Alzheimer's, Parkinson's and Multiple Sclerosis
Getting to the Root Causes of Neurodegnerative Diseases

Dissociation of CSF Flow in Neurodegenerative Diseases
One of the suspected causes of hydrocephalus, associated with neurodegenerative diseases seen in children and adults, is a dissociation of cerebrospinal fluid (CSF) flow between the cranial vault and spinal canal. The term hydrocephalus means water on the brain. Hydrocephalus causes the ventricles to enlarge, which is called ventriculomegaly. The ventricles are chambers in the brain where CSF is produced. Ventriculomegaly can be caused by anything that obstructs the pathways and normal flow of CSF, or it can be caused by inadequate absorption of CSF described below. In children, hydrocephalus is associated with high presssure in the brain called intracranial pressure. The high intracranial pressure, however, may be due to the open joints of the skull in a child, which provide less resistance to CSF pressure. The combination of high intracranial pressure and open joints in the skull causes the head to enlarge.
Normal pressure hydrocephalus (NPH) is a condition seen in adults in which the CSF volume increases and the ventricles enlarge but intracranial pressure remains normal or just slightly elevated. The size of the head, likewise, remains normal due to the closed joints of the skull. More than likely, the closed joints of the adult skull act like a counter-weight on a pressure cooker and limit CSF pressure inside the cranial vault. This will be discussed further in future posts. NPH and ventriculomegaly in adults can be caused by conditions such as traumatic brain injuries, subarachnoid hemorrhage (bleeding), prior intracranial surgery, and meningitis (inflammation of the protective coats called meninges). Most cases of NPH, however, are unknown.
 The brain scan on the right is of an adult patient with NPH. NPH is typically associated with ventriculomegaly without atrophy (shrinkage) of the brain. Atrophy is seen as a widening of the spaces of the brain called fissures and sulci (dark spaces between the folds in the picture) that separate the gyri and folds of the different lobes. Ventriculomegaly is usually found around the frontal and temporal horns of the lateral ventricles.
The brain scan on the right is of an adult patient with NPH. NPH is typically associated with ventriculomegaly without atrophy (shrinkage) of the brain. Atrophy is seen as a widening of the spaces of the brain called fissures and sulci (dark spaces between the folds in the picture) that separate the gyri and folds of the different lobes. Ventriculomegaly is usually found around the frontal and temporal horns of the lateral ventricles.
In adults, NPH and enlarged lateral ventricles have been associated with Alzheimer’s and Parkinson’s disease, as well as dementia, schizophrenia, bipolar disorder, Parkinson’s Plus, Huntington’s disease and other neurodegenerative conditions for decades. More recently, enlargement of the third ventricle has been associated with multiple sclerosis. The fourth ventricle is sometimes enlarged in a condition called multisystem atrophy (MSA), which is a variant of Parkinson’s disease. MSA will be discussed further below.
In the brain scan above, the black arrows point to the lateral ventricles, which are seen as the large black spaces in the core of the brain. The ventricles are part of the brain. They are surrounded by the lobes, diencephalon (thalamus and hypothalamus) and brainstem and contain CSF. The corpus callosum forms the roof of the lateral ventricles and is seen as the white rim over the black space. The white rim below the lateral ventricles is called the fornix which sits over the roof of the third ventricle. As in this case, NPH often causes the corpus callosum to bow upward, and compress the outer cortex of the brain against the inner surface of the skull. White matter lesions are often present in the periventricular areas that surround the lateral ventricles. Periventricular white matter lesions are also seen in MS.
CSF flows from the lateral ventricles into the third and then the fourth ventricle. After leaving the fourth ventricle CSF flows into the cisterns. The cisterns are not part of the body of the brain called the parenchyma. Instead, they are part of the subarachnoid space that surrounds the brain. The subarachnoid space is a network of tunnels formed in the protective outer coats of the brain called meninges. The cisterns are seen in the brain scan above as the black spaces located around the brainstem and beneath the cerebellum (cauliflower-like structure in the lower rear of the skull). In this particular case, the fourth ventricle, seen in front of the cerebellum, is enlarged as is the space below it which is called the cisterna magna. The white arrow points to the cerebral aqueduct which is also enlarged. The cerebral aqueduct is a canal that connects the third ventricle to the fourth ventricle. The third ventricle is the dark space beneath the lateral ventricles. Some researchers now suggest that the term hydrocephalus should include an increase in CSF volume outside the ventricles as well, such as in the cisterns and the subarachnoid spaces.
 CSF from the fourth ventricle drains into the pontine cistern, the cisterna magna and the central canal of the spinal cord. The pontine cistern is the black space in front of the brainstem (the long white structure). The pons is the part of the brainstem that sticks out toward the face like a big round potbelly. The cisterna magna is the black space beneath the cerebellum.
CSF from the fourth ventricle drains into the pontine cistern, the cisterna magna and the central canal of the spinal cord. The pontine cistern is the black space in front of the brainstem (the long white structure). The pons is the part of the brainstem that sticks out toward the face like a big round potbelly. The cisterna magna is the black space beneath the cerebellum.
The central canal of the cord is not seen in this image. The connection between the fourth ventricle and the central canal will be covered separately as it relates to a type of hydrocephalus in the cord called hydromyelia or syringomyelia. Sometimes they are simply referred to as a syrinx. For now suffice it to say, they are abnormal cavities in the cord that are probably caused by pressure problems within the cord, similar to hydrocephalus which is due to pressure problems in the brain.
After entering the cisterns, CSF can flow down into the subarachnoid space of the spinal cord or it can flow upward through the subarachnoid space of the brain to the arachnoid granulations at the top of the brain, where the bulk of CSF absorption takes place to eventually leave the central nervous system via the venous system. The arachnoid granulations are one-way valves that connect the subarachnoid space to the superior sagittal sinus. The superior sagittal sinus is part of the venous drainage system of the brain located at the top of the skull.
The MRI above on the left is of a patient with a condition called multisystem atrophy. Multisystem atrophy is a variant of Parkinson’s disease, which also includes olivopontocerebellar atrophy. It is also known as Shy-Drager Syndrome. Among other things, multisystem atrophy is associated with dysautonomia and orthostatic hypotension in which blood pressure drops when changing position from sitting to standing. Dysautonomia is a malfunction of the autonomic nervous system that controls automatic internal operations such as heartbeat, circulation, respiration, temperature regulation, bladder and bowel control and more. In addition to Parkinson’s and multisystem atrophy, signs and symptoms of dysautonomia are common in Alzheimer’s disease and multiple sclerosis.
As can be seen in the brain scan above, in addition to enlargement of the fourth ventricle, multisystem atrophy is also associated with enlargement of the cisterns that surround, cushion and support the brainstem and cerebellum. In this regard, it looks similar to the MRI in the case with NPH at the top of the page. The difference is, the lateral ventricles aren’t enlarged. On the other hand, NPH is more typically associated with enlarged lateral ventricles but not enlarged cisterns. In this case the front of the pons (potbelly) appears slightly compressed due to the enlargement of the pontine cistern.
 The brain scan on the right is of a child with a condition called Dandy-Walker Syndrome, which looks somewhat similar to the multisystem atrophy scan above. Here the fourth ventricle (the dark space in front of the cerebellum) and the prepontine cistern (the dark space in front of the cord) aren’t enlarged as above. Only the cisterna magna below the cerebellum is enlarged, which is called mega cisterna magna. Some cases of Dandy-Walker syndrome have enlarged ventricles, hydrocephalus and a mega cisterna magna. According to the classic definition, a mega cisterna magna alone, without ventriculomegaly, isn’t classified as hydrocephalus.
The brain scan on the right is of a child with a condition called Dandy-Walker Syndrome, which looks somewhat similar to the multisystem atrophy scan above. Here the fourth ventricle (the dark space in front of the cerebellum) and the prepontine cistern (the dark space in front of the cord) aren’t enlarged as above. Only the cisterna magna below the cerebellum is enlarged, which is called mega cisterna magna. Some cases of Dandy-Walker syndrome have enlarged ventricles, hydrocephalus and a mega cisterna magna. According to the classic definition, a mega cisterna magna alone, without ventriculomegaly, isn’t classified as hydrocephalus.
The enlarged cisterns and fourth ventricle seen in MSA (Parkinson’s) in adults, and in Dandy-Walker Syndrome in children are usually attributed to atrophy of the brainstem and cerebellum, which are surrounded by cisterns. Likewise, ventriculomegaly seen in neurodegenerative diseases such as Alzheimer’s, Parkinson’s and multiple sclerosis is typically attributed to atrophy of periventricular structures that surround the ventricles. Ventriculomegaly seen in NPH, on the other hand, is typically attributed to enlargement of the ventricles without atrophy of the surrounding tissues and structures. The problem is, the ventricles don’t always return to normal size when excess CSF volume is surgically decreased with a shunt. This led researchers to suggest that, the sustained enlargement of the ventricles may be due to permanent damage to the surrounding periventricular structures as a result of the NPH.
There are two primary theories regarding the origin of NPH. The first theory has to do with obstruction of CSF flow or blockage of resorption into the venous drainage system of the brain discussed above. The other theory is that NPH is due to atrophy of surrounding structures, such as the periventricular white matter that gets strained and tensioned to the point of breaking, causing the walls of the ventricles to weaken and enlarge. Enlargement of the ventricles also stretches, strains and compresses surrounding blood vessels that can decrease blood flow and cause ischemic tissue damage. In either case, the subsequent weakness in the walls of the ventricles and surrounding structures cause the ventricles to enlarge. NPH, in turn, increases tension, tangential and shear stresses in the brain, as well as compression loads caused by expansion and contraction of the brain with each beat of the heart that forces a relatively large volume of fluid into the mostly closed container of the cranial vault.
There is a reason why these different types of ventriculomegaly (hydrocephalus) and mega cisterns seen in children and adults look remarkably similar. It is because they are all related to faulty CSF flow in the brain. Whether it shows up as ventriculomegaly or mega cisterns depends on the location of the obstruction or malabsorption problem. Aside from internal problems in CSF pathways of the brain inside the cranial vault, researchers now suspect that one of the causes of hydrocephalus in children and adults is a dissociation of CSF flow between the cranial vault and spinal canal. Dissociation simply means that the normal flow between the two compartments is disrupted, and as a result they react independantly. Among other things, this can cause potentially destructive abnormal increases in CSF pressure waves in the brain and cord. Dissociation of CSF flow between the two compartments may similarly play a role in hydromyelia and other conditions of the cord.
Upright posture requires proper CSF flow between the cranial and spinal compartments in order to maintain the correct volume, pressure, protection and bouyancy of the brain. Excess CSF volume in the ventricles, cisterns and subarachnoid spaces can cause destructive tension (stretch) and compression loads in the brain. An insufficient volume reduces bouyancy, which causes the brain to sink and make contact with the base of the skull. The connection between the cranial compartment and spinal compartment is in the upper cervical spine. Malformations, injuries and misalignments of the upper cervical spine can cause a dissociation of CSF flow between the cranial and spinal compartment. Further below in the lower spine, spondylosis (degeneration), scoliosis (abnormal curvature) and stenosis (narrowing) alter the design of the spinal canal and thus affect blood and CSF flow. The changes in the design of the spinal canal can, likewise, result in a dissociation of CSF flow between the cranial vault and spinal canal. Thus far, the studies on dissociation of CSF flow between the cranial vault and spinal canal have all been done using supine MRI. Future research will need to be done using upright MRI. Upright MRI will most likely reveal much more about the destructive consequences of dissociation of CSF flow between the cranial vault and spinal canal.
The areas hardest hit by faulty fluid mechanics in the cranial vault are: 1) the periventricular structures that surround the ventricles, 2) the bottom surfaces of the brain, brainstem and cerebellum located above the base of the skull that are surrounded and supported by the cisterns, and 3) the cortex of the brain closest to the inner surface of the skull. The particular areas that are affected are determined by the cause and the consequences of the faulty CSF flow.
For more information on this and other related subjects visit my website at www.upright-health.com.
Normal pressure hydrocephalus (NPH) is a condition seen in adults in which the CSF volume increases and the ventricles enlarge but intracranial pressure remains normal or just slightly elevated. The size of the head, likewise, remains normal due to the closed joints of the skull. More than likely, the closed joints of the adult skull act like a counter-weight on a pressure cooker and limit CSF pressure inside the cranial vault. This will be discussed further in future posts. NPH and ventriculomegaly in adults can be caused by conditions such as traumatic brain injuries, subarachnoid hemorrhage (bleeding), prior intracranial surgery, and meningitis (inflammation of the protective coats called meninges). Most cases of NPH, however, are unknown.
 The brain scan on the right is of an adult patient with NPH. NPH is typically associated with ventriculomegaly without atrophy (shrinkage) of the brain. Atrophy is seen as a widening of the spaces of the brain called fissures and sulci (dark spaces between the folds in the picture) that separate the gyri and folds of the different lobes. Ventriculomegaly is usually found around the frontal and temporal horns of the lateral ventricles.
The brain scan on the right is of an adult patient with NPH. NPH is typically associated with ventriculomegaly without atrophy (shrinkage) of the brain. Atrophy is seen as a widening of the spaces of the brain called fissures and sulci (dark spaces between the folds in the picture) that separate the gyri and folds of the different lobes. Ventriculomegaly is usually found around the frontal and temporal horns of the lateral ventricles.In adults, NPH and enlarged lateral ventricles have been associated with Alzheimer’s and Parkinson’s disease, as well as dementia, schizophrenia, bipolar disorder, Parkinson’s Plus, Huntington’s disease and other neurodegenerative conditions for decades. More recently, enlargement of the third ventricle has been associated with multiple sclerosis. The fourth ventricle is sometimes enlarged in a condition called multisystem atrophy (MSA), which is a variant of Parkinson’s disease. MSA will be discussed further below.
In the brain scan above, the black arrows point to the lateral ventricles, which are seen as the large black spaces in the core of the brain. The ventricles are part of the brain. They are surrounded by the lobes, diencephalon (thalamus and hypothalamus) and brainstem and contain CSF. The corpus callosum forms the roof of the lateral ventricles and is seen as the white rim over the black space. The white rim below the lateral ventricles is called the fornix which sits over the roof of the third ventricle. As in this case, NPH often causes the corpus callosum to bow upward, and compress the outer cortex of the brain against the inner surface of the skull. White matter lesions are often present in the periventricular areas that surround the lateral ventricles. Periventricular white matter lesions are also seen in MS.
CSF flows from the lateral ventricles into the third and then the fourth ventricle. After leaving the fourth ventricle CSF flows into the cisterns. The cisterns are not part of the body of the brain called the parenchyma. Instead, they are part of the subarachnoid space that surrounds the brain. The subarachnoid space is a network of tunnels formed in the protective outer coats of the brain called meninges. The cisterns are seen in the brain scan above as the black spaces located around the brainstem and beneath the cerebellum (cauliflower-like structure in the lower rear of the skull). In this particular case, the fourth ventricle, seen in front of the cerebellum, is enlarged as is the space below it which is called the cisterna magna. The white arrow points to the cerebral aqueduct which is also enlarged. The cerebral aqueduct is a canal that connects the third ventricle to the fourth ventricle. The third ventricle is the dark space beneath the lateral ventricles. Some researchers now suggest that the term hydrocephalus should include an increase in CSF volume outside the ventricles as well, such as in the cisterns and the subarachnoid spaces.
 CSF from the fourth ventricle drains into the pontine cistern, the cisterna magna and the central canal of the spinal cord. The pontine cistern is the black space in front of the brainstem (the long white structure). The pons is the part of the brainstem that sticks out toward the face like a big round potbelly. The cisterna magna is the black space beneath the cerebellum.
CSF from the fourth ventricle drains into the pontine cistern, the cisterna magna and the central canal of the spinal cord. The pontine cistern is the black space in front of the brainstem (the long white structure). The pons is the part of the brainstem that sticks out toward the face like a big round potbelly. The cisterna magna is the black space beneath the cerebellum.The central canal of the cord is not seen in this image. The connection between the fourth ventricle and the central canal will be covered separately as it relates to a type of hydrocephalus in the cord called hydromyelia or syringomyelia. Sometimes they are simply referred to as a syrinx. For now suffice it to say, they are abnormal cavities in the cord that are probably caused by pressure problems within the cord, similar to hydrocephalus which is due to pressure problems in the brain.
After entering the cisterns, CSF can flow down into the subarachnoid space of the spinal cord or it can flow upward through the subarachnoid space of the brain to the arachnoid granulations at the top of the brain, where the bulk of CSF absorption takes place to eventually leave the central nervous system via the venous system. The arachnoid granulations are one-way valves that connect the subarachnoid space to the superior sagittal sinus. The superior sagittal sinus is part of the venous drainage system of the brain located at the top of the skull.
The MRI above on the left is of a patient with a condition called multisystem atrophy. Multisystem atrophy is a variant of Parkinson’s disease, which also includes olivopontocerebellar atrophy. It is also known as Shy-Drager Syndrome. Among other things, multisystem atrophy is associated with dysautonomia and orthostatic hypotension in which blood pressure drops when changing position from sitting to standing. Dysautonomia is a malfunction of the autonomic nervous system that controls automatic internal operations such as heartbeat, circulation, respiration, temperature regulation, bladder and bowel control and more. In addition to Parkinson’s and multisystem atrophy, signs and symptoms of dysautonomia are common in Alzheimer’s disease and multiple sclerosis.
As can be seen in the brain scan above, in addition to enlargement of the fourth ventricle, multisystem atrophy is also associated with enlargement of the cisterns that surround, cushion and support the brainstem and cerebellum. In this regard, it looks similar to the MRI in the case with NPH at the top of the page. The difference is, the lateral ventricles aren’t enlarged. On the other hand, NPH is more typically associated with enlarged lateral ventricles but not enlarged cisterns. In this case the front of the pons (potbelly) appears slightly compressed due to the enlargement of the pontine cistern.
 The brain scan on the right is of a child with a condition called Dandy-Walker Syndrome, which looks somewhat similar to the multisystem atrophy scan above. Here the fourth ventricle (the dark space in front of the cerebellum) and the prepontine cistern (the dark space in front of the cord) aren’t enlarged as above. Only the cisterna magna below the cerebellum is enlarged, which is called mega cisterna magna. Some cases of Dandy-Walker syndrome have enlarged ventricles, hydrocephalus and a mega cisterna magna. According to the classic definition, a mega cisterna magna alone, without ventriculomegaly, isn’t classified as hydrocephalus.
The brain scan on the right is of a child with a condition called Dandy-Walker Syndrome, which looks somewhat similar to the multisystem atrophy scan above. Here the fourth ventricle (the dark space in front of the cerebellum) and the prepontine cistern (the dark space in front of the cord) aren’t enlarged as above. Only the cisterna magna below the cerebellum is enlarged, which is called mega cisterna magna. Some cases of Dandy-Walker syndrome have enlarged ventricles, hydrocephalus and a mega cisterna magna. According to the classic definition, a mega cisterna magna alone, without ventriculomegaly, isn’t classified as hydrocephalus.The enlarged cisterns and fourth ventricle seen in MSA (Parkinson’s) in adults, and in Dandy-Walker Syndrome in children are usually attributed to atrophy of the brainstem and cerebellum, which are surrounded by cisterns. Likewise, ventriculomegaly seen in neurodegenerative diseases such as Alzheimer’s, Parkinson’s and multiple sclerosis is typically attributed to atrophy of periventricular structures that surround the ventricles. Ventriculomegaly seen in NPH, on the other hand, is typically attributed to enlargement of the ventricles without atrophy of the surrounding tissues and structures. The problem is, the ventricles don’t always return to normal size when excess CSF volume is surgically decreased with a shunt. This led researchers to suggest that, the sustained enlargement of the ventricles may be due to permanent damage to the surrounding periventricular structures as a result of the NPH.
There are two primary theories regarding the origin of NPH. The first theory has to do with obstruction of CSF flow or blockage of resorption into the venous drainage system of the brain discussed above. The other theory is that NPH is due to atrophy of surrounding structures, such as the periventricular white matter that gets strained and tensioned to the point of breaking, causing the walls of the ventricles to weaken and enlarge. Enlargement of the ventricles also stretches, strains and compresses surrounding blood vessels that can decrease blood flow and cause ischemic tissue damage. In either case, the subsequent weakness in the walls of the ventricles and surrounding structures cause the ventricles to enlarge. NPH, in turn, increases tension, tangential and shear stresses in the brain, as well as compression loads caused by expansion and contraction of the brain with each beat of the heart that forces a relatively large volume of fluid into the mostly closed container of the cranial vault.
There is a reason why these different types of ventriculomegaly (hydrocephalus) and mega cisterns seen in children and adults look remarkably similar. It is because they are all related to faulty CSF flow in the brain. Whether it shows up as ventriculomegaly or mega cisterns depends on the location of the obstruction or malabsorption problem. Aside from internal problems in CSF pathways of the brain inside the cranial vault, researchers now suspect that one of the causes of hydrocephalus in children and adults is a dissociation of CSF flow between the cranial vault and spinal canal. Dissociation simply means that the normal flow between the two compartments is disrupted, and as a result they react independantly. Among other things, this can cause potentially destructive abnormal increases in CSF pressure waves in the brain and cord. Dissociation of CSF flow between the two compartments may similarly play a role in hydromyelia and other conditions of the cord.
Upright posture requires proper CSF flow between the cranial and spinal compartments in order to maintain the correct volume, pressure, protection and bouyancy of the brain. Excess CSF volume in the ventricles, cisterns and subarachnoid spaces can cause destructive tension (stretch) and compression loads in the brain. An insufficient volume reduces bouyancy, which causes the brain to sink and make contact with the base of the skull. The connection between the cranial compartment and spinal compartment is in the upper cervical spine. Malformations, injuries and misalignments of the upper cervical spine can cause a dissociation of CSF flow between the cranial and spinal compartment. Further below in the lower spine, spondylosis (degeneration), scoliosis (abnormal curvature) and stenosis (narrowing) alter the design of the spinal canal and thus affect blood and CSF flow. The changes in the design of the spinal canal can, likewise, result in a dissociation of CSF flow between the cranial vault and spinal canal. Thus far, the studies on dissociation of CSF flow between the cranial vault and spinal canal have all been done using supine MRI. Future research will need to be done using upright MRI. Upright MRI will most likely reveal much more about the destructive consequences of dissociation of CSF flow between the cranial vault and spinal canal.
The areas hardest hit by faulty fluid mechanics in the cranial vault are: 1) the periventricular structures that surround the ventricles, 2) the bottom surfaces of the brain, brainstem and cerebellum located above the base of the skull that are surrounded and supported by the cisterns, and 3) the cortex of the brain closest to the inner surface of the skull. The particular areas that are affected are determined by the cause and the consequences of the faulty CSF flow.
For more information on this and other related subjects visit my website at www.upright-health.com.
Hydrofracking, Ventriculomegaly and Brain Atrophy
Researchers suspect that enlarged ventricles, known as ventriculomegaly, seen in many neurodegenerative diseases may be the result of atrophy (decrease in size) of the brain. The cause of the damage or atrophy of the brain may be due to destructive waves and hydraulic pressures that damage tissues by a process I compare to hydrofracking which is used by engineers to fracture rocks. Ventriculomegaly and brain atrophy have been associated with Alzheimer’s disease, Parkinson’s disease and its variants, called Parkinson’s Plus, as well as multiple sclerosis, amyotrophic lateral sclerosis and Huntington’s disease.
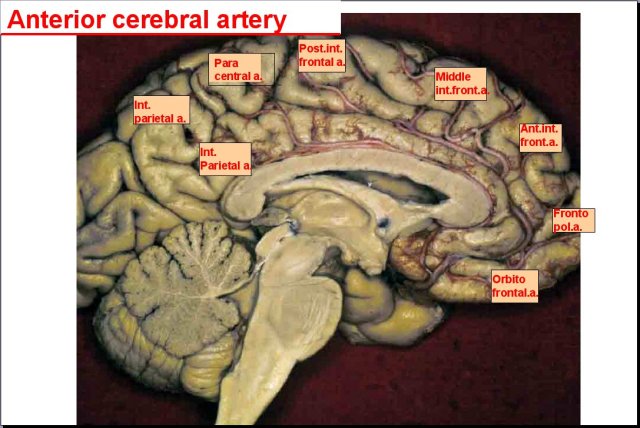
The picture above shows the left half of the brain. The face would be to the right. The cauliflower structure in the lower left corner is the cerebellum. The hollow area (darker grey) in the middle of the brain is the left lateral ventricle. The heavy white structure that forms the roof over the lateral ventricle is the corpus callosum. The heavy white structure that forms the floor is the fornix. The corpus callosum is a group of myelinated (white matter) high speed interconnecting communication pathways that link the left and right halves of the brain. The fornix is, likewise, a high-speed communication pathway of white fibers. The third ventricle is located just below the fornix. The fourth ventricle is the space shaped like a dart between the cerebellum and brainstem. The ventricles are chambers in the core of the brain and brainstem where cerebrospinal fluid (CSF) is produced.
CFS is basically water with some sugar and a few other ingredients mixed in. CSF fills the ventricles and surrounds the entire brain in a water jacket. CSF in the ventricles, fissures and spaces of the brain serves to cushion and protect the brain from compression against the bones of the cranial vault, as well as maintain its shape, layout and position inside the vault. It also serves as the lymphatic waste removal system of the brain. Due to the constant state of tension caused by CSF in the ventricles and spaces in and around the brain, some engineers consider the brain to be essentially a non-compressible monophasic structure. Monophasic simply means that it doesn’t buckle and deform under pressure.
In contrast to engineers, chiropractic and osteopathic craniosacral theories have maintained for many years that the musculoskeletal system, CSF and central nervous system, which includes the brain and spinal cord, rhythmically pulsate and move. The movement and pulsations are driven by neurological, cardiovascular and respiratory waves. More recently, radiologists have similarly shown that CSF pulsates and that the ventricles expand and contract in synchrony with cardiovascular waves. They have also shown that the brain moves up and down like a piston during each cardiac cycle. This is because the increase in volume, mass and pressure of the brain caused by the increase in blood volume drives the brain downward in the cranial vault. Relaxation of the heart relieves the pressure and strain, which causes the brain to rise inside the vault. This expansion and contraction coupled with up and down movement of the brain inside the vault makes it a biphasic structure in engineering terms and futher confirms the craniosacral theory.
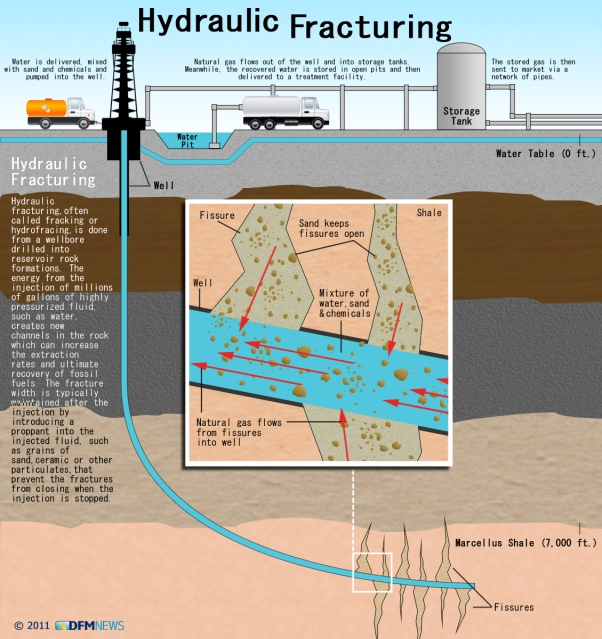
The picture below is from an article published in 2011 in the Delaware Free Media News on the politically controversial process called hydrofracking. Hydrofracking is done by pumping water under pressure into rocks located deep below the surface of the earth to open their fissures (cracks) and pores by fracturing them. The process is mostly used to flush out oils and gases to be brought to the surface and refined. In addition to the potential pollution of water aquifers that are located above the fracture zone, the compression and shear stress caused by hydrofracking can set off vibrational waves deep below in the fracture zone that travel to the surface where they can be felt as earthquakes by residents. The earthquakes can cause tears in the surface of the earth and cracks in buildings.
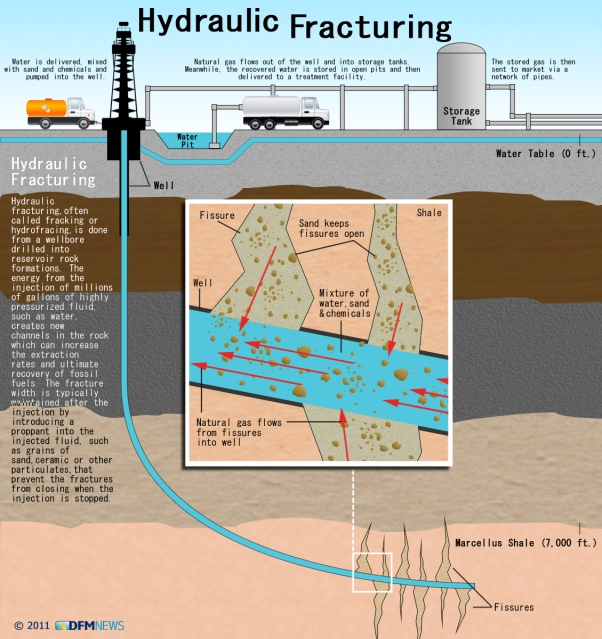
A similar situation can occur inside the cranial vault of the skull due to the heart pumping a relatively large volume of blood with each contraction, into the mostly closed container of the cranial vault. If the blood volume and pressure coming into the cranial vault isn’t sufficiently buffered (within the subarachnoid space shown below) before it enters the brain, strong pressure waves can be sent into the core of the brain. These high pressure waves can damage delicate tissues resulting in atrophy and subsequent ventriculomegaly. The structures that most often show atrophy are often located in the periventricular areas, the areas that surround the ventricles.
Aside from atrophy, some cases of ventriculomegaly are caused by an increase in CSF volume due to obstruction or faulty flow. In these cases, the ventricles and brain return to normal size when flow is restored via shunts and surgery due to their biphasic nature. While these cases are seen much less frequently thus far, early detection may change things and prevent permanent damage and subsequent atrophy.
In addition to unchecked incoming high pressure arterial waves causing problems, damage can also occur to periventricular structures due to overstretching similar to an overinflated balloon. At the same time, the expanding ventricles can compress neighboring structures and blood vessels. Compression of blood vessels can decrease blood flow in smaller blood vessels resulting in chronic ischemia and subsequent atrophy. Some researchers further suspect that faulty CSF flow may cause water hammers(explained below) in the brain similar to tremors and earthquakes caused by hydrofracking. Water hammers can similarly fracture surrounding tissues resulting in atrophy. In any case, the cause of the ventriculomegaly and atrophy can come from water pressure problems inside the ventricles or outside of them.
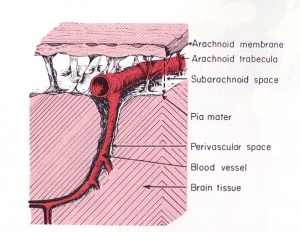 In contrast to hydrofracking which pumps large volumes of water into deep subterranean rocks, the heart pumps a relatively large volume of blood into the arteries contained within the subarachnoid space (see picture to the right). The subarachnoid space surrounds the outer surfaces of the lobes, the convolutions (gyri) and fissures of the brain and the brainstem within the cranial vault. The large incoming arteries pass through the subarachnoid space to supply numerous smaller branches (arterioles) that exit the subarachnoid space and enter tunnels called perivascular or Verchow-Robin spaces to supply smaller branches that supply the parenchyma (substance) of the brain.
In contrast to hydrofracking which pumps large volumes of water into deep subterranean rocks, the heart pumps a relatively large volume of blood into the arteries contained within the subarachnoid space (see picture to the right). The subarachnoid space surrounds the outer surfaces of the lobes, the convolutions (gyri) and fissures of the brain and the brainstem within the cranial vault. The large incoming arteries pass through the subarachnoid space to supply numerous smaller branches (arterioles) that exit the subarachnoid space and enter tunnels called perivascular or Verchow-Robin spaces to supply smaller branches that supply the parenchyma (substance) of the brain.
As stated above, the periventricular areas are those structures that interface with the ventricles. These are important nerve centers. Blood vessels also pass through the periventricular space between the ventricles and surrounding structures. As you can see in the picture of the brain at the top of the page, arteries pass over the lateral ventricles. Veins also pass over the lateral ventricles. Smaller arteries and veins are similarly located next to the third and fourth ventricle. In contrast to the veins on the surface of the brain, the periventricular veins are much smaller and more susceptible to compression. Smaller arterioles can, likewise, be compressed.
The stress from the increase in blood volume causes mechanical strains and temporary deformation of the brain as the subarachnoid space balloons slightly outward. In cases of high intracranial pressure, the areas of the subarachnoid space located near the bones of the cranial vault can compress surface veins of the brain against the bones of the vault and, thereby, decrease blood flow. Ballooning of the subarachnoid space also causes compression loads on the lobes of the brain and the ventricles similar to squeezing a sponge. Due to their location in the core of the brain, the periventricular areas are the most vulnerable to compression and shear stresses.
In addition to compression loads caused by enlargement of the subarachnoid space and ventricles, ventriculomegaly also causes shear stresses due to stretching of the periventricular structures and blood vessels. The combination of excess compression and shear stresses can, over time, cause mechanical damage to the structures and blood vessels, as well as decrease blood flow that can result in tissue atrophy (shrinkage).
The rhythmical beating of the heart thus causes pulsations and pressure waves to form in the brain, blood and CSF. Those pulsating hydraulic waves dissipate through the entire brain. If the pressure isn’t reduced appropriately, the high pressure arterial waves on the surface of the brain get directed inward toward the weaker more vulnerable parts of the brain, such as those surrounding the ventricles in the periventricular areas. These structures get compressed against the unyielding walls of the cranial vault on the outside and the stiff walls of the ventricles in the center of the brain that are supported by internal tension from CSF pressure. Chronic pulsatile high pressure waves can lead to hydraulic fracturing of vulnerable tissues. This can result in degeneration and atrophy of surrounding periventricular structures. Some researchers suspect that myelinated nerves (white matter) such as those that surround the ventricles, are more vulnerable to tension strains and subsequently more likely to tear (fracture) from excess loads.
In a healthy brain, the subarachnoid space typically buffers the increase in blood volume and pressure. Most of the force is absorbed by veins in the subarachnoid space which have weak walls and are easily compressible. Compression of the veins moves blood out of the brain reducing pressureby removing volume inside the cranial vault. Pressure is further relieved by squeezing a proportionate amount of venous blood and CSF out of the brain and cranial vault by way of the foramen magnum, which is the large hole in the base of the skull for the passage of the brainstem and cord. As the arterioles relax following contraction of the heart, and the arteries and veins begin to return to their previous size, the fresh supply of arterial blood in the subarachnoid space is released into the perivascular spaces of the brain under lower pressure.
 Blockage of venous blood and cerebrospinal fluid anywhere along their pathways can alter CSF flow and cause abnormal pressure waves. The abnormal pressure waves are the result of incoming arterial blood flow and pressure waves running into resistance from venous backpressure and reduced or blocked CSF outflow causing what plumbers refer to as a water hammer. As shown in the sketch on the left, water hammers occur in domestic plumbing when water flow out of a faucet is suddenly shut off. This causes waves to be reflected backwards and crash with incoming waves. Since stiff non-elastic pipes can’t absorb the force like elastic veins, it causes them to shudder like a tremor. The tremor causes the pipes to bounce on surrounding structures resulting in noises that sound like someone hammering on the pipes.
Blockage of venous blood and cerebrospinal fluid anywhere along their pathways can alter CSF flow and cause abnormal pressure waves. The abnormal pressure waves are the result of incoming arterial blood flow and pressure waves running into resistance from venous backpressure and reduced or blocked CSF outflow causing what plumbers refer to as a water hammer. As shown in the sketch on the left, water hammers occur in domestic plumbing when water flow out of a faucet is suddenly shut off. This causes waves to be reflected backwards and crash with incoming waves. Since stiff non-elastic pipes can’t absorb the force like elastic veins, it causes them to shudder like a tremor. The tremor causes the pipes to bounce on surrounding structures resulting in noises that sound like someone hammering on the pipes.
Alzheimer’s and other neurodegenerative diseases seen in adults are often associated with normal pressure hydrocephalus (NPH) in which the ventricles enlarge but CSF pressure remains normal or just slightly elevated. To this day, it remains a mystery to scientists as to how the ventricles can enlarge when CSF pressure is normal. The only plausible explanation so far is atrophy. In other words, the brain decreases in size around the ventricles creating space allowing the ventricles to enlarge when CSF moves into the ventricles.
Some researchers suspect that brain atrophy is caused by water hammers that damage susceptible tissues. Others suggest that it is due to compression and shear stresses mentioned previously. Still others suggest that compression and shear forces can damage blood vessels and decrease flow resulting in atrophy. Lastly, some cases are due to an increase in CSF volume due to faulty flow without atrophy. In other words, the brain is simply compressed and returns to normal size when CSF flow and volume are restored as mentioned above.
In brief, the biphasic brain is trapped between a rock and a hard place. The rock is the skull that surrounds and protects it. The hard places are the ventricles located in its core, as well as the surrounding spaces, filled with CSF. Shear stresses caused by stretching from ventriculomegaly strain the periventricular tissues. Increases in arterial blood volume during heart contractions cause compression load strains that deform the brain and ventricles. Abnormally high blood and CSF pressure waves coupled with water hammers compound the internal and external ventricular stresses and strains with tremors. Over time, strong chronic tremors can tear tissues.
Researchers are now looking into the impact of blockage of the venous drainage system of the brain and abnormal CSF pulse waves. Over time, chronic venous drainage problems and high CSF pressure waves can lead to hydrofracking, ventriculomegaly and atrophy of the brain. One of the most likely points of blockage to venous blood and CSF flow is in the cervical spine, especially the upper cervical spine. The most vulnerable structures to hydrofracking and subsequent atrophy are located in the periventricular areas that interface with the lobes of the brain.
For additional information on these and related topics visit my website at www.upright-health.com.
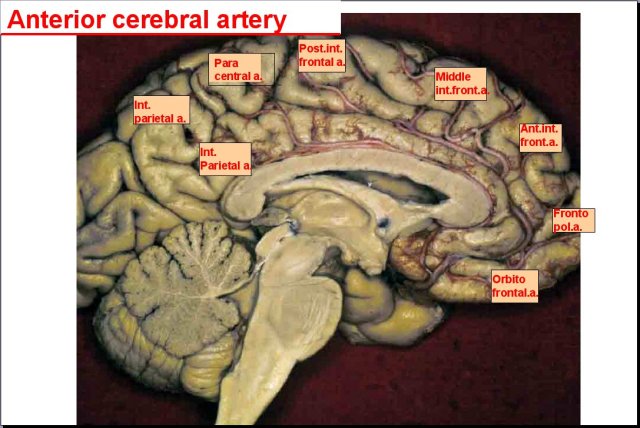
The picture above shows the left half of the brain. The face would be to the right. The cauliflower structure in the lower left corner is the cerebellum. The hollow area (darker grey) in the middle of the brain is the left lateral ventricle. The heavy white structure that forms the roof over the lateral ventricle is the corpus callosum. The heavy white structure that forms the floor is the fornix. The corpus callosum is a group of myelinated (white matter) high speed interconnecting communication pathways that link the left and right halves of the brain. The fornix is, likewise, a high-speed communication pathway of white fibers. The third ventricle is located just below the fornix. The fourth ventricle is the space shaped like a dart between the cerebellum and brainstem. The ventricles are chambers in the core of the brain and brainstem where cerebrospinal fluid (CSF) is produced.
CFS is basically water with some sugar and a few other ingredients mixed in. CSF fills the ventricles and surrounds the entire brain in a water jacket. CSF in the ventricles, fissures and spaces of the brain serves to cushion and protect the brain from compression against the bones of the cranial vault, as well as maintain its shape, layout and position inside the vault. It also serves as the lymphatic waste removal system of the brain. Due to the constant state of tension caused by CSF in the ventricles and spaces in and around the brain, some engineers consider the brain to be essentially a non-compressible monophasic structure. Monophasic simply means that it doesn’t buckle and deform under pressure.
In contrast to engineers, chiropractic and osteopathic craniosacral theories have maintained for many years that the musculoskeletal system, CSF and central nervous system, which includes the brain and spinal cord, rhythmically pulsate and move. The movement and pulsations are driven by neurological, cardiovascular and respiratory waves. More recently, radiologists have similarly shown that CSF pulsates and that the ventricles expand and contract in synchrony with cardiovascular waves. They have also shown that the brain moves up and down like a piston during each cardiac cycle. This is because the increase in volume, mass and pressure of the brain caused by the increase in blood volume drives the brain downward in the cranial vault. Relaxation of the heart relieves the pressure and strain, which causes the brain to rise inside the vault. This expansion and contraction coupled with up and down movement of the brain inside the vault makes it a biphasic structure in engineering terms and futher confirms the craniosacral theory.
The picture below is from an article published in 2011 in the Delaware Free Media News on the politically controversial process called hydrofracking. Hydrofracking is done by pumping water under pressure into rocks located deep below the surface of the earth to open their fissures (cracks) and pores by fracturing them. The process is mostly used to flush out oils and gases to be brought to the surface and refined. In addition to the potential pollution of water aquifers that are located above the fracture zone, the compression and shear stress caused by hydrofracking can set off vibrational waves deep below in the fracture zone that travel to the surface where they can be felt as earthquakes by residents. The earthquakes can cause tears in the surface of the earth and cracks in buildings.
A similar situation can occur inside the cranial vault of the skull due to the heart pumping a relatively large volume of blood with each contraction, into the mostly closed container of the cranial vault. If the blood volume and pressure coming into the cranial vault isn’t sufficiently buffered (within the subarachnoid space shown below) before it enters the brain, strong pressure waves can be sent into the core of the brain. These high pressure waves can damage delicate tissues resulting in atrophy and subsequent ventriculomegaly. The structures that most often show atrophy are often located in the periventricular areas, the areas that surround the ventricles.
Aside from atrophy, some cases of ventriculomegaly are caused by an increase in CSF volume due to obstruction or faulty flow. In these cases, the ventricles and brain return to normal size when flow is restored via shunts and surgery due to their biphasic nature. While these cases are seen much less frequently thus far, early detection may change things and prevent permanent damage and subsequent atrophy.
In addition to unchecked incoming high pressure arterial waves causing problems, damage can also occur to periventricular structures due to overstretching similar to an overinflated balloon. At the same time, the expanding ventricles can compress neighboring structures and blood vessels. Compression of blood vessels can decrease blood flow in smaller blood vessels resulting in chronic ischemia and subsequent atrophy. Some researchers further suspect that faulty CSF flow may cause water hammers(explained below) in the brain similar to tremors and earthquakes caused by hydrofracking. Water hammers can similarly fracture surrounding tissues resulting in atrophy. In any case, the cause of the ventriculomegaly and atrophy can come from water pressure problems inside the ventricles or outside of them.
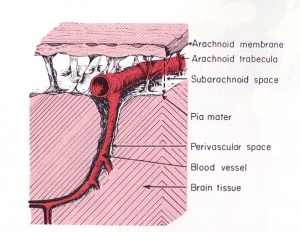 In contrast to hydrofracking which pumps large volumes of water into deep subterranean rocks, the heart pumps a relatively large volume of blood into the arteries contained within the subarachnoid space (see picture to the right). The subarachnoid space surrounds the outer surfaces of the lobes, the convolutions (gyri) and fissures of the brain and the brainstem within the cranial vault. The large incoming arteries pass through the subarachnoid space to supply numerous smaller branches (arterioles) that exit the subarachnoid space and enter tunnels called perivascular or Verchow-Robin spaces to supply smaller branches that supply the parenchyma (substance) of the brain.
In contrast to hydrofracking which pumps large volumes of water into deep subterranean rocks, the heart pumps a relatively large volume of blood into the arteries contained within the subarachnoid space (see picture to the right). The subarachnoid space surrounds the outer surfaces of the lobes, the convolutions (gyri) and fissures of the brain and the brainstem within the cranial vault. The large incoming arteries pass through the subarachnoid space to supply numerous smaller branches (arterioles) that exit the subarachnoid space and enter tunnels called perivascular or Verchow-Robin spaces to supply smaller branches that supply the parenchyma (substance) of the brain.As stated above, the periventricular areas are those structures that interface with the ventricles. These are important nerve centers. Blood vessels also pass through the periventricular space between the ventricles and surrounding structures. As you can see in the picture of the brain at the top of the page, arteries pass over the lateral ventricles. Veins also pass over the lateral ventricles. Smaller arteries and veins are similarly located next to the third and fourth ventricle. In contrast to the veins on the surface of the brain, the periventricular veins are much smaller and more susceptible to compression. Smaller arterioles can, likewise, be compressed.
The stress from the increase in blood volume causes mechanical strains and temporary deformation of the brain as the subarachnoid space balloons slightly outward. In cases of high intracranial pressure, the areas of the subarachnoid space located near the bones of the cranial vault can compress surface veins of the brain against the bones of the vault and, thereby, decrease blood flow. Ballooning of the subarachnoid space also causes compression loads on the lobes of the brain and the ventricles similar to squeezing a sponge. Due to their location in the core of the brain, the periventricular areas are the most vulnerable to compression and shear stresses.
In addition to compression loads caused by enlargement of the subarachnoid space and ventricles, ventriculomegaly also causes shear stresses due to stretching of the periventricular structures and blood vessels. The combination of excess compression and shear stresses can, over time, cause mechanical damage to the structures and blood vessels, as well as decrease blood flow that can result in tissue atrophy (shrinkage).
The rhythmical beating of the heart thus causes pulsations and pressure waves to form in the brain, blood and CSF. Those pulsating hydraulic waves dissipate through the entire brain. If the pressure isn’t reduced appropriately, the high pressure arterial waves on the surface of the brain get directed inward toward the weaker more vulnerable parts of the brain, such as those surrounding the ventricles in the periventricular areas. These structures get compressed against the unyielding walls of the cranial vault on the outside and the stiff walls of the ventricles in the center of the brain that are supported by internal tension from CSF pressure. Chronic pulsatile high pressure waves can lead to hydraulic fracturing of vulnerable tissues. This can result in degeneration and atrophy of surrounding periventricular structures. Some researchers suspect that myelinated nerves (white matter) such as those that surround the ventricles, are more vulnerable to tension strains and subsequently more likely to tear (fracture) from excess loads.
In a healthy brain, the subarachnoid space typically buffers the increase in blood volume and pressure. Most of the force is absorbed by veins in the subarachnoid space which have weak walls and are easily compressible. Compression of the veins moves blood out of the brain reducing pressureby removing volume inside the cranial vault. Pressure is further relieved by squeezing a proportionate amount of venous blood and CSF out of the brain and cranial vault by way of the foramen magnum, which is the large hole in the base of the skull for the passage of the brainstem and cord. As the arterioles relax following contraction of the heart, and the arteries and veins begin to return to their previous size, the fresh supply of arterial blood in the subarachnoid space is released into the perivascular spaces of the brain under lower pressure.
 Blockage of venous blood and cerebrospinal fluid anywhere along their pathways can alter CSF flow and cause abnormal pressure waves. The abnormal pressure waves are the result of incoming arterial blood flow and pressure waves running into resistance from venous backpressure and reduced or blocked CSF outflow causing what plumbers refer to as a water hammer. As shown in the sketch on the left, water hammers occur in domestic plumbing when water flow out of a faucet is suddenly shut off. This causes waves to be reflected backwards and crash with incoming waves. Since stiff non-elastic pipes can’t absorb the force like elastic veins, it causes them to shudder like a tremor. The tremor causes the pipes to bounce on surrounding structures resulting in noises that sound like someone hammering on the pipes.
Blockage of venous blood and cerebrospinal fluid anywhere along their pathways can alter CSF flow and cause abnormal pressure waves. The abnormal pressure waves are the result of incoming arterial blood flow and pressure waves running into resistance from venous backpressure and reduced or blocked CSF outflow causing what plumbers refer to as a water hammer. As shown in the sketch on the left, water hammers occur in domestic plumbing when water flow out of a faucet is suddenly shut off. This causes waves to be reflected backwards and crash with incoming waves. Since stiff non-elastic pipes can’t absorb the force like elastic veins, it causes them to shudder like a tremor. The tremor causes the pipes to bounce on surrounding structures resulting in noises that sound like someone hammering on the pipes.Alzheimer’s and other neurodegenerative diseases seen in adults are often associated with normal pressure hydrocephalus (NPH) in which the ventricles enlarge but CSF pressure remains normal or just slightly elevated. To this day, it remains a mystery to scientists as to how the ventricles can enlarge when CSF pressure is normal. The only plausible explanation so far is atrophy. In other words, the brain decreases in size around the ventricles creating space allowing the ventricles to enlarge when CSF moves into the ventricles.
Some researchers suspect that brain atrophy is caused by water hammers that damage susceptible tissues. Others suggest that it is due to compression and shear stresses mentioned previously. Still others suggest that compression and shear forces can damage blood vessels and decrease flow resulting in atrophy. Lastly, some cases are due to an increase in CSF volume due to faulty flow without atrophy. In other words, the brain is simply compressed and returns to normal size when CSF flow and volume are restored as mentioned above.
In brief, the biphasic brain is trapped between a rock and a hard place. The rock is the skull that surrounds and protects it. The hard places are the ventricles located in its core, as well as the surrounding spaces, filled with CSF. Shear stresses caused by stretching from ventriculomegaly strain the periventricular tissues. Increases in arterial blood volume during heart contractions cause compression load strains that deform the brain and ventricles. Abnormally high blood and CSF pressure waves coupled with water hammers compound the internal and external ventricular stresses and strains with tremors. Over time, strong chronic tremors can tear tissues.
Researchers are now looking into the impact of blockage of the venous drainage system of the brain and abnormal CSF pulse waves. Over time, chronic venous drainage problems and high CSF pressure waves can lead to hydrofracking, ventriculomegaly and atrophy of the brain. One of the most likely points of blockage to venous blood and CSF flow is in the cervical spine, especially the upper cervical spine. The most vulnerable structures to hydrofracking and subsequent atrophy are located in the periventricular areas that interface with the lobes of the brain.
For additional information on these and related topics visit my website at www.upright-health.com.
Ventriculomegaly and Mega Cisterns in Alzheimer’s, Parkinsons and MS
About seventy years ago, a highly regarded neurosurgeon from Columbia, Dr. Solomon Hakim, noticed that on autopsy many patients with Alzheimer’s disease had enlargement of the ventricles without destruction of the outer cortex of the brain, which would have happened if the enlargement was due to high pressure. The ventricles are chambers in the center of the brain and brainstem where a watery substance called cerebrospinal fluid (CSF) is produced. The purpose of CSF is to support and protect the brain. It also removes waste from the brain. Enlargement of the ventricles is called ventriculomegaly. Ventriculomegaly seen on brain scans is a sign of hydrocephalus, which is an increase in CSF volume in the brain.
Ventriculomegaly stretches and deforms the surrounding periventricular structures. Prolonged deformation can lead to plastic deformation, which is permanent. Ventriculomegaly also compresses the veins, that are located on the outer surface of the brain, against the bones of the cranial vault. This can decrease venous drainage of the brain and cause the hydrocephalic condition to worsen. Ventriculomegaly and damage to periventricular structures may play a role in many of the signs and symptoms associated with neurodegenerative diseases such as motor weaknesses, dementia, cog fog, heat intolerance, sleep disturbances, sleep apnea and incontinence of the bowel and bladder.
 Dr. Hakim later called the condition he discovered normal pressure hydrocephalus (NPH). He also made a major improvement in the design of the spring on the valves that are used in shunts to treat hydrocephalus. The principle behind his modification to shunts is still in use today.
Dr. Hakim later called the condition he discovered normal pressure hydrocephalus (NPH). He also made a major improvement in the design of the spring on the valves that are used in shunts to treat hydrocephalus. The principle behind his modification to shunts is still in use today.
In 1976 Dr. Hakim published a paper in which he compared the brain to a sponge and suggested that poroelasticity plays a role in the development of ventriculomegaly. The term poroelasticity comes from engineering sciences related to soils and rocks and will be explained later in this post. Since the advent of brain scans, ventriculomegaly has been associated with Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, and other neurodegenerative conditions. Mega cisterns are enlarged CSF chambers similar to ventriculomegaly and will also be discussed in this post.
In the brain scan below, the lateral ventricles are located beneath the large white arch-like structure. A smaller arch-like white band underneath the larger structure is joined to it in the rear and is the bottom of the lateral ventricle. The third ventricle is below the lower white band and above the midbrain which is the uppermost part of the brainstem (stalk-like). The fourth ventricle is the dart shaped area between the brainstem in front and a cauliflower-like looking structure in the rear, which is the cerebellum.
 The dark gray spaces in front of the brainstem and beneath the cerebellum are called cisterns. CSF flows out of the fourth ventricle and into the cisterns. The cisterns cushion the brain from the hard walls of the cranial vault. They also support the brain and prevent it from sinking into the large hole in the bottom of the vault called the foramen magnum. This is the opening for the passage of the brainstem and spinal cord, as well as blood vessels and CSF pathways.
The dark gray spaces in front of the brainstem and beneath the cerebellum are called cisterns. CSF flows out of the fourth ventricle and into the cisterns. The cisterns cushion the brain from the hard walls of the cranial vault. They also support the brain and prevent it from sinking into the large hole in the bottom of the vault called the foramen magnum. This is the opening for the passage of the brainstem and spinal cord, as well as blood vessels and CSF pathways.
Ventriculomegaly can be caused by an increase in CSF volume and pressure in the ventricles, or it can be caused by atrophy (shrinking) of the brain due to degeneration of the structures that surround them. It can also be a combination of atrophy and changes in CSF volume and pressure. In many cases the cause of the ventriculomegaly is unknown. In any case, enlargement of the ventricles can affect the important structures that surround them in what is called the periventricular areas.
The periventricular structures that surround the ventricles are some of the most important and fundamental systems in the brain such as the limbic (reptilian/visceral/self-preservation) and autonomic (vegetative) nervous systems. The roof of the lateral ventricles is formed by a large group of myelinated (white matter) nerves that link the left and right hemispheres of the brain. Descending long myelinated motor (muscle) nerve tracts called the internal capsule pass close to the ventricles.
To get a better understanding of the mechanical forces that can cause enlargement of the ventricles, researchers have been turning to engineers, mathematicians and physicists for answers. From an engineering perspective, the skull and brain, as well as the fluids inside them can be compared to rocks and soils. Poroelasticity is a property of rocks and soils that affect their structural strength and their abiltiy to support large loads such as from water, waves, buildings, bridges and roads. Different types of rocks and soils, as well as the shapes of their pores, fissures, fractures and caves affect the way they handle loads. Similarly, poroelasticity affects the structural strength and shape of the brain, as well as deformation such as ventriculomegaly. This is important because deformation of the brain such as enlarged ventricles can damage nearby delicate nerves and blood vessels. Damage to nerves and blood vessels can, in turn, lead to atrophy (shrinkage) and ventriculomegaly.
 The term poroelasticity refers to the pores in soils and rocks that affect their elasticity. Elasticity is the ability of a structure to deform and return to its original shape without breaking (fracturing). The pores in soils and rocks can be filled with gas or fluids. The gas could be air or natural gas. The fluid could be water or oil. The gases or fluids affect the strength of soils and rocks, as well as their elasticity. Consequently, the gases and fluids affect the ability of soils and rocks to deform and reform. Structures that go through expansion and contraction are considered to be biphasic. If it can’t deform and reform, meaning return to its original shape, the structure is considered to be monophasic. The ability of a structure to deform and return to its original shape is determined by, what is called, its elastic coefficient.
The term poroelasticity refers to the pores in soils and rocks that affect their elasticity. Elasticity is the ability of a structure to deform and return to its original shape without breaking (fracturing). The pores in soils and rocks can be filled with gas or fluids. The gas could be air or natural gas. The fluid could be water or oil. The gases or fluids affect the strength of soils and rocks, as well as their elasticity. Consequently, the gases and fluids affect the ability of soils and rocks to deform and reform. Structures that go through expansion and contraction are considered to be biphasic. If it can’t deform and reform, meaning return to its original shape, the structure is considered to be monophasic. The ability of a structure to deform and return to its original shape is determined by, what is called, its elastic coefficient.
As far as biphasic poroelastic properties are concerned, blood and CSF are essentially non-porous and non-compressible. They also lack elastic properties. Instead, they have viscoelastic properties that are entirely different. Basically, elasticity is a property of solid structures. Viscoelasticity refers to properties of liquids and foams such as viscoelastic memory foam mattresses used for sleep surfaces. In contrast to blood and CSF, the brain is made of billions of cells that are filled with fluids called intracellular fluids. The brain’s many fissures, sulci, interstitial spaces, perivascular spaces, subarachnoid spaces, ventricles, caverns, cisterns and sinuses are all filled with fluids such as, intracellular fluids, interstitial fluids, blood and CSF. This makes the brain a highly porous liquid filled structure.
In addition to being porous, the brain is also elastic. For example, tumors and hydrocephalus can cause significant deformation of the brain. When the stress is removed, however, it returns to normal size provided permanent damage has not yet occurred. Being elastic technically makes the brain a biphasic structure capable of expansion and contraction. Under normal circumstances, however, the brain is only slightly biphasic. This is because it is completely surrounded and all it spaces are filled with CSF. CSF pressure causes internal and external tension, called turgor, in the pores and spaces of the brain. Turgor causes stiffness.
The stiffness caused by turgor is important to maintaining the shapes of living things. Plants use turgor to stay upright. If they become dehydrated they quickly start to droop. Cells similarly use turgor to maintain their structure and internal space and prevent compression. Turgor, likewise, maintains the shape of the brain. Maintaining the shape of the brain is important because it prevents compression of delicate nerve structures and smaller blood vessels that travel through sulci (folds), fissures (cracks) and foramen (holes) in the brain and skull. Turgor also keeps the ventricles from collapsing which is called slit ventricles. Slit ventricles occur due to overdrainge of CSF by external surgical shunts. They can also occur when the normal CSF pressure gradient is reversed. I will discuss shunts, siphons and slit ventricles further in future posts. In addition to maintaining the size of the ventricles turgor helps to keep the brain afloat and prevent it from sinking or making contact with the cranial vault.
Turgor has its limitations, however. Too much turgor limits the compliance of the brain. Compliance is a term used to describe the stretch phase of elasticity in the brain. Compliance allows tissue to deform without damage such as with compression and stretching. Elastance is the complete opposite of compliance. Elastance is the strength of tissues to resist deformation and return to their original shape once the load is removed. Elastance preserves the designs and shapes of structures. On the other hand, the compliance of certain tissues in the brain, especially weak-walled veins, allows them to buffer the impact of the relatively large volume of blood and the associated increase in pressure that is pumped into the cranial vault with each contraction phase of the heart roughly seventy times per minute. The strength of the arterial waves of blood and the pressure pumped in during each heart beat needs to be decreased and modified before sending it into the delicate internal structures of the brain.
The dark grey areas on the bran scan above is CSF. As you can see, CSF fills all the spaces, cracks and caves. The brain is also contained inside the cranial vault and surrounded by CSF that maintains its position and prevents contact with the bones of the vault. Although it is highly porous, the interior and exterior surfaces of the skull are more like limestone or granite in that it has poor permeability. The non-permeable hard shell of the skull protects the brain and keeps the weather out. Although it lacks permeability, the skull is penetrated by many holes called foramen and other openings, which makes it highly porous. Nerves, blood and CSF travel through these openings. Moreover, pressure in these openings can have a profound effect on fluid mechanics in the brain.
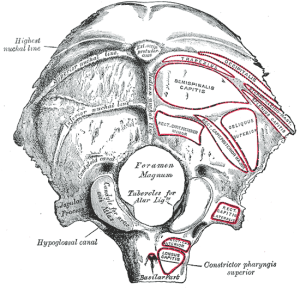 While it is not considered to be a factor that directly affects compliance (elasticity) in the brain, the foramen magnum and spinal canal play an important role in maintaining CSF volume and pressure in the brain. As shown in the picture on the left of the skull base, the foramen magum is the large hole in the base of the skull that connects the cranial vault to the spinal canal. The arterial pulsations and pressure waves that are pumped into the brain by the heart are not only buffered but a proportionate outflow in the amount of blood and CSF is also transferred out of the cranial vault and brain through the foramen magnum and into the spinal canal.
While it is not considered to be a factor that directly affects compliance (elasticity) in the brain, the foramen magnum and spinal canal play an important role in maintaining CSF volume and pressure in the brain. As shown in the picture on the left of the skull base, the foramen magum is the large hole in the base of the skull that connects the cranial vault to the spinal canal. The arterial pulsations and pressure waves that are pumped into the brain by the heart are not only buffered but a proportionate outflow in the amount of blood and CSF is also transferred out of the cranial vault and brain through the foramen magnum and into the spinal canal.
Obstruction of venous and CSF pathways in the foramen magnum can affect intracranial pulsatility and pressure waves. In particular it can cause back pressure on the drainage system that results in increased turgor resulting in stiffness due to loss of compliance (elasticity). Obstruction to blood and CSF flow through the foramen magnum can also cause CSF inversion (reverse) flows, turblulence and water hammers in the brain. CSF inversion flows, turbulence and water hammers may play a destructive role that results in damage to periventricular structures.
The most common place for obstruction of CSF outflow to occur is in the craniocervical junction (upper cervical spine). The most common causes of obstruction in the craniocervical junction are malformations and mechanical strains such as misalignments. Obstructions due to malformations and mechanical strains indirectly but significantly affect intracranial compliance (elasticity) and the ability of the brain to absorb and control fluid mechanics caused by heart contractions.
To get a better understanding of how faulty fluid mechanics batter the brain, researchers and engineers are now plugging biphasic poroelastic properties of the brain into computational fluid dynamics and finite element analysis formulas to form computer models to predict and determine the cause of ventriculomegaly. They are also using physics formulas for computational fluid dynamics to determine flow through the different structures of the brain such as the ventricles. The different structures of the brain and the skull have complex shapes and different materials with different degrees of strength and compliance (elasticity), as well as their differing response to hydraulic pressure.
Hydraulic force is a product of pressure multiplied by the size of the area the pressure is being applied to, such as the volume of the ventricles or cisterns for example. A hydraulic pump can be used to increase force by applying pressure to a larger cylinder. Similarly, the pressure from the heart exerts more force on the larger pores and spaces of the brain compared to smaller ones. In this regard, the largest spaces in the brain are the ventricles and cisterns. The effects of hydraulic force may play a role in the ventriculomegaly seen in neurodegenerative condtions such as Alzheimer’s, Parkinson’s and multiple sclerosis. Constant strain from increased force in the ventricles and cisterns may cause a breakdown in the elastic properties of the brain so that the ventricles and surrounding structures can no longer return to their original shape, which is called plastic (permanent) deformation. Dr. Hakim also suggested, many years ago, that the greater size of the ventricles allow them to exert more force and thus maintain the ventriculomegaly with relatively lower pressure (turgor).
In addition to Hakim’s theory regarding ventriculomegaly, my theory regarding mega cisterns, which are enlarged cisterns, is that they are caused by inversion flows, turbulance and hydraulic forces that damage the brainstem and cerebellum resulting in atrophy of nearby structures. Mega Cisterns and atrophy of the brainstem are seen in mega cisterna magna, the Dandy-Walker Complex-Continuum, and a variant form of Parkinson’s disease called olivopontocerebellar atrophy, also known and Shy-Drager Syndrome or Multisystem Atrophy. Understanding these conditions will shed further light on the role of faulty fluid mechanics and hydraulics in neurodegenerative conditions of the brain. I have covered these conditions previously and will cover them more in future posts.
Hydrofracking is a term method engineer’s use to fracture rocks with water pressure. A similar situation called a water hammer can occur in the brain and damage delicate tissues. The location of the periventricular tissues predisposes them to compression, shear forces and water hammers that can cause damage. Loss of compliance in the brain magnifies the destructive forces. My next post will be on hydrofracking and brain atrophy (shrinkage).
For further information on enlargement of the ventricles and autonomic dysfunction called dysautonomia visit my website www.upright-health.com.
Ventriculomegaly stretches and deforms the surrounding periventricular structures. Prolonged deformation can lead to plastic deformation, which is permanent. Ventriculomegaly also compresses the veins, that are located on the outer surface of the brain, against the bones of the cranial vault. This can decrease venous drainage of the brain and cause the hydrocephalic condition to worsen. Ventriculomegaly and damage to periventricular structures may play a role in many of the signs and symptoms associated with neurodegenerative diseases such as motor weaknesses, dementia, cog fog, heat intolerance, sleep disturbances, sleep apnea and incontinence of the bowel and bladder.
 Dr. Hakim later called the condition he discovered normal pressure hydrocephalus (NPH). He also made a major improvement in the design of the spring on the valves that are used in shunts to treat hydrocephalus. The principle behind his modification to shunts is still in use today.
Dr. Hakim later called the condition he discovered normal pressure hydrocephalus (NPH). He also made a major improvement in the design of the spring on the valves that are used in shunts to treat hydrocephalus. The principle behind his modification to shunts is still in use today.In 1976 Dr. Hakim published a paper in which he compared the brain to a sponge and suggested that poroelasticity plays a role in the development of ventriculomegaly. The term poroelasticity comes from engineering sciences related to soils and rocks and will be explained later in this post. Since the advent of brain scans, ventriculomegaly has been associated with Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, and other neurodegenerative conditions. Mega cisterns are enlarged CSF chambers similar to ventriculomegaly and will also be discussed in this post.
In the brain scan below, the lateral ventricles are located beneath the large white arch-like structure. A smaller arch-like white band underneath the larger structure is joined to it in the rear and is the bottom of the lateral ventricle. The third ventricle is below the lower white band and above the midbrain which is the uppermost part of the brainstem (stalk-like). The fourth ventricle is the dart shaped area between the brainstem in front and a cauliflower-like looking structure in the rear, which is the cerebellum.
 The dark gray spaces in front of the brainstem and beneath the cerebellum are called cisterns. CSF flows out of the fourth ventricle and into the cisterns. The cisterns cushion the brain from the hard walls of the cranial vault. They also support the brain and prevent it from sinking into the large hole in the bottom of the vault called the foramen magnum. This is the opening for the passage of the brainstem and spinal cord, as well as blood vessels and CSF pathways.
The dark gray spaces in front of the brainstem and beneath the cerebellum are called cisterns. CSF flows out of the fourth ventricle and into the cisterns. The cisterns cushion the brain from the hard walls of the cranial vault. They also support the brain and prevent it from sinking into the large hole in the bottom of the vault called the foramen magnum. This is the opening for the passage of the brainstem and spinal cord, as well as blood vessels and CSF pathways.Ventriculomegaly can be caused by an increase in CSF volume and pressure in the ventricles, or it can be caused by atrophy (shrinking) of the brain due to degeneration of the structures that surround them. It can also be a combination of atrophy and changes in CSF volume and pressure. In many cases the cause of the ventriculomegaly is unknown. In any case, enlargement of the ventricles can affect the important structures that surround them in what is called the periventricular areas.
The periventricular structures that surround the ventricles are some of the most important and fundamental systems in the brain such as the limbic (reptilian/visceral/self-preservation) and autonomic (vegetative) nervous systems. The roof of the lateral ventricles is formed by a large group of myelinated (white matter) nerves that link the left and right hemispheres of the brain. Descending long myelinated motor (muscle) nerve tracts called the internal capsule pass close to the ventricles.
To get a better understanding of the mechanical forces that can cause enlargement of the ventricles, researchers have been turning to engineers, mathematicians and physicists for answers. From an engineering perspective, the skull and brain, as well as the fluids inside them can be compared to rocks and soils. Poroelasticity is a property of rocks and soils that affect their structural strength and their abiltiy to support large loads such as from water, waves, buildings, bridges and roads. Different types of rocks and soils, as well as the shapes of their pores, fissures, fractures and caves affect the way they handle loads. Similarly, poroelasticity affects the structural strength and shape of the brain, as well as deformation such as ventriculomegaly. This is important because deformation of the brain such as enlarged ventricles can damage nearby delicate nerves and blood vessels. Damage to nerves and blood vessels can, in turn, lead to atrophy (shrinkage) and ventriculomegaly.
 The term poroelasticity refers to the pores in soils and rocks that affect their elasticity. Elasticity is the ability of a structure to deform and return to its original shape without breaking (fracturing). The pores in soils and rocks can be filled with gas or fluids. The gas could be air or natural gas. The fluid could be water or oil. The gases or fluids affect the strength of soils and rocks, as well as their elasticity. Consequently, the gases and fluids affect the ability of soils and rocks to deform and reform. Structures that go through expansion and contraction are considered to be biphasic. If it can’t deform and reform, meaning return to its original shape, the structure is considered to be monophasic. The ability of a structure to deform and return to its original shape is determined by, what is called, its elastic coefficient.
The term poroelasticity refers to the pores in soils and rocks that affect their elasticity. Elasticity is the ability of a structure to deform and return to its original shape without breaking (fracturing). The pores in soils and rocks can be filled with gas or fluids. The gas could be air or natural gas. The fluid could be water or oil. The gases or fluids affect the strength of soils and rocks, as well as their elasticity. Consequently, the gases and fluids affect the ability of soils and rocks to deform and reform. Structures that go through expansion and contraction are considered to be biphasic. If it can’t deform and reform, meaning return to its original shape, the structure is considered to be monophasic. The ability of a structure to deform and return to its original shape is determined by, what is called, its elastic coefficient.As far as biphasic poroelastic properties are concerned, blood and CSF are essentially non-porous and non-compressible. They also lack elastic properties. Instead, they have viscoelastic properties that are entirely different. Basically, elasticity is a property of solid structures. Viscoelasticity refers to properties of liquids and foams such as viscoelastic memory foam mattresses used for sleep surfaces. In contrast to blood and CSF, the brain is made of billions of cells that are filled with fluids called intracellular fluids. The brain’s many fissures, sulci, interstitial spaces, perivascular spaces, subarachnoid spaces, ventricles, caverns, cisterns and sinuses are all filled with fluids such as, intracellular fluids, interstitial fluids, blood and CSF. This makes the brain a highly porous liquid filled structure.
In addition to being porous, the brain is also elastic. For example, tumors and hydrocephalus can cause significant deformation of the brain. When the stress is removed, however, it returns to normal size provided permanent damage has not yet occurred. Being elastic technically makes the brain a biphasic structure capable of expansion and contraction. Under normal circumstances, however, the brain is only slightly biphasic. This is because it is completely surrounded and all it spaces are filled with CSF. CSF pressure causes internal and external tension, called turgor, in the pores and spaces of the brain. Turgor causes stiffness.
The stiffness caused by turgor is important to maintaining the shapes of living things. Plants use turgor to stay upright. If they become dehydrated they quickly start to droop. Cells similarly use turgor to maintain their structure and internal space and prevent compression. Turgor, likewise, maintains the shape of the brain. Maintaining the shape of the brain is important because it prevents compression of delicate nerve structures and smaller blood vessels that travel through sulci (folds), fissures (cracks) and foramen (holes) in the brain and skull. Turgor also keeps the ventricles from collapsing which is called slit ventricles. Slit ventricles occur due to overdrainge of CSF by external surgical shunts. They can also occur when the normal CSF pressure gradient is reversed. I will discuss shunts, siphons and slit ventricles further in future posts. In addition to maintaining the size of the ventricles turgor helps to keep the brain afloat and prevent it from sinking or making contact with the cranial vault.
Turgor has its limitations, however. Too much turgor limits the compliance of the brain. Compliance is a term used to describe the stretch phase of elasticity in the brain. Compliance allows tissue to deform without damage such as with compression and stretching. Elastance is the complete opposite of compliance. Elastance is the strength of tissues to resist deformation and