(1):78-84. [Medline].
- Uncini A, De Angelis MV, Di Muzio A, et al. Chronic inflammatory demyelinating polyneuropathy in diabetics: motor conductions are important in the differential diagnosis with diabetic polyneuropathy. Clin Neurophysiol. Apr 1999;110(4):705-11. [Medline].
- Visudtibhan A, Chiemchanya S, Visudhiphan P. Cyclosporine in chronic inflammatory demyelinating polyradiculoneuropathy. Pediatr Neurol. Nov 2005;33(5):368-72. [Medline].
Electromyography of a patient with chronic inflammatory demyelinating polyradiculoneuropathy illustrating conduction block, temporal dispersion of compound muscle action potential, prolonged distal latencies, and slowed conduction.
Prolonged F wave latencies (normal is < 31).
Electron micrograph of the peripheral nerve of a patient with chronic inflammatory demyelinating polyradiculoneuropathy. Note "onion bulb" formation in the myelin sheath of the nerve fibers due to continuous demyelination and remyelination. Courtesy of A. Sima, MD, Department of Pathology, Wayne State University.


No comments:
Post a Comment