Alzheimer's, Parkinson's and Multiple Sclerosis
Getting to the Root Causes of Neurodegnerative Diseases

CSF Currents, Winds and Tides
 In 1925 the famous neurosurgeon Dr. Harvey Cushing published one of his lectures in Lancet in which he described cerebrospinal fluid (CSF) as the third circulatory system of the brain. The dynamic flow of the third circulatory system of the brain and cord can be compared to a current that comes out of large lakes and rivers fed by rainfall and streams and connected by a gulf to a much larger ocean. Winds whip up the water and the currents and tides collide in the gulf, which results in waves.
In 1925 the famous neurosurgeon Dr. Harvey Cushing published one of his lectures in Lancet in which he described cerebrospinal fluid (CSF) as the third circulatory system of the brain. The dynamic flow of the third circulatory system of the brain and cord can be compared to a current that comes out of large lakes and rivers fed by rainfall and streams and connected by a gulf to a much larger ocean. Winds whip up the water and the currents and tides collide in the gulf, which results in waves.The sketch above on the right shows the Great Lakes of North America where rain water gathers from surrounding hills and streams. The water is carried by currents that flow out of the lakes by way of the Saint Lawrence River where it enters the Saint Lawrence Gulf, which is continuous with the ocean. Compared to the vast Atlantic Ocean, all the Great Lakes combined are much smaller in size and capacity.
While the current flows out of the Great Lakes to the ocean the tide of the ocean it runs into varies with the moon and time of day. Sometimes it moves out to sea in the same direction as the flow of the Saint Lawrence. Othertimes the tide comes in and flows against the river’s current. This creates conflict and turbulance where the two meet in the gulf. Over time the water turbulance caused by the ebb and flow of the tide erodes the coasts of Northern America and helps shape its shorelines.
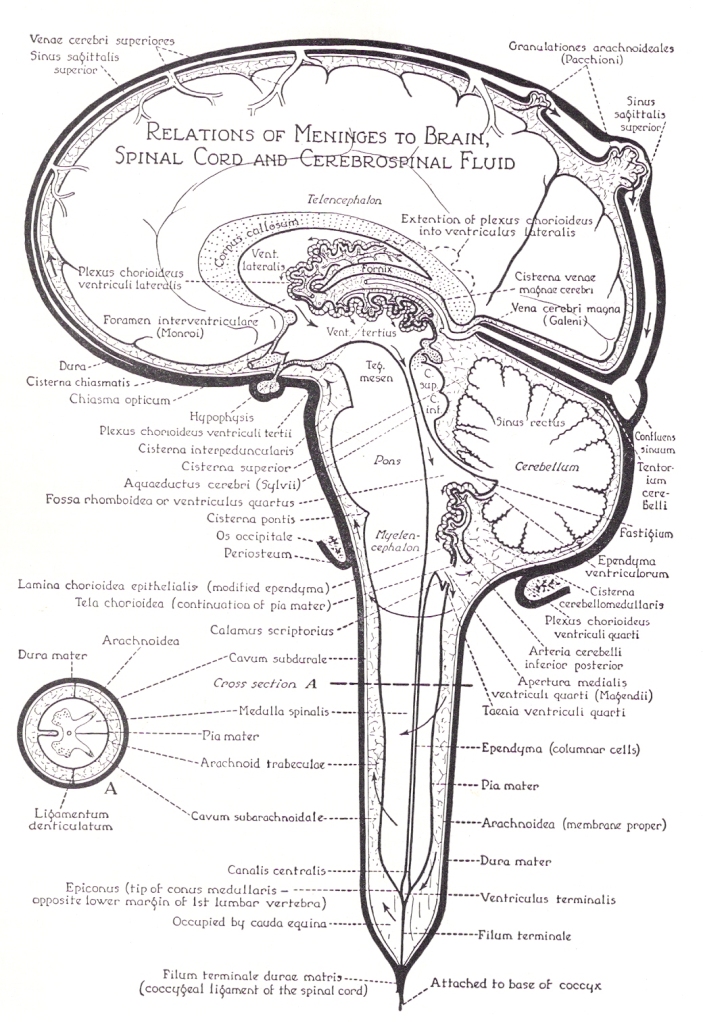
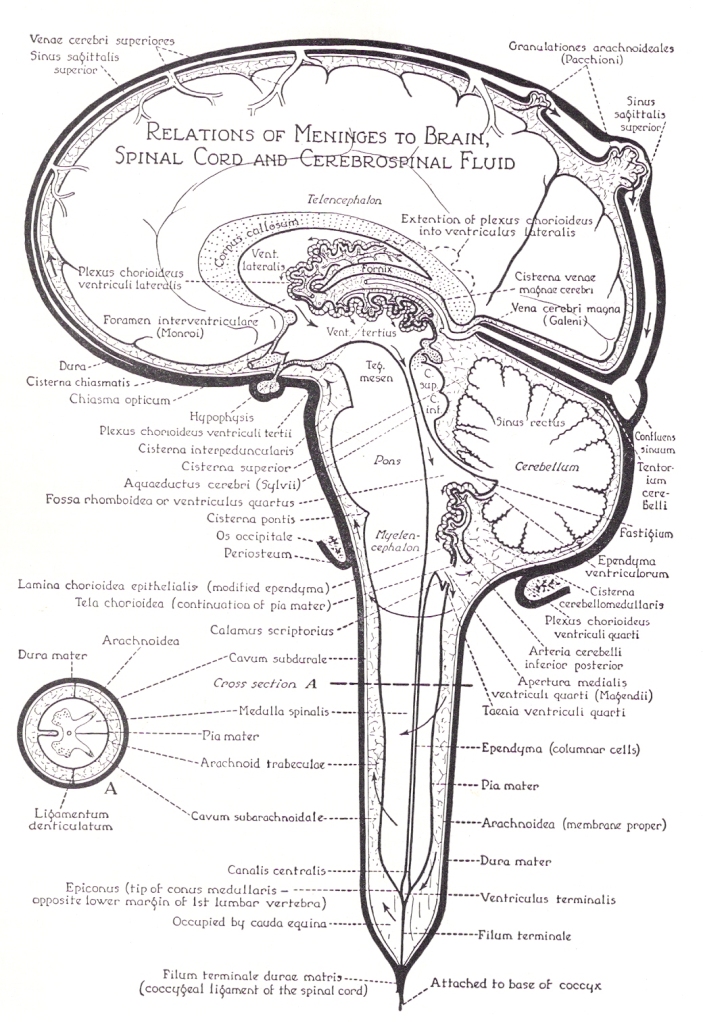
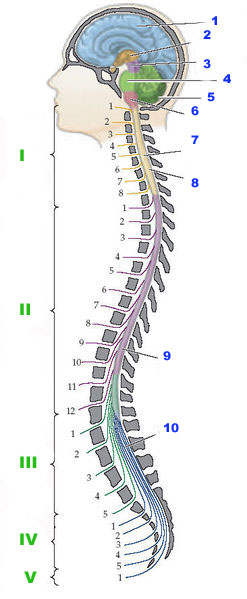
Cerebrospinal fluid (CSF), a filtrate of blood, is basically water with some sugar and other elements mixed in. CSF is produced in the four ventricles (chambers) of the brain. From there it follows through various channels and into every nook and cranny of the brain. It also flows down through the spinal cord. For the most part, as far as we currently know, most CSF finds its way from the cord back to the brain where it eventually flows into the major veins of the brain and exits the skull by way of the internal jugular and vertebral veins.
Click on the sketch of the brain below to enlarge it. (This is a sagittal view meaning looking at one half of the brain and cord as though they were split from front to back.) In this analogy the person is lying on their side. Now look at the sketch as though it was a nautical map of many lakes and rivers with the brain and cord being the land masses. All the folds, creases, crevices and cracks you see in the brain are like large and small fiords filled with water (CSF). The coast of the brain is completely surrounded by the sea so that no surface is untouched by water (CSF). The cord is, likewise, surrounded by water. Both are further bound by large rivers, which are the dural sinuses (veins) of the brain and vertebral veins of the cord.
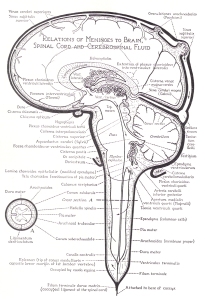
CSF begins its journey in the lateral ventricles (lakes) located in the center of the brain. The squiggly lines surrounding the lakes are like mountains from which water flows down through streams to fill the lakes. The arrows show the direction of the current and CSF flow in the brain and cord.
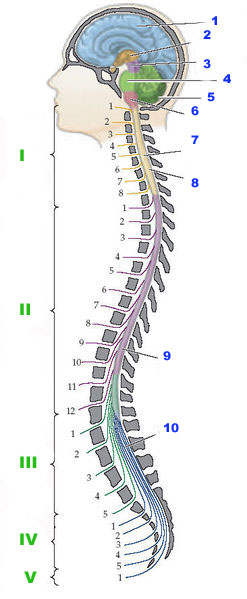
The first two lakes flow into the next lake (third ventricle) where additional water from surrounding hills enter the system. It then flows through a tight canal called an aqueduct and enters yet another lake (fourth ventricle) with a large land mass protruding into it. Again, rivers from the surrounding hills that line the coast contribute even more water but this is the last place where water enters the system.
From the last lake (the fourth ventricle) CSF flows out into a gulf called the basal cisterns of the brain. From here, in the gulf, it can flow in one of two directions. It can either flow back up to the top of the brain or it can flow down into the cord. At the bottom of the cord is a large sea called the lumbar cistern. The capacity and volume of CSF (water) in the cord and lumbar cistern, like the ocean, is far greater than the combined capacity of all the ventricles, cisterns and spaces in the brain.
The direction CSF takes when it enters the gulf of the basal cisterns depends on which way the tide is going which is determined by the gravitational pull of the earth, as well as the time of day, which will be explained below. If it gets strong enough, wind can also affect the current and flow of CSF (water) in the cisterns (gulf). It can even cause it to take alternative routes. In either case, once it leaves the (ventricles) lakes where it is produced, CSF moves through channels that don’t contribute any additional water. Those channels are depicted by spaces with stipled lines.
In the position described above (the person on their side) the tide is in and the flow of CSF in the brain and the cord is mostly upwards toward the top of the brain. When it reaches the top of the brain it empties into part of the drainage system of the brain called the venous lacunae, lacunae means lakes. The venous lacunae contain canals called arachnoid granulations that are small protrusions (villi) of the arachnoid layer (middle covering of the brain) that connect the CSF pathways to the largest vein of the brain called the superior sagittal sinus. They transfer CSF back into the blood stream through the venous drainage system.
After it leaves the stipled CSF pathways and enters the superior sagittal sinus by way of the arachnoid granulation, slightly further down you can see a white circle called a confluence. A confluence is a place where rivers meet. In this case several large veins (rivers) meet at the confluence. From here the large veins drain down into the basement of the skull called the posterior fossa and enter into either the internal jugular veins or vertebral veins.
The tide changes in this analogy when we turn the system upright. When we stand upright, the current speeds up and the tide flows away from the brain. During the night when we sleep the tide returns back toward the brain. Hanging upside down (inversion) causes a strong reversal in the tide. Straining while holding the breath, which is called a Valsalva maneuver also causes back pressure against the current and can, likewise, reverse tides. Strong tides can cause rivers to change their course in the brain and seek other outlets. In my book, The Downside of Upright Posture, I discuss giraffes, bats and whales and the forces they have to deal with. Giraffes and bats had to find ways to contend with tides caused by exceptional inversion flows from long necks and spending long periods of time hanging upside down. In giraffes it occurs when they lower their head to drink water. In bats the tides shift when they sleep. In humans tides shift when we wake up from lying down to sit or stand upright.
The first place to feel the affects of shifts in currents and tides in the brain is where they collide in the gulf of the basal cisterns. If you look closely at the picture you will see a cistern above and below the cerebellum. There are also cisterns below and in front of the cord. The cisterns in the spaces above the pons of the cord and the cerebellum surround the midbrain. Among other things the midbrain contains the cerebral aqueduct (canal for CSF flow) and the substantia nigra. The substantia nigra is where dopamine is produced and is affected in Parkinson’s disease. I suspect that increased volume and pressure in the ventricles and cisterns may play a role in Parkinson’s disease. Increased CSF volume and pressure in the ventricles and cisterns may play a role in other neurodegenerative diseases as well.
The wind in the system comes from respiration (breathing). Most times breathing merely creates ripples that help to move CSF along. Sometimes, however, it causes a great deal of back pressure, such as in a Valsalva maneuver mentioned above, which forces CSF to find alternative outlets to exit the brain in order to keep things flowing and prevent backups in the system.
 When it comes to the impact of currents, winds and tides, tide has a far greater influence on CSF flow. When large ocean tides rush into small river channels tidal bores (waves) occur. Where river currents and ocean tides collide standing waves called clapotis can occur. Tidal bores and clapotis (covered in my last blog) cause turbulance that moves depris which scour and undermine anything in its wake. Coasts are shaped by the relentless ebb and flow of daily tides. Anything that stands in its way or disrupts the ebb and flow of relentless tide and current is subject to erosion. The same thing happens in the brain.
When it comes to the impact of currents, winds and tides, tide has a far greater influence on CSF flow. When large ocean tides rush into small river channels tidal bores (waves) occur. Where river currents and ocean tides collide standing waves called clapotis can occur. Tidal bores and clapotis (covered in my last blog) cause turbulance that moves depris which scour and undermine anything in its wake. Coasts are shaped by the relentless ebb and flow of daily tides. Anything that stands in its way or disrupts the ebb and flow of relentless tide and current is subject to erosion. The same thing happens in the brain.When it comes to the brain the posterior fossa is the first area to feel the affect of tidal bores and clapotis. If the tidal waves are strong enough it can start to back up into the lakes (ventricles) and affect the structures that line their shores. The first ventricle (lake) to feel the affect is the fourth ventricle (lowest). Not surprisingly, the cisterns and ventricles are similarly affected in Dandy-Walker syndrome seen in children and a variant of Parkinson’s disease called multisystem atrophy or olivopontine cerebellar atrophy seen in adults. Both conditions are associated with enlarged cisterns and cystic (enlarged) fourth ventricles mentioned in previous posts.
Dandy-Walker sydrome is a congenital malformation of the brain originally referred to as Dandy-Walker cysts. It was named after Dr. Walter Edward Dandy and Dr. Earl Walker. The contributions of Dr. Dandy to neurosurgery and our understanding of CSF flow and hydrocephalus are legendary and far too numerous to describe here. Among other things he trained under Dr. Harvey Cushing mentioned above. The Dandy Walker cyst-like malformation is somewhat like a reverse Chiari malformation in that the posterior fossa is too large, the brainstem and cerebellum are too small and the cerebellum herniates upward into the tentorium cerebelli rather than downwards into the foramen magnum. Brain shrinkage and increased CSF volume has also been associated with Alzheimer’s disease and multiple sclerosis.
The choke point in the CSF and venous circulatory system of the brain is in the foramen magnum and upper cervical spinal canal. Degeneration (spondylosis) and misaligments of the lower cervical spine can further affect the current and flow of blood and CSF between the brain and cord. For additional information regarding the connection between the brain and cord visit our site at www.upright-health.com.
CSF, Clapotis, Cisterns and Cysts
 The picture on the right is an example of clapotis. It comes from a book called Sea Kayak by Gordon Brown who teaches classes in Scotland where sea and surf are notoriously rough. White water and open sea kayakers are attracted to waves and love to study all their subtleties.
The picture on the right is an example of clapotis. It comes from a book called Sea Kayak by Gordon Brown who teaches classes in Scotland where sea and surf are notoriously rough. White water and open sea kayakers are attracted to waves and love to study all their subtleties.Clapotis is a nautical term for standing waves. It is French for lapping of water. According to English translators it is pronounced as clap-o-tee, like a long sounding “o”, as in toe. According to my Canadian French connection, it is pronouned more like clap-ah-tee, similar to the short sound of ”o” as in copper. In either case, in French, the “s”, at the end of the word indicates that it is plural, meaning more than one wave, but it is silent.
Clapotis occur when waves clap together such as incoming ocean waves running into waves that have bounced off of objects such as rocky coasts or manmade seawalls. Clapotis can be explosive and sometimes roar from the rush of the water. Like the sound of the “s” on the end, sometimes they can be silent and gentle swells like those that occur between the land masses of a mainland and its barrier islands. The ocean waves are calmer but still reflect between these land masses.
As all sea faring people well know, however, silent or not, standing waves can be deceptive, destructive and even deadly. On the bottom side they scour and tear at the footers of manmade seawalls. They similarly severely undermine and damage coasts. On the top side they can toss and turn ships about like toys in a tub.
Rogue waves are a type of standing wave. They are also known as freak or killer waves because they suddenly spring up seemingly out of nowhere and significantly increase the height and strength of a wave. They often travel against prevailing winds and currents and are sometimes preceded by deep troughs that look like a hole in the ocean. Killer waves can run aground, wreck, roll and swallow unsuspecting ships, sometimes in a matter of minutes and sometimes only seconds. For centuries scientists scoffed at sailors and claimed the sailors were spinning tall tales from too much time spent isolated at sea. New evidence, however, has rocked their boat. Sailors were right, these waves do exist. As yet, we know very little about them or what stirs them up. What we do know is that fluids basically follow pressure gradients and the path of least resistance.
In physics, clapotis are considered to be transverse waves because they can rise up. In other words, they travel up and down in a two dimensional plane. Consequently, clapotis cannot occur in rigid containers, such as water pipes in homes, because rigid containers can’t expand and allow the wave to rise. Instead rigid containers cause longitudinal waves. Longitudinal waves are caused by alternating compression and expansion of fluids or air within a confined space. For example, longitudinal waves occur in muscial instruments that use pipes to make sound. In contrast to transverse waves, longitudinal waves travel in one plane.
Unlike standing waves, water hammers occur in rigid containers, such as pipes, when a forceful stream of moving water is suddenly stopped. The rapid change in velocity causes a collision similar to a standing wave but the outcome is different. Because the wave cannot increase in height it causes compression (a longitudinal movement), which increases pressure that travels back through the pipes. The stiff pipes absorb the energy, which causes them to shake along their course. Unlike the “s” at the end of clapotis, water hammers are not silent. They make a loud banging noise like someone hammering on the plumbing. Over time, water hammers can break pipe joints.
 When it comes to standing waves and water hammers, the latest research is starting to connect faulty cerebrospinal fluid (CSF) flow with the cause of neurodegenerative diseases such as Alzheimer’s, Parkinson’s and multiple scleriosis, which is the subject of my book, “The Downside of Upright Posture”. I started looking into the role of CSF in neurodegenerative diseases about thirty years ago because of my background in upper cervical chiropractic and craniopathy, which led me to the subject of physical anthropology.
When it comes to standing waves and water hammers, the latest research is starting to connect faulty cerebrospinal fluid (CSF) flow with the cause of neurodegenerative diseases such as Alzheimer’s, Parkinson’s and multiple scleriosis, which is the subject of my book, “The Downside of Upright Posture”. I started looking into the role of CSF in neurodegenerative diseases about thirty years ago because of my background in upper cervical chiropractic and craniopathy, which led me to the subject of physical anthropology.Upper cervical chiropractic taught me the importance of the upper cervical spine and base of the skull to human health. Craniopathy taught me about the design of the human skull and the movement of cerebrospinal fluid through the brain and cord. Because of craniopathy, I also became interested in the base and sutures of the skull. In particular, I became interested in the sutures that unite the membranous bones of the skull that form the cover over the cranial vault, which contains the brain.
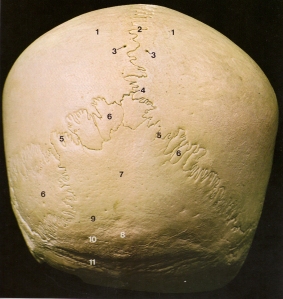
The picture above on the left shows the sutures at the back and bottom of the skull. Like all bones, the sutures are a reflexion of the mechanical stresses that strained and shaped them. Early anatomists called them sutures because they thought they looked somewhat similar to surgical stitches. But to me they look more like waves and they are shaped that way for a reason. They are similar to a seismic recording of pressure fluctuations and movement in the skull and cranial vault. The pressure fluctuations come from a combination of neurological (electrical), circulatory and respiratory waves. Upright posture and bipedal walking further amplify those waves.
 CSF is a watery fluid produced in cavities of the brain called ventricles. CSF flows out of the ventricles and into the cisterns and subarachnoid spaces of the brain and spinal cord. The role of CSF is to cushion, protect and support the brain to prevent it from sinking inside the cranial vault. It also carries waste out of the brain.
CSF is a watery fluid produced in cavities of the brain called ventricles. CSF flows out of the ventricles and into the cisterns and subarachnoid spaces of the brain and spinal cord. The role of CSF is to cushion, protect and support the brain to prevent it from sinking inside the cranial vault. It also carries waste out of the brain.CSF is under constant fluctuating hydraulic pressures due to the pumping of the heart which increases arterial pressure in the brain when it contracts. Likewise, breathing causes changes in pressure inside the ribcage. During exhalation pressure inside the ribcage increases. Among other things this increases venous pressure which is transmitted to the vertebral veins. The vertebral veins are connected to the dural sinuses of the brain and like the dural sinuses, have no valves to prevent inversion (reverse) flows. Consequently, respiratory pressure changes are transmitted to the brain and exhalation increases intracranial pressure.
Because the cranial vault is a closed container, the increase in blood volume and intracranial pressure needs to be controlled. When things are working properly, any excess CSF volume and pressure is typically vented out of the cranial vault via the foramen magnum and down into the subarachnoid space of the spinal canal. Inherited (genetic) and acquired (aging and injuries) structural problems in the cervical spine can cause back pressure against the venting mechanism. If outgoing CSF waves meet resistance or inversion flows of blood and CSF waves coming up from the vertebral veins and subarachnoid space (contains CSF) in the spinal canal then clapotis (standing waves) or water hammers can occur.
In the sketch above on the right, the brain is like a landmass inside the cranial vault surrounded by a sea of CSF and venous blood in vessels with no valves to prevent inversion flows. The skull is a fairly rigid container. Consequently, the amplitude of any standing waves (clapotis) in the brain is limited. Thus the standing wave that occurs as CSF in the brain claps into CSF in the cord as it attempts to flow through the foramen magnum and out of the cranial vault becomes more like a water hammer.
In either case, the first areas of the brain to receive the brunt of either clapotis or water hammers are the basal cisterns that surround the cerebellum and brainstem. It is possible that over time, chronic clapotis (standing waves) or constant banging from water hammers in the basal cisterns weaken and eventually erode the soft tissues of the brain the same as rocky coasts.
Similarly, I suspect that standing waves and water hammers may also play a role in the formation of arachnoid cysts and empty sella syndromes, as well as the Dandy-Walker and Shy-Drager syndrome (a variant of Parkinson’s disease) type cysts seen in the ventricles and cisterns.
For a better understanding of the big picture read my book. For further information visit my website at www.upright-health.com.
Posted in Alzheimer's, arachnoid cysts, chiari malformations, CSF, Dandy-Walker syndrome, dementia, demyelination, Devic's disease, Ehlers Danlos Syndrome, empty sella syndrome, ms lesions, multiple sclerosis, neuromyelitis optica, optic neuritis, optic spinal multiple sclerosis, Parkinson's, physical anthropology, spondylosis, syrinxes Leave a comment
The Missed Measure of Man
The missed measure of man was overlooked during earlier investigations of human cranial capacity that focused on its relationship to intelligence. That is what the book to the right set about to disprove. Unfortunately, the subject of cranial capacity due to it’s ties to human intelligence has since become taboo to discuss due to political correctness. This is unfortunate because cranial capacity may play a key role in neurodegenerative diseases such as Alzheimer’s, Parkinson’s and multiple sclerosis and has nothing to do with intelligence. The missed measure of man that was overlooked is the design, layout and capacity of the posterior fossa in particular.
Some scientists once believed that there was a direct correlation between cranial capacity and human intelligence. It is a myth I cover in the last chapter in my book. The first problem is that there is no direct linear correlation between brain size and intelligence. If there were then elephants and whales would be smarter than humans. Similarly speaking, parrots have small cranial capacities but are far more intelligent (due to the way we test intelligence) than many mammals with much larger brains. Furthermore, regardless of race, females tend to have a smaller cranial capacity compared to males and Einstein, who was considered by many to be a genius, had an exceptionally small cranial capacity. In fact, his cranium was at the very low end of female capacity.
There is another problem and that is the way we measure intelligence. The brain is a survival organism. It’s job it to help us manipulate and master our environment. IQ tests are prejudiced against indigenous people who must master and remember many things about their environment and rely on ingenuity to survive and thrive. IQ tests fail to measure the subtleties and full spectrum of human intellect such as creativty, imagination and intuition among other things. Instead, modern IQ tests measure abstractions and memory in ways that may be important to people living in industrialized socities but are useless to indigenous people. Many people with so called high IQ’s wouldn’t be able to survive in similar circumstances. The bottom line is that the correlation between IQ and cranial capacity doesn’t work.
Presumably there are about one hundred billion nerves cells in the brain. Interestingly, the cerebellum sits in the posterior fossa and has more nerves that the rest of the brain put together. The truth is no one has actually counted. It is simply a guess based on average brain weight, the amount of fat and other factors. The average brain in humans weighs 1300-1400 grams or about 2.75-3.5 pounds. About half of it is fat. The rest of it is nerve cells. As far as we know for now, until proven otherwise, all humans are born with roughly the same number of nerve cells in the brain give or take a few billion or so. Bigger heads simply have bigger brains with larger nerves and more fat, not necessarily more nerves.
Nonetheless, a great deal of time and energy was wasted at the time measuring the size of the head and the capacity of the cranial vault. The famous book by Jay Gould pictured above was published in 1984 called The Mismeasure of Man. In it Gould refutes the arguements of the day, some of which were racially motivated.
Disregarding the old ignorant debates about cranial capacity and intelligence, there are many important issues to consider when it comes to race, gender and health. Just as females and males have different health concerns, certain health conditions have a higher incidence in particular races and ethnic groups. For example, thalasemia and sickle cells affect Asians and Africans far more than northern Europeans. Europeans living on the Mediterranean, however, are likewise effected. Thalasemia and sickle cell anemia are believed to have been protective mechanisms against malaria. The downside is they predispose afflicted people to anemia. Just as blood cells affect our physiology so does the design of the skull.
It is easy to see racial differences, including mixed races, simply by looking at the face. In this regard, it is interesting to note that the design of the facial part of the skull is intimately connected to the design of the base of the skull. They grow together during development and have a strong influence on one another. Their growth in childhood follows the musculoskeletal system of the rest of the body.
Together, the face and base of the skull determine the basic layout of the floor of the cranial vault. The bones that form the curved walls and cap the top of the cranial vault follow the growth of the brain. The cover over the cranial vault stops growing early in life when the brain stops growing in size.
 There are significant racial and gender differences in the incidence of multiple sclerosis. There are also geographic differences but that’s a different story. When it comes to race, people of Asian and African descent appear to have a distinct advantage in that they appear to have a much lower incidence of MS than European people. When it comes to gender, regardless of race, females appear to have a distinct disadvantage in that they have a significantly higher incidence of MS compared to males. The difference in incidence in both race and gender may be due to design diffferences in the posterior fossa.
There are significant racial and gender differences in the incidence of multiple sclerosis. There are also geographic differences but that’s a different story. When it comes to race, people of Asian and African descent appear to have a distinct advantage in that they appear to have a much lower incidence of MS than European people. When it comes to gender, regardless of race, females appear to have a distinct disadvantage in that they have a significantly higher incidence of MS compared to males. The difference in incidence in both race and gender may be due to design diffferences in the posterior fossa.
The white lines in the brain scan above represent the outline of the posterior fossa. The top line is missing because it represents the opening in the covering over the posterior fossa. The covering is called the tentorium cerebelli. The opening is called the tentorial notch or incisura. The scan is from a paper called, “Dimensions of the posterior fossa in patients symptomatic for Chiari 1 malformation but without cerebellar tonsillar descent,” by Sekula et. al., published in Fluids and Barriers of the CNS in 2005.
Among other things, a smaller or hypoplastic posterior fossa is more susceptible to Chiari malformations. In this regard, females most likely have a smaller posterior fossa compared to most males. They also have a higher incidence of multiple sclerosis compared to males.
Up until the eighth decade, they also have a higher incidence and get Alzheimer’s sooner than males. Females are also far more susceptible to Chiari malformations and to Dandy-Walker syndrome. Dandy-Walker syndrome, as you may recall, is related to enlarged ventricles and cysts that effect CSF flow mentioned in the previous post. The increased incidence of these particular conditions in females may have to do with the design of the posterior fossa, especially its capacity.
When it comes to race, a fairly recent orthodontic study on racial differences in craniofacial design done in Scotland showed that Europeans tend to have a shorter clivus in the base of the skull. This is interesting because a shorter clivus could decrease the capacity of the posterior fossa in Europeans compared to Asian and African designs. Thus, if the old arguments regarding a correlation between cranial capacity and IQ were true, then European brains would have fewer nerves compared to Asian and African brains. In addition to the capacity of the posterior fossa, other design issues to consider are the angles and pitch of the clivus and the tentorium cerebelli, as well as the angle of the base of the skull to the upper cervical spine.
Another issue to consider is, although they don’t get classic MS, Asians and Africans do get optic spinal multiple sclerosis and Devic’s disease. What’s more, Devic’s tends to be relatively more severe and disabling. Both optic spinal multiple sclerosis and Devic’s may be variants of multiple sclerosis due to design differences in the posterior fossa. The problem may lie in our method of diagnosing MS, which is based on classic lesions. Apparently, Asian and African people don’t get classic lesions. Aside from that, they otherwise get similar signs and symptoms. Consequently, many cases of MS among African and and Asian races may have been and continue to be overlooked and marginalized.
In addition, the condition of hydrocephalus is as old as the human race. It started with standing upright. All races are equally susceptible. Lastly, as we continue to learn more from upright MRI, just as I predicted in my book, it appears Chiari malformations also referred to as cerebellar tonsillar ectopia (CTE) are far more common than once thought. They can occur later in life due to trauma, aging and misalignments of the upper cervical spine that cause the brainstem to get pulled down or to sag slightly, due to low pressure, toward the base of the skull and into the foramen magnum. Tethered cords from a genetically short cord or from degeneration and abnormal curvatures of the spine can also cause CTE. Humans are susceptible to CTE by design and CTE can cause hydrocephalic-like conditions. Furthermore, hydrocephalic conditions and CTE may be at the core and cause of many neurodegenerative diseases. One of the causes lies in the design, layout and capcity of the posterior fossa. Other causes will be discussed as my blog and website continue to grow. For further information visit my website at www.upright-health.com.
Some scientists once believed that there was a direct correlation between cranial capacity and human intelligence. It is a myth I cover in the last chapter in my book. The first problem is that there is no direct linear correlation between brain size and intelligence. If there were then elephants and whales would be smarter than humans. Similarly speaking, parrots have small cranial capacities but are far more intelligent (due to the way we test intelligence) than many mammals with much larger brains. Furthermore, regardless of race, females tend to have a smaller cranial capacity compared to males and Einstein, who was considered by many to be a genius, had an exceptionally small cranial capacity. In fact, his cranium was at the very low end of female capacity.
There is another problem and that is the way we measure intelligence. The brain is a survival organism. It’s job it to help us manipulate and master our environment. IQ tests are prejudiced against indigenous people who must master and remember many things about their environment and rely on ingenuity to survive and thrive. IQ tests fail to measure the subtleties and full spectrum of human intellect such as creativty, imagination and intuition among other things. Instead, modern IQ tests measure abstractions and memory in ways that may be important to people living in industrialized socities but are useless to indigenous people. Many people with so called high IQ’s wouldn’t be able to survive in similar circumstances. The bottom line is that the correlation between IQ and cranial capacity doesn’t work.
Presumably there are about one hundred billion nerves cells in the brain. Interestingly, the cerebellum sits in the posterior fossa and has more nerves that the rest of the brain put together. The truth is no one has actually counted. It is simply a guess based on average brain weight, the amount of fat and other factors. The average brain in humans weighs 1300-1400 grams or about 2.75-3.5 pounds. About half of it is fat. The rest of it is nerve cells. As far as we know for now, until proven otherwise, all humans are born with roughly the same number of nerve cells in the brain give or take a few billion or so. Bigger heads simply have bigger brains with larger nerves and more fat, not necessarily more nerves.
Nonetheless, a great deal of time and energy was wasted at the time measuring the size of the head and the capacity of the cranial vault. The famous book by Jay Gould pictured above was published in 1984 called The Mismeasure of Man. In it Gould refutes the arguements of the day, some of which were racially motivated.
Disregarding the old ignorant debates about cranial capacity and intelligence, there are many important issues to consider when it comes to race, gender and health. Just as females and males have different health concerns, certain health conditions have a higher incidence in particular races and ethnic groups. For example, thalasemia and sickle cells affect Asians and Africans far more than northern Europeans. Europeans living on the Mediterranean, however, are likewise effected. Thalasemia and sickle cell anemia are believed to have been protective mechanisms against malaria. The downside is they predispose afflicted people to anemia. Just as blood cells affect our physiology so does the design of the skull.
It is easy to see racial differences, including mixed races, simply by looking at the face. In this regard, it is interesting to note that the design of the facial part of the skull is intimately connected to the design of the base of the skull. They grow together during development and have a strong influence on one another. Their growth in childhood follows the musculoskeletal system of the rest of the body.
Together, the face and base of the skull determine the basic layout of the floor of the cranial vault. The bones that form the curved walls and cap the top of the cranial vault follow the growth of the brain. The cover over the cranial vault stops growing early in life when the brain stops growing in size.
 There are significant racial and gender differences in the incidence of multiple sclerosis. There are also geographic differences but that’s a different story. When it comes to race, people of Asian and African descent appear to have a distinct advantage in that they appear to have a much lower incidence of MS than European people. When it comes to gender, regardless of race, females appear to have a distinct disadvantage in that they have a significantly higher incidence of MS compared to males. The difference in incidence in both race and gender may be due to design diffferences in the posterior fossa.
There are significant racial and gender differences in the incidence of multiple sclerosis. There are also geographic differences but that’s a different story. When it comes to race, people of Asian and African descent appear to have a distinct advantage in that they appear to have a much lower incidence of MS than European people. When it comes to gender, regardless of race, females appear to have a distinct disadvantage in that they have a significantly higher incidence of MS compared to males. The difference in incidence in both race and gender may be due to design diffferences in the posterior fossa.The white lines in the brain scan above represent the outline of the posterior fossa. The top line is missing because it represents the opening in the covering over the posterior fossa. The covering is called the tentorium cerebelli. The opening is called the tentorial notch or incisura. The scan is from a paper called, “Dimensions of the posterior fossa in patients symptomatic for Chiari 1 malformation but without cerebellar tonsillar descent,” by Sekula et. al., published in Fluids and Barriers of the CNS in 2005.
Among other things, a smaller or hypoplastic posterior fossa is more susceptible to Chiari malformations. In this regard, females most likely have a smaller posterior fossa compared to most males. They also have a higher incidence of multiple sclerosis compared to males.
Up until the eighth decade, they also have a higher incidence and get Alzheimer’s sooner than males. Females are also far more susceptible to Chiari malformations and to Dandy-Walker syndrome. Dandy-Walker syndrome, as you may recall, is related to enlarged ventricles and cysts that effect CSF flow mentioned in the previous post. The increased incidence of these particular conditions in females may have to do with the design of the posterior fossa, especially its capacity.
When it comes to race, a fairly recent orthodontic study on racial differences in craniofacial design done in Scotland showed that Europeans tend to have a shorter clivus in the base of the skull. This is interesting because a shorter clivus could decrease the capacity of the posterior fossa in Europeans compared to Asian and African designs. Thus, if the old arguments regarding a correlation between cranial capacity and IQ were true, then European brains would have fewer nerves compared to Asian and African brains. In addition to the capacity of the posterior fossa, other design issues to consider are the angles and pitch of the clivus and the tentorium cerebelli, as well as the angle of the base of the skull to the upper cervical spine.
Another issue to consider is, although they don’t get classic MS, Asians and Africans do get optic spinal multiple sclerosis and Devic’s disease. What’s more, Devic’s tends to be relatively more severe and disabling. Both optic spinal multiple sclerosis and Devic’s may be variants of multiple sclerosis due to design differences in the posterior fossa. The problem may lie in our method of diagnosing MS, which is based on classic lesions. Apparently, Asian and African people don’t get classic lesions. Aside from that, they otherwise get similar signs and symptoms. Consequently, many cases of MS among African and and Asian races may have been and continue to be overlooked and marginalized.
In addition, the condition of hydrocephalus is as old as the human race. It started with standing upright. All races are equally susceptible. Lastly, as we continue to learn more from upright MRI, just as I predicted in my book, it appears Chiari malformations also referred to as cerebellar tonsillar ectopia (CTE) are far more common than once thought. They can occur later in life due to trauma, aging and misalignments of the upper cervical spine that cause the brainstem to get pulled down or to sag slightly, due to low pressure, toward the base of the skull and into the foramen magnum. Tethered cords from a genetically short cord or from degeneration and abnormal curvatures of the spine can also cause CTE. Humans are susceptible to CTE by design and CTE can cause hydrocephalic-like conditions. Furthermore, hydrocephalic conditions and CTE may be at the core and cause of many neurodegenerative diseases. One of the causes lies in the design, layout and capcity of the posterior fossa. Other causes will be discussed as my blog and website continue to grow. For further information visit my website at www.upright-health.com.
Posted in Alzheimer's, arachnoid cysts, chiari malformations, cranial capacity, CSF, Dandy-Walker syndrome, dementia, Devic's disease, human intellect, measure intelligence, multiple sclerosis, neuromyelitis optica, optic neuritis, optic spinal multiple sclerosis, Parkinson's, physical anthropology Leave a comment
Cysts, Syrinxes and CSF
Cavities such as cysts and syrinxes that may or may not contain cerebrospinal fluid (CSF) are seen in the brain and cord. In this post we are concerned with the types that contain CSF. Faulty fluid mechanics in the brain and cord can cause these types of cavities to form. Likewise, cysts and syrinxes can cause faulty fluid mechanics in the brain and cord.
Cysts sometimes develop in the middle layer of the three protective coverings of the brain and cord, called meninges. If you look at the picture below, toward the bottom on the right hand side, there is a label pointing to a dark line called dura mater. The dura mater is the tough outer covering that surrounds the brain and cord. Above the dura mater is another label, called the arachnoidea, which points to a white line surrounding the brain and cord. The arachnoid mater is the middle layer of the meninges. Still another label above that points to a black line called the pia mater, which is the inner most layer of the covering of the brain and cord. The subarachnoid space is the stipled area that lies between the arachnoid and pia mater.
 Arachnoid cysts are fairly common. They project out from the arachnoid mater covering and subarachnoid space. They are also called leptomeningeal cysts. Arachnoid cysts tend to occur in certain places in the brain and cord. One of the common areas is the middle fossa of the cranial vault, as well as the Sylvian fissure of the brain which is located in the middle fossa. The Sylvian fissure is a deep fold which separates the frontal, temporal and parietal lobes of the brain.
Arachnoid cysts are fairly common. They project out from the arachnoid mater covering and subarachnoid space. They are also called leptomeningeal cysts. Arachnoid cysts tend to occur in certain places in the brain and cord. One of the common areas is the middle fossa of the cranial vault, as well as the Sylvian fissure of the brain which is located in the middle fossa. The Sylvian fissure is a deep fold which separates the frontal, temporal and parietal lobes of the brain.
Other common areas for arachnoid cysts are, within the covering over the posterior fossa called the tentorium cerebelli (the black line over top of cerebellum), the cisterna magna (the stipled area beneath the cerebellum), which is a cistern located between the cerebellum and the medulla oblongata, and the suprasellar region, which is a cavity in a bone in the skull that houses the pituitary gland (the hypophysis hanging down beneath the front of the brain).
If you look at the middle of the brain in the picture above, the arrows start in the lateral ventricles and flow down through the third ventricle, the cerebral aqueduct, and into the fourth ventricle. They then leave the fourth ventricle and enter the stipled area which represents the subarachnoid space.
Enlarged ventricles are typically referred to as ventriculomegaly. Enlargement of the fourth ventricle, however, is sometimes classified as a cyst or cystic ventricle. A well known example of a cystic fourth ventricle is seen in Dandy-Walker syndrome which occurs in children.
Some cysts are acquired later in life, such as from trauma. Trauma can cause cysts due to tears in the meninges. It is currently maintained, however, that most people are born with arachnoid cysts. Some are caused by genetic weakness in the tissues or design flaws in the subarachnoid space. I suspect that still others may occur due to intrauterine positions of the fetus during pregnancy that can potentially increase pressure in critical areas of the brain and cord.
Some cysts are formed in the cord and are called syrinxes from the Greek word tube. If you look at the picture above you will see a canal going down through the center of the cord. The label that points to it on the left near the bottom of the canal is the canalis centralis, which means central canal of the cord. Syrinxes typically start and are found in the central canal but they can spread outwards and affect other parts of the cord.
Syrinxes are typically expansions in the central canal of the cord. The central canal is connected to the lowest ventricle in the brain, which is the fourth. These syrinxes are also referred to as syringomyelia. Similar to cysts, syrinxes are sometimes connected to and sometimes more isolated from CSF pathways, which can trap fluids.
Sometimes the cysts and syrinxes communicate with normal CSF pathways. In the case of subarachnoid cysts the fluid can flow more freely between the cyst and subarachnoid space. In other cases, the cyst is more isolated by connective tissues so that fluids that manage to find there way into the space, find it hard to get out.
Cysts and syrinxes are sometimes associated with significant pressure that causes fluids to eject forcefully when penetrated surgically. The force from the hydraulic nature of cysts and syrinxes can consequently compress nearby tissues. The turbulant flow and subsequent pounding they create can also erode nearby tissues like waves beating on rocky cliffs on a shoreline. Turbulant flow can, likewise, erode bone. In the skull it leaves impressions that look like little dents on the inside roof of the cranial vault. Researchers now suspect that the turbulant CSF flow caused by Chiari malformations may play a role in the formation of syrinxes in the central canal of the cord.
Chiari malformations obstruct CSF flow through the foramen magnum of the skull and the upper cervical spine, which can cause normal pressure hydrocephalus (NPH) in adults. Lastly, Chiari malformations and NPH have been associated with multiple sclerosis and other neurodegenerative conditions.
Cysts and syrinxes speak volumes about CSF and the hydraulic stress it causes in the brain and cord. What’s more, obstruction of CSF flow through the foramen magnum and upper cervical spine and the faulty fluid mechanics and hydraulic stresses it creates may be one of the root causes of Alzheimer’s, Parkinson’s and multiple sclerosis, as well as other neurodegenerative diseases. Ventriculomegaly (enlargement of a ventricle) has been associated with all three of these conditions. Two variants of Parkinson’s disease are also associated with cystic conditions within the ventricles and cisterns. In most cases, the cause of cysts and syrinxes is unknown.
I will be covering more on cysts and syrinxes on this blog and my website in future posts. For now, for further information click on syringomyelia above or visit my website at www.upright-health.com.
Cysts sometimes develop in the middle layer of the three protective coverings of the brain and cord, called meninges. If you look at the picture below, toward the bottom on the right hand side, there is a label pointing to a dark line called dura mater. The dura mater is the tough outer covering that surrounds the brain and cord. Above the dura mater is another label, called the arachnoidea, which points to a white line surrounding the brain and cord. The arachnoid mater is the middle layer of the meninges. Still another label above that points to a black line called the pia mater, which is the inner most layer of the covering of the brain and cord. The subarachnoid space is the stipled area that lies between the arachnoid and pia mater.
 Arachnoid cysts are fairly common. They project out from the arachnoid mater covering and subarachnoid space. They are also called leptomeningeal cysts. Arachnoid cysts tend to occur in certain places in the brain and cord. One of the common areas is the middle fossa of the cranial vault, as well as the Sylvian fissure of the brain which is located in the middle fossa. The Sylvian fissure is a deep fold which separates the frontal, temporal and parietal lobes of the brain.
Arachnoid cysts are fairly common. They project out from the arachnoid mater covering and subarachnoid space. They are also called leptomeningeal cysts. Arachnoid cysts tend to occur in certain places in the brain and cord. One of the common areas is the middle fossa of the cranial vault, as well as the Sylvian fissure of the brain which is located in the middle fossa. The Sylvian fissure is a deep fold which separates the frontal, temporal and parietal lobes of the brain.Other common areas for arachnoid cysts are, within the covering over the posterior fossa called the tentorium cerebelli (the black line over top of cerebellum), the cisterna magna (the stipled area beneath the cerebellum), which is a cistern located between the cerebellum and the medulla oblongata, and the suprasellar region, which is a cavity in a bone in the skull that houses the pituitary gland (the hypophysis hanging down beneath the front of the brain).
If you look at the middle of the brain in the picture above, the arrows start in the lateral ventricles and flow down through the third ventricle, the cerebral aqueduct, and into the fourth ventricle. They then leave the fourth ventricle and enter the stipled area which represents the subarachnoid space.
Enlarged ventricles are typically referred to as ventriculomegaly. Enlargement of the fourth ventricle, however, is sometimes classified as a cyst or cystic ventricle. A well known example of a cystic fourth ventricle is seen in Dandy-Walker syndrome which occurs in children.
Some cysts are acquired later in life, such as from trauma. Trauma can cause cysts due to tears in the meninges. It is currently maintained, however, that most people are born with arachnoid cysts. Some are caused by genetic weakness in the tissues or design flaws in the subarachnoid space. I suspect that still others may occur due to intrauterine positions of the fetus during pregnancy that can potentially increase pressure in critical areas of the brain and cord.
Some cysts are formed in the cord and are called syrinxes from the Greek word tube. If you look at the picture above you will see a canal going down through the center of the cord. The label that points to it on the left near the bottom of the canal is the canalis centralis, which means central canal of the cord. Syrinxes typically start and are found in the central canal but they can spread outwards and affect other parts of the cord.
Syrinxes are typically expansions in the central canal of the cord. The central canal is connected to the lowest ventricle in the brain, which is the fourth. These syrinxes are also referred to as syringomyelia. Similar to cysts, syrinxes are sometimes connected to and sometimes more isolated from CSF pathways, which can trap fluids.
Sometimes the cysts and syrinxes communicate with normal CSF pathways. In the case of subarachnoid cysts the fluid can flow more freely between the cyst and subarachnoid space. In other cases, the cyst is more isolated by connective tissues so that fluids that manage to find there way into the space, find it hard to get out.
Cysts and syrinxes are sometimes associated with significant pressure that causes fluids to eject forcefully when penetrated surgically. The force from the hydraulic nature of cysts and syrinxes can consequently compress nearby tissues. The turbulant flow and subsequent pounding they create can also erode nearby tissues like waves beating on rocky cliffs on a shoreline. Turbulant flow can, likewise, erode bone. In the skull it leaves impressions that look like little dents on the inside roof of the cranial vault. Researchers now suspect that the turbulant CSF flow caused by Chiari malformations may play a role in the formation of syrinxes in the central canal of the cord.
Chiari malformations obstruct CSF flow through the foramen magnum of the skull and the upper cervical spine, which can cause normal pressure hydrocephalus (NPH) in adults. Lastly, Chiari malformations and NPH have been associated with multiple sclerosis and other neurodegenerative conditions.
Cysts and syrinxes speak volumes about CSF and the hydraulic stress it causes in the brain and cord. What’s more, obstruction of CSF flow through the foramen magnum and upper cervical spine and the faulty fluid mechanics and hydraulic stresses it creates may be one of the root causes of Alzheimer’s, Parkinson’s and multiple sclerosis, as well as other neurodegenerative diseases. Ventriculomegaly (enlargement of a ventricle) has been associated with all three of these conditions. Two variants of Parkinson’s disease are also associated with cystic conditions within the ventricles and cisterns. In most cases, the cause of cysts and syrinxes is unknown.
I will be covering more on cysts and syrinxes on this blog and my website in future posts. For now, for further information click on syringomyelia above or visit my website at www.upright-health.com.
Kyphosis, Stenosis and Multiple Sclerosis
 The spine has four curves. Two of them curve forward toward the belly side of the body. They are the cervical (neck) and lumbar (low back) spines. The other two arch backward toward the back and buttocks. They are the thoracic spine which supports the ribcage, and the sacrum which sits in the back of the pelvis beneath the low back. It is the pedestal the spine rests on and, similar to the thoracic spine, bends backward to support a load.
The spine has four curves. Two of them curve forward toward the belly side of the body. They are the cervical (neck) and lumbar (low back) spines. The other two arch backward toward the back and buttocks. They are the thoracic spine which supports the ribcage, and the sacrum which sits in the back of the pelvis beneath the low back. It is the pedestal the spine rests on and, similar to the thoracic spine, bends backward to support a load.
The term kyphosis refers to the normal curves of the thoracic spine and sacrum. It also refers to an exaggeration of the thoracic curve that causes a pronounced hump or backward bend in the upper back called a Gibbus deformity that pitches the shoulders and neck forward of the normal gravity line. Exaggerated kyphosis also causes a loss in height. In severe cases it can interfere with breathing as it alters the rib cage which contains the lungs and heart. Exaggerated kyphosis is sometimes referred to as hyperkyphosis.
 The term kyphosis can also be used to describe an abnormal curve of the spine that goes in the opposite or wrong direction. For example, it can be used to describe a reversal of the curve in the low back. More commonly, it is used to describe a reversal of the normal curvature in the cervical spine, which is the neck. The x-ray on the right is a good example of a kyphotic (backwards) curve in the cervical spine. Kyphosis occurring in any area of the spine can be inherited as a developmental design problem or it can be acquired later in life through trauma, aging and diseases such as arthritis, osteoporosis, compression fractures and Parkinson’s disease.
The term kyphosis can also be used to describe an abnormal curve of the spine that goes in the opposite or wrong direction. For example, it can be used to describe a reversal of the curve in the low back. More commonly, it is used to describe a reversal of the normal curvature in the cervical spine, which is the neck. The x-ray on the right is a good example of a kyphotic (backwards) curve in the cervical spine. Kyphosis occurring in any area of the spine can be inherited as a developmental design problem or it can be acquired later in life through trauma, aging and diseases such as arthritis, osteoporosis, compression fractures and Parkinson’s disease.Scoliosis is an abnormal lateral (sidewards) curve of the spine. Scoliosis is sometimes associated with kyphosis and is referred to as kyphoscoliosis. Scoliosis is typically a problem that becomes apparent in childhood. It affects females far more than males. Adults, however, can acquire scoliosis later in life due to trauma, degenerative conditions of the spine, inherited and acquired connective tissue disorders and other causes.
Scoliosis has been shown to cause functional stenosis of the spinal canal and subsequent compression of the vertebral veins which decreases venous blood flow. The problem occurs as the veins get compressed against the inside curvature of the spinal canal. Kyphosis most likely causes functional stenosis of the spinal canal and vertebral veins similar to scoliosis.
The images below are used with permission from a member of the TiMS website who underwent testing for chronic cerebrospinal venous insufficiency (CCSVI). The patient was found to have impingement of both internal jugular veins which was corrected by the placement of stents. Subsequent to placement of the stents the patient had considerable improvement in signs and symptoms.
 The image is composed of three different views superimposed on one screen. The view to the left is a plain view x-ray of the upper back and neck. If you look closely at the spinous processes (they look like teardrops that go down the middle of the spine) you will see that they deviate to the left side of the spine. Likewise, if you follow the contour of the sides of the spine you will see that the spine is curved to the left. Since the x-rays were taken from front to back the left side of the film is the right side of the patient.
The image is composed of three different views superimposed on one screen. The view to the left is a plain view x-ray of the upper back and neck. If you look closely at the spinous processes (they look like teardrops that go down the middle of the spine) you will see that they deviate to the left side of the spine. Likewise, if you follow the contour of the sides of the spine you will see that the spine is curved to the left. Since the x-rays were taken from front to back the left side of the film is the right side of the patient.The middle image is a venogram which is an MRI with contrast dye injected into the veins. In this case, the red arrow points to an area of impingement or stenosis of the internal jugular veins just in front of the upper cervical spine. The impingement decreases blood flow through the internal jugular veins, which can back up in the brain.
The image on the right is an x-ray of the stents that were inserted using interventional radiology. More often, most physicians doing the procedure use venoplasty in which a balloon is inserted into the vein and then filled to stretch the vein and open it up. Venoplasty is subject to restenosis. Stents are tubes placed in the veins that spring outward to keep the veins open. Stents are more durable and less likely to re-stenose but pose more problems due to clots. In cases such as the one above it is a tough choice, but if the structural problem causing the impingement is permanent then durability may become more of a factor to consider in choosing procedures.
If you look closely at the above image to the right and follow the contour of the spine you will notice that it arches backwards slightly. As mentioned at the start, the neck or cervical spine should arch gently forward toward the chin. In this particular case the cervical spine is kyphotic or going in the opposite direction that it should.
The internal jugular veins exit the skull through the jugular foramen on the floor of the skull just in front of the transverse process of the C1 vertebra of the upper cervical spine called atlas. After exiting the skull the internal jugular veins join the external jugular veins and follow the curve of the cervical spine on their way down from the head and back to the heart. In the case above, the internal jugulars like the cervical spine bend backward due to the cervical kyphosis. This causes a sharp change in the course of the normal direction of blood flow out of the brain as the internal jugular veins bend around the upper cervical spine. In addition to possibly impinging the internal jugular veins where they exit the skull in front of the transverse process of C1 (atlas), kyphosis most likely compresses the vertebral veins on the inside curve of the cervical spine similar to what scoliosis does in the rest of the spine. Kyphosis and scoliosis most likely play a significant role in CCSVI and CCVBP.
The angle of the upper cervical spine to the base of the skull is important to blood and CSF flow going into and out of the brain and cord. Likewise, the relationship of the base of the skull and upper cervical spine to the curve in the lower cervical spine is important to blood and CSF flow. Inherited and acquired misalignments and disorders of the upper cervical spine, as well as spondylosis (degeneration), scoliosis and other abnormal curves including kyphosis affect blood and CSF flow to the brain and cord. They also cause malpositioning and thus mechanical stress and strain of the brainstem and cord within the skull and spinal canal.
For further information on the upper cervical angle visit my website.
http://www.upright-health.com/upper-cervical-angle.html
Scoliosis, Chiari malformations and CCSVI
The spine is the frame of the body. Its alignment affects all the organs and vessels that surround or are attached to it, including the brain and its blood vessels. The spine also houses the cord, as well as its blood vessels and cerebrospinal fluid (CSF) pathways.
This post is about the impact of scoliosis on the contents of the posterior fossa of the skull, which includes the drainage system of the brain. Abnormal curvatures in the spine alter the normal alignment and relationship of the head and spine, and as a result, the normal relationship of the brain and cord. Curvatures also alter their circulatory routes.
While there may be an attachment of the covering of the upper cord to the foramen magnum, for the most part, the brain is unattached and floats freely inside compartments within the cranial vault. Similarly, the spinal cord is unattached and moves fairly freely inside the spinal canal to accommodate movement of the spine. The end of the spinal cord, called the filum terminale, attaches to the tail end of the spine, called the coccyx. Certain movements of the spine, such as flexion stretch and strain the cord somewhat. Abnormal curvatures of the spine stretch and strain the spine that much more and thus deform the cord and brainstem.
Scoliosis is an abnormal sidewards curvature of the spine. It is typically thought of as a childhood condition but adults can get scoliosis as well. A thoracolumbar scoliosis affects the thoracic and lumbar spines. The thoracic spine is attached to the ribcage. The lumbar spine is the low back.
A double major scoliosis starts in the low back and pelvis and bends one way and then reverses itself and bends the other way in the thoracic spine. The thought is the second curve is to help balance the head on the spine. This may not be the case all the time. The x-ray above is of a young female not quite seventeen. It is a perfect example of a double major scoliosis. The x-ray was contributed to Wikimedia by the University of Utah Hospital Department of Radiology from a case in 2009.
 In most cases the cause of childhood scoliosis is unknown but it affects females far more than it does males. In this regard there is also a connection of scoliosis to tethered cord syndromes. In tethered cord the spinal cord is genetically too short for the length of the spine. This creates a strain putting tension on the cord, which causes a downward traction on the brainstem.
In most cases the cause of childhood scoliosis is unknown but it affects females far more than it does males. In this regard there is also a connection of scoliosis to tethered cord syndromes. In tethered cord the spinal cord is genetically too short for the length of the spine. This creates a strain putting tension on the cord, which causes a downward traction on the brainstem.
Compared to males, females finish developing neurologically much earlier than males. The body, however, can continue to grow and outgrow the length of the cord. It makes sense that the normal growth of the spine could be restrained by the tension caused by the cord thus resulting in a scoliosis. This could explain why tall females seem to be somewhat more susceptible to scoliosis.
In addition to tethered cords, scoliosis can also alter the normal position of the brain within the cranial vault. Tethered cords for example pull the brain down toward the foramen magnum and base of the skull. Head tilts and twists due to scoliosis, likewise, alter the normal alignment of the brain on top of the spine and inside the cranial vault. It is not surprising then, that scoliosis is also associated with Chiari malformations in which the cerebellum is dislocated to a position out of the posterior fossa and into the foramen magnum.
Adults can acquire scoliosis later in life due to injuries and degeneration of the spine such as from arthritis or osteoporosis. Parkinson’s disease also affects the normal alignment of the spine causing it to bend forward into flexion. Rheumatoid arthritis can cause severe destruction of the spine and subsequent scoliosis. Tethered cords can also be caused in adults by injuries and scar tissue inside the spinal canal that restrict the normal movement of the cord.
In addition to scoliosis, kyphosis is an abnormal backwards curve in the spine. Parkinson’s disease and osteoporosis can cause kyphosis. Some people are born with a kyphosis. Kyphosis of the cervical spine can occur as a result of whiplash injuries. Kyphosis, like scoliosis, alters the normal course of blood vessels. It can also create tension in the cord similar to scoliosis when it tethers the cord.
In addition to Chiari malformations and tethered cords, scoliosis and kyphosis alter the normal course of blood vessels and cerebrospinal fluid (CSF) pathways and can thus affect blood and CSF flow. Scoliosis and kyphosis most likely play a significant role in chronic cerebrospinal venous insufficiency, better known as CCSVI. It’s another topic I will cover in the future.
To get a better picture of the potential impact of scoliosis, Chiari malformation, and tethered cord on the brainstem and cerebellum in the posterior fossa click on the following link http://www.upright-health.com/posterior-fossa-chiari.html .
This post is about the impact of scoliosis on the contents of the posterior fossa of the skull, which includes the drainage system of the brain. Abnormal curvatures in the spine alter the normal alignment and relationship of the head and spine, and as a result, the normal relationship of the brain and cord. Curvatures also alter their circulatory routes.
While there may be an attachment of the covering of the upper cord to the foramen magnum, for the most part, the brain is unattached and floats freely inside compartments within the cranial vault. Similarly, the spinal cord is unattached and moves fairly freely inside the spinal canal to accommodate movement of the spine. The end of the spinal cord, called the filum terminale, attaches to the tail end of the spine, called the coccyx. Certain movements of the spine, such as flexion stretch and strain the cord somewhat. Abnormal curvatures of the spine stretch and strain the spine that much more and thus deform the cord and brainstem.
Scoliosis is an abnormal sidewards curvature of the spine. It is typically thought of as a childhood condition but adults can get scoliosis as well. A thoracolumbar scoliosis affects the thoracic and lumbar spines. The thoracic spine is attached to the ribcage. The lumbar spine is the low back.
A double major scoliosis starts in the low back and pelvis and bends one way and then reverses itself and bends the other way in the thoracic spine. The thought is the second curve is to help balance the head on the spine. This may not be the case all the time. The x-ray above is of a young female not quite seventeen. It is a perfect example of a double major scoliosis. The x-ray was contributed to Wikimedia by the University of Utah Hospital Department of Radiology from a case in 2009.
 In most cases the cause of childhood scoliosis is unknown but it affects females far more than it does males. In this regard there is also a connection of scoliosis to tethered cord syndromes. In tethered cord the spinal cord is genetically too short for the length of the spine. This creates a strain putting tension on the cord, which causes a downward traction on the brainstem.
In most cases the cause of childhood scoliosis is unknown but it affects females far more than it does males. In this regard there is also a connection of scoliosis to tethered cord syndromes. In tethered cord the spinal cord is genetically too short for the length of the spine. This creates a strain putting tension on the cord, which causes a downward traction on the brainstem.Compared to males, females finish developing neurologically much earlier than males. The body, however, can continue to grow and outgrow the length of the cord. It makes sense that the normal growth of the spine could be restrained by the tension caused by the cord thus resulting in a scoliosis. This could explain why tall females seem to be somewhat more susceptible to scoliosis.
In addition to tethered cords, scoliosis can also alter the normal position of the brain within the cranial vault. Tethered cords for example pull the brain down toward the foramen magnum and base of the skull. Head tilts and twists due to scoliosis, likewise, alter the normal alignment of the brain on top of the spine and inside the cranial vault. It is not surprising then, that scoliosis is also associated with Chiari malformations in which the cerebellum is dislocated to a position out of the posterior fossa and into the foramen magnum.
Adults can acquire scoliosis later in life due to injuries and degeneration of the spine such as from arthritis or osteoporosis. Parkinson’s disease also affects the normal alignment of the spine causing it to bend forward into flexion. Rheumatoid arthritis can cause severe destruction of the spine and subsequent scoliosis. Tethered cords can also be caused in adults by injuries and scar tissue inside the spinal canal that restrict the normal movement of the cord.
In addition to scoliosis, kyphosis is an abnormal backwards curve in the spine. Parkinson’s disease and osteoporosis can cause kyphosis. Some people are born with a kyphosis. Kyphosis of the cervical spine can occur as a result of whiplash injuries. Kyphosis, like scoliosis, alters the normal course of blood vessels. It can also create tension in the cord similar to scoliosis when it tethers the cord.
In addition to Chiari malformations and tethered cords, scoliosis and kyphosis alter the normal course of blood vessels and cerebrospinal fluid (CSF) pathways and can thus affect blood and CSF flow. Scoliosis and kyphosis most likely play a significant role in chronic cerebrospinal venous insufficiency, better known as CCSVI. It’s another topic I will cover in the future.
To get a better picture of the potential impact of scoliosis, Chiari malformation, and tethered cord on the brainstem and cerebellum in the posterior fossa click on the following link http://www.upright-health.com/posterior-fossa-chiari.html .
Spondylosis, Stenosis, Cog Fog and Dementia

Dementia is a loss of cognitive ability, such as loss of memory, concentration, language and problem solving. Dementia is seen in many neurodegenerative diseases including Alzheimer’s and Parkinson’s disease. Furthermore, cog fog is a common complaint among multiple sclerosis patients. Cog fog is simply a milder form of cognitive impairment compared to what is commonly considered to be dementia. In any case, dementia and cog fog may share similar causes.
The x-ray on the left is a lateral (side) view of a fairly normal cervical spine. The bones, cartilage and joints are all normal in size, shape and spacing. The gray spaces are the discs made of cartilage, and posterior to them are the facets or joints that separate the vertebral segments of the spine.
There are many different types of inherited disorders that can affect the normal design of the base of the skull and cervical spine and thus impair blood and cerebrospinal fluid (CSF) flow in the brain and cord. They fall into categories called: craniosynostosis, craniodyostosis and craniocervical junction abnormalities, which is the base of the skull and upper cervical spine. One of the first types of inherited disorders of connective tissues I studied when I began my research is a condition called craniocleidodysostosis. It is a very rare condition in which cartilage in an infant fails to turn into bone resulting in significant deformation of the skull, clavicals and spine among other things. I also grew up witnessing first hand the impact of severe rheumatoid arthritis on the upper cervical spine and the serious neurological consequences it can have. Both my mother and her mother, my grandmother died quite young due to complications including a slipped odontoid process of the second cervical vertebra (C2) called axis. Rheumatoid arthritis is also considered to be an inherited disorder of connective tissues. The inflammatory arthritides are a separate subject I cover at another time.
In addition to inherited disorders, even more people are affected by acquired disorders due to diseases such as rheumatoid arthritis mentioned above, psoriatic arthritis, lupus erythematosis and osteoarthritis to name just a few. Lastly, everyone is affected by degeneration of the spine due to injuries and aging. Diseases and trauma simply speed up the process and generally make it worse. Inherited disorders tend to show up early in life because of the design flaws. Conditions related to trauma show up later, in midlife, and conditions related to aging degeneration tend to show up late in life. In brief, I categorize all of the different conditions collectively under the umbrella term craniocervical syndromes. The list of craniocervical syndromes is long. Although the different types of craniocervical syndromes are rare by themselves, collectively they affect many people.
 Degeneration of the cervical spine is called spondylosis. This lateral view x-ray of the neck shows spondylosis in the lower cervical spine. If you look at the gray spaces between the bones and compare it to the picture above you will see that they are much thinner. As mentioned above, the gray spaces are the cartilage or discs of the spine. The bones show distortion on the front side and are less square with pointed edges due to compression that caused their inner support structures to collapse.
Degeneration of the cervical spine is called spondylosis. This lateral view x-ray of the neck shows spondylosis in the lower cervical spine. If you look at the gray spaces between the bones and compare it to the picture above you will see that they are much thinner. As mentioned above, the gray spaces are the cartilage or discs of the spine. The bones show distortion on the front side and are less square with pointed edges due to compression that caused their inner support structures to collapse.When the bones, cartilage and connective tissues of the spine, such as the ligaments degenerate they sometimes bulge and buckle backward which invades the space of the spinal canal and outlets for the spinal nerves. Technically it’s called stenosis. Stenosis means narrowing. When it becomes severe enough stenosis can compress the nerve roots and cord causing neurological signs and symptoms. It may even lead to dementia.
More and more evidence is starting to link head injuries to Alzheimer’s disease, Parkinson’s disease and dementia. Controversy, likewise, continues to surround the role of trauma in multiple sclerosis. Research has come a long way in understanding traumatic brain injuries which occur immediately after the trauma. In contast to traumatic brain injuries that occur at the time of the accident the symptoms of cog fog and dementia start to show up many years, sometimes decades later even when they are from the same cause.
In this regard, head and neck injuries often occur together. Unless it is fractured, the skull is oftentimes undamaged. The bones, cartilage and connective tissues of the spine, however, are much more vulnerable to serious strains and sprains that can initiate the degenerative process. In contrast to nerves, the hard and soft tissues of the spine breakdown slowly over years, which leads to spondylosis.
 The brain scan on the left is a perfect example of spondylosis. The cord is the long gray tube that drops down from the brainstem. The white area is blood and cerebrospinal fluid. If you look down at the lower cervical spine you can see that the white area is indented. The indentations are caused by degeneration of the bones, cartilage and connective tissues that spread into the spinal canal and if severe enough, compress the cord.
The brain scan on the left is a perfect example of spondylosis. The cord is the long gray tube that drops down from the brainstem. The white area is blood and cerebrospinal fluid. If you look down at the lower cervical spine you can see that the white area is indented. The indentations are caused by degeneration of the bones, cartilage and connective tissues that spread into the spinal canal and if severe enough, compress the cord.Oftentimes, however, spondylosis compresses the thecal sac of the cord without compressing the cord directly. But the thecal sac contains the vertebral veins of the cord so that compression can lead to what is called venous hypertension, which is an increase in venous pressure.
Acccording to a study done by Rutger’s University, vertebral venous hypertension is one of the most overlooked causes of ischemia of the arterial blood supply to the cord. The arterial blood supply to the cervical cord comes from the vertebral arteries. In this regard, the vertebral arteries also supply the lower inner lobes of the brain, thalamus, hypothalmaus, brainstem and cerebellum. Furthermore, the brain sits further upstream and above the level of the neck making it more susceptible to decreased blood flow from the vertebral arteries due to distance and gravity. Vertebral venous hypertension, that is, back pressure against the vertebral veins, can thus decrease blood flow to the brain the same way it decreases blood flow to the cord by decreasing the pressure gradient. It can also affect the drainage of the brain, as well as CSF flow in the brain and cord, which is closely connected to venous flow.
The health of the cervical spine is important to the health of the brain. Cervical spondylosis and stenosis may play a role in chronic edema, ischemia and normal pressure hydrocephalus. It may also play a role in cog fog and dementia.
For further information on head injuries and dementia check out the following links: dementia and Parkinson’s, Dementia and Neck Injuries
Craniocervical Syndromes, EDS and MS
There are many different types of inherited and acquired disorders, as well as degenerative conditions (aging and wear and tear) of the cervical spine, especially the upper cervical spine (skull and upper cervical spine). I refer to them as craniocervical syndromes in my book. Craniocervical syndromes can cause and array of neurological signs and symptoms related to the brain and cord.
Craniocervical syndromes cause problems by compressing blood and cerebrospinal fluid pathways going into and out of the brain and cord. They can also cause compressive myelopathy of the cervicomedullary cord; which is compression of the lower brainstem and upper cord. Craniocervical syndromes can thus cause an array of signs and symptoms.
In the brain scan above the cauliflower looking structure, at the lower rear part of the brain, is the cerebellum. In front of and below the cerebellum is a verticle tube-like structure which is the brainstem and cord. At the top of the tube-like structure is a round protruding belly-like part of the brainstem in front of the cerebellum called the pons. Above the pons is the midbrain of the brainstem and below it is the medulla oblongata which is the lowest part of the brainstem that connects to the highest part of the spinal cord. Pons is the Latin word for bridge. The pons was called a bridge because it links the midbrain, cerebellum and medulla of the brainstem together.
In front of the pons and behind a black circular structure (the sphenoid sinus) is a white triangular shaped structure with what could be described as a white cup at the very top. The structure is the clivus of the base of the skull. The cup is the compartment in the skull that contains the pituitary gland, which is the master gland that controls the endocrine system. The very bottom of the clivus is the front side of the foramen magnum. This is a large opening in the base of the skull to accommodate the brainstem and cord. Across from it and under the cerebellum (cauliflower) is a thin white strip which is part of the occipital bone that forms the rear of the foramen magnum.
Just below the bottom of the clivus on the front side of the foramen magnum is a white peg-like structure with a black line shaped like a cap over it. The peg-like structure is the dens or odontoid part of the second cervical vertebra below the skull. The dens sits in a pocket of the atlas or first cervical vertebra. The dens is a pivot joint for left and right rotation of the neck. The black line, in front and back of the dens, is fluid that lubricates the joint. A ligament holds the dens in place inside the atlas formed pocket and keeps it from moving posteriorly (back) causing it to compress the spinal cord.
 The cerebellum sits in its own compartment called the posterior fossa. The dark shadow above the cerebellum is the tent-like covering over the posterior fossa called the tentorium cerebelli. The covering is not flat but angles upward. There is a whole in the covering called the incisura for the brainstem to pass through to the foramen magnum and cord below. In the graphic picture on the left, the green area is the right half of the tentorium cerebelli that covers the cerebellum in the posterior fossa below. It divides the brain into upper and lower comparments. The light red area represents the falx cerebri, which is a vertical curtain of connective tissue similar to the tentorium that divides the brain into left and right halves. A similar vertical curtain of connective tissue, called the falx cerebelli, also separtes the posterior fossa and cerebellum into left and right sides.
The cerebellum sits in its own compartment called the posterior fossa. The dark shadow above the cerebellum is the tent-like covering over the posterior fossa called the tentorium cerebelli. The covering is not flat but angles upward. There is a whole in the covering called the incisura for the brainstem to pass through to the foramen magnum and cord below. In the graphic picture on the left, the green area is the right half of the tentorium cerebelli that covers the cerebellum in the posterior fossa below. It divides the brain into upper and lower comparments. The light red area represents the falx cerebri, which is a vertical curtain of connective tissue similar to the tentorium that divides the brain into left and right halves. A similar vertical curtain of connective tissue, called the falx cerebelli, also separtes the posterior fossa and cerebellum into left and right sides.
The posterior fossa and upper cervical spine are critical to blood and CSF flow and contain some of the most crucial components of the brain and cord. Many conditions affect the upper cervical spine and base of the skull predisposing humans to neurodegenerative conditions and subsequent diseases. This is due to the unique design of the skull, spine and circulatory system of the brain and cord as a result of upright posture.
One genetic condition in particular underscores the role of craniocervical syndromes in neurodegenerative conditions due to it’s design flaws. That condition is Ehlers-Danlos syndrome or EDS. Even the short version of EDS is far too long to discuss here but is discussed on my website. In brief, certain cases of Ehlers-Danlos Syndrome (EDS) affect the design of the skull and some affect the upper cervical spine resulting in Chiari malformations and hydrocephalus type condtions among other things.
I will discuss other craniocervical syndromes that can cause similar problems as the website develops. The design of the base of the skull and upper cervical spine needs to be studied much further. It may be a key culprit in many neurodegenerative conditions. Upright MRI will shed much more light on this in the future.
For additional information on this and other related topics as well as my book go to my website at www.upright-health.com.
Craniocervical syndromes cause problems by compressing blood and cerebrospinal fluid pathways going into and out of the brain and cord. They can also cause compressive myelopathy of the cervicomedullary cord; which is compression of the lower brainstem and upper cord. Craniocervical syndromes can thus cause an array of signs and symptoms.
In the brain scan above the cauliflower looking structure, at the lower rear part of the brain, is the cerebellum. In front of and below the cerebellum is a verticle tube-like structure which is the brainstem and cord. At the top of the tube-like structure is a round protruding belly-like part of the brainstem in front of the cerebellum called the pons. Above the pons is the midbrain of the brainstem and below it is the medulla oblongata which is the lowest part of the brainstem that connects to the highest part of the spinal cord. Pons is the Latin word for bridge. The pons was called a bridge because it links the midbrain, cerebellum and medulla of the brainstem together.
In front of the pons and behind a black circular structure (the sphenoid sinus) is a white triangular shaped structure with what could be described as a white cup at the very top. The structure is the clivus of the base of the skull. The cup is the compartment in the skull that contains the pituitary gland, which is the master gland that controls the endocrine system. The very bottom of the clivus is the front side of the foramen magnum. This is a large opening in the base of the skull to accommodate the brainstem and cord. Across from it and under the cerebellum (cauliflower) is a thin white strip which is part of the occipital bone that forms the rear of the foramen magnum.
Just below the bottom of the clivus on the front side of the foramen magnum is a white peg-like structure with a black line shaped like a cap over it. The peg-like structure is the dens or odontoid part of the second cervical vertebra below the skull. The dens sits in a pocket of the atlas or first cervical vertebra. The dens is a pivot joint for left and right rotation of the neck. The black line, in front and back of the dens, is fluid that lubricates the joint. A ligament holds the dens in place inside the atlas formed pocket and keeps it from moving posteriorly (back) causing it to compress the spinal cord.
 The cerebellum sits in its own compartment called the posterior fossa. The dark shadow above the cerebellum is the tent-like covering over the posterior fossa called the tentorium cerebelli. The covering is not flat but angles upward. There is a whole in the covering called the incisura for the brainstem to pass through to the foramen magnum and cord below. In the graphic picture on the left, the green area is the right half of the tentorium cerebelli that covers the cerebellum in the posterior fossa below. It divides the brain into upper and lower comparments. The light red area represents the falx cerebri, which is a vertical curtain of connective tissue similar to the tentorium that divides the brain into left and right halves. A similar vertical curtain of connective tissue, called the falx cerebelli, also separtes the posterior fossa and cerebellum into left and right sides.
The cerebellum sits in its own compartment called the posterior fossa. The dark shadow above the cerebellum is the tent-like covering over the posterior fossa called the tentorium cerebelli. The covering is not flat but angles upward. There is a whole in the covering called the incisura for the brainstem to pass through to the foramen magnum and cord below. In the graphic picture on the left, the green area is the right half of the tentorium cerebelli that covers the cerebellum in the posterior fossa below. It divides the brain into upper and lower comparments. The light red area represents the falx cerebri, which is a vertical curtain of connective tissue similar to the tentorium that divides the brain into left and right halves. A similar vertical curtain of connective tissue, called the falx cerebelli, also separtes the posterior fossa and cerebellum into left and right sides.The posterior fossa and upper cervical spine are critical to blood and CSF flow and contain some of the most crucial components of the brain and cord. Many conditions affect the upper cervical spine and base of the skull predisposing humans to neurodegenerative conditions and subsequent diseases. This is due to the unique design of the skull, spine and circulatory system of the brain and cord as a result of upright posture.
One genetic condition in particular underscores the role of craniocervical syndromes in neurodegenerative conditions due to it’s design flaws. That condition is Ehlers-Danlos syndrome or EDS. Even the short version of EDS is far too long to discuss here but is discussed on my website. In brief, certain cases of Ehlers-Danlos Syndrome (EDS) affect the design of the skull and some affect the upper cervical spine resulting in Chiari malformations and hydrocephalus type condtions among other things.
I will discuss other craniocervical syndromes that can cause similar problems as the website develops. The design of the base of the skull and upper cervical spine needs to be studied much further. It may be a key culprit in many neurodegenerative conditions. Upright MRI will shed much more light on this in the future.
For additional information on this and other related topics as well as my book go to my website at www.upright-health.com.
Posted in ccsvi, chiari malformations, Devic's disease, Ehlers Danlos Syndrome, multiple sclerosis, optic spinal multiple sclerosis, physical anthropology Tagged Arnold–Chiari malformation, Base of skull, Brainstem, Cervical vertebrae, Ehlers–Danlos syndrome, Foramen magnum, Posterior cranial fossa, Spinal cord 2 Comments
C1, C2 and CSF Flow
The picture on the left is from promotional material for Fonar Corporation’s upright MRI. In this regard, my theory is that humans are predisposed to neurodegenerative diseases such as Alzheimer’s, Parkinson’s and multiple sclerosis due to the unique design of the skull, spine and circulatory system of the brain as a result of upright posture. In addition to blood flow, upright posture also changes CSF flow. Besides its added benefit in many other health conditions, when it comes to blood and CSF flow, upright MRI is the wave of the future in brain research.
Cerebrospinal fluid (CSF) flow is called the third circulation of the brain and it is the least understood. CSF production and flow is critical to brain cushioning and protection. In terms of protection CSF is important to brain support to prevent the brain from sinking in the cranial vault. Conversely, excess CSF volume compresses the brain.
CSF comes from arterial blood that has been filtered through the blood brain barrier to the point where it is mostly water. CSF leaves the brain through the venous system. Therefore, backups in the venous drainage system affect cerebrospinal fluid (CSF) flow and drainage. Although it uses other routes as well, such as cranial and spinal nerves and the lymphatic system, most of the cerebrospinal fluid (CSF) produced by the brain eventually makes its way up to the superior sagittal sinus where it empties into the venous system.
The superior sagittal sinus, depicted in the graphic image on the right, is the largest dural sinus located at the top of the brain. The superior sagittal sinus contains arachnoid granulations that act as one way check valves for the flow of CSF from the subarachnoid space to the sinus. Click on the image for a better view. The pulsatile nature and the pressure generated by the CSF outflow through the arachnoid granulations is powerful enough to scour impressions into the roof of the cranial vault.Cerebrospinal fluid (CSF) flow is called the third circulation of the brain and it is the least understood. CSF production and flow is critical to brain cushioning and protection. In terms of protection CSF is important to brain support to prevent the brain from sinking in the cranial vault. Conversely, excess CSF volume compresses the brain.
CSF comes from arterial blood that has been filtered through the blood brain barrier to the point where it is mostly water. CSF leaves the brain through the venous system. Therefore, backups in the venous drainage system affect cerebrospinal fluid (CSF) flow and drainage. Although it uses other routes as well, such as cranial and spinal nerves and the lymphatic system, most of the cerebrospinal fluid (CSF) produced by the brain eventually makes its way up to the superior sagittal sinus where it empties into the venous system.
About sixty percent of the CSF produced in the brain ends up in the spinal cord. Eventually most of the CSF in the spinal cord makes its way back up through the subarachnoid space of the cord and into the subarchnoid space of the brain. From there it travels up to the superior sagittal sinus and arachnoid granulations to exit the brain along with venous blood.
The movement of CSF is driven by cardiovascular waves arising from the heart and blood vessels. During the contraction phase of the heart cycle (systole) pressure in the arteries of the brain increases. The increase in blood pressure drives CSF out of the brain through the upper cervical spine because as blood volume rises CSF volume must decrease. During the relaxation phase (diastole) the pressure drops and CSF enters the cranial vault through the subarachnoid space of the upper cervical spine. In addition, because the veins of the vertebral venous plexus of the spine have no valves, respiratory pressure changes are transmitted to the brain and amplify the cardiovascular waves. In brief, as pressure in the chest cavity drops during inspiration, due to the diaphram moving down and the chest wall moving out, CSF is pulled out of the cranial vault. As pressure in the chest cavity increases during exhalation CSF is driven into the cranial cavity. Thus, combined cardiorespiratory waves are important to the movement of CSF through the brain and cord.
The CSF that leaves the brain on its way down to the cord , however, must first pass through the tight neural (spinal) canal of the the upper cervical spine. Likewise, on its return trip back to the brain, it must again pass through the neural canal of the upper cervical spine. Therefore, the upper cervical spine is a critical link in the flow of CSF between the subarachnoid space of the brain and the cord. Under normal circumstances cardiorespiratory waves move CSF through the neural canal of the upper cervical spine unimpeded with good pulsatility and continue to drive it through the subarachnoid space up to the superior sagittal sinus.
Genetic design flaws, such as Chiari malformations, and acquired disorders from injuries or disease can impede the pulsatility and flow of CSF through the upper cervical spine. Restrictions in CSF flow that cause a decrease in its volume, can, in turn, cause Chiari malformations and pressure conus conditions. Furthermore, any condition that restricts CSF flow can lead to hydrocephalus-like conditions. It is therefore important to maintain the correct volume of CSF in order to provide sufficient brain support and protection, as well as to prevent hydrocephalus.
The picture above shows a fairly severe rotational misalignment of the upper cervical spine to the right. Click on the image for a better view. The dart shaped structure in the upper cervical spine is the spinous process of C2. It should be in the midline. The misalignment was caused by a motorcycle accident in which the victim landed on the right side of his head causing his head to snap to the left while simultaneously shifting and twisting his upper cervical spine to the right. Misalignments, such as the one above (due to micro or macro trauma), genetic design flaws (Chiari malformations), diseases (rheumatoid arthritis) and degenerative conditons (aging) of the upper cervical spine can affect the vertebral arteries that supply the brain, as well as the vertebral veins that drain the brain during upright posture. They can also cause deformation of the subarachnoid space and consequently, they can affect CSF flow going into and out of the brain and cord.
While CCSVI treatment can improve venous drainage, which may further relieve hydrocephalic conditions in certain cases, it cannot improve CSF flow through the subarachnoid space of the upper cervical spine. Furthermore, increasing venous drainage of the brain and consequently decreasing CSF volume without a proportionate rise in passive CSF production could compromise brain support causing it to sink in the vault resulting in a condition similar to a pressure conus or Chiari malformation. Over drainage of the brain may thus present problems similar to spinal taps which can cause headaches due to a pressure conus condition following CSF removal. Over drainage is probably less likely in younger cases where the passive CSF pressure gradient and CSF production remains strong. Older patients, on the other hand, may have a lower CSF pressure gradient and thus a decrease in passive production of CSF due to aging of the brain and chronic craniocervical back pressure against the vertebral veins and subarachnoid space.
The flow of CSF clearly plays a role in normal pressure hydrocephalus (NPH), which has been associated with Alzheimer’s and Parkinson’s disease. It also plays a role in Chiari malformations, which cause signs and symptoms similar to MS. I discuss CSF production and flow thoroughly in my book. I will be discussing it more here in future posts as well as on my new website at: http://www.upright-health.com/.
Chiari Malformations and Cranial Nerves
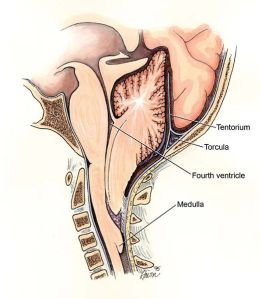 Chiari malformations are typically associated with herniation of the brainstem into the foramen magnum in the base of the skull as shown in the picture on the left. More recently, it has come to include what is called a Zero Chiari Malformation in which the cerebellum comes in contact with the base of the cranial vault without herniation into the foramen magnum. This has prompted some researchers to suggest that Chiari malformations include any decrease in cerebrospinal fluid volume (CSF) sufficient enough to cause the brain to sink and come in contact with the bones of the base of the skull.
Chiari malformations are typically associated with herniation of the brainstem into the foramen magnum in the base of the skull as shown in the picture on the left. More recently, it has come to include what is called a Zero Chiari Malformation in which the cerebellum comes in contact with the base of the cranial vault without herniation into the foramen magnum. This has prompted some researchers to suggest that Chiari malformations include any decrease in cerebrospinal fluid volume (CSF) sufficient enough to cause the brain to sink and come in contact with the bones of the base of the skull.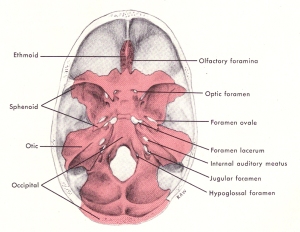 Considering the above, in addition to the foramen magnum there are other large holes in the base of the skull through which cranial nerves and blood vessels pass, as seen in the picture on the right. It is possible that the cranial nerves may herniate into the openings or come in contact with the base of the skull due to Chiari malformations in which the volume of CSF falls too low, as mentioned above. The consequence would be similar, as well, that is cause compression of nerves and circulatory routes.
Considering the above, in addition to the foramen magnum there are other large holes in the base of the skull through which cranial nerves and blood vessels pass, as seen in the picture on the right. It is possible that the cranial nerves may herniate into the openings or come in contact with the base of the skull due to Chiari malformations in which the volume of CSF falls too low, as mentioned above. The consequence would be similar, as well, that is cause compression of nerves and circulatory routes. The brain floats within the cranial vault. Typically, it is prevented from sinking into the foramen magnum by the cisterns of the brain which are filled with cerebrospinal fluid (CSF). The cisterns are also strategically placed to provide cushioning, support and protection from the hard bones of the cranial vault as seen in the picture on the left.
The brain floats within the cranial vault. Typically, it is prevented from sinking into the foramen magnum by the cisterns of the brain which are filled with cerebrospinal fluid (CSF). The cisterns are also strategically placed to provide cushioning, support and protection from the hard bones of the cranial vault as seen in the picture on the left.Symptoms of MS often include cranial nerves. Common complaints include dizziness, ringing in the ears or loss of hearing, trigeminal neuralgia, burning tongue and dry mouth. By far, however, the cranial nerve most commonly involved in MS is the optic nerve. Optic neuritis is, in fact, one of the most frequent symptoms of MS. Even Asians and African-Americans who, otherwise, have a much lower incidence of MS, get optic neuritis. They also get transverse myelitis, but that’s another topic entirely. I will be covering the different cranial nerve signs, as well as transverse myelitis on my new website starting with the optic nerve.
The optic nerve is the second most superior (highest) nerve in the cranial vault. The highest cranial nerve is the olfactory nerve to the nose which is located in the anterior fossa or forehead area of the base of the skull. The optic nerve lies in the middle fossa behind the eye sockets. Most of the cranial nerves are in the posterior fossa along with the brainstem and cerebellum.
It’s position in the cranial vault and the optic canal may be the reason why optic neuritis is one of the most common signs and symptoms of MS, optic-spinal MS and Devic’s disease. Typically, the optic nerve is protected by the chiasmatic cistern, which is one of the highest cisterns in the brain. Among other things trauma and failure of the CSF support system of the brain may play a role in optic neuritis. For further information on optic neuritis click on the link below to my new website. The website can also be found in the links section of the sidebar under upright-health





No comments:
Post a Comment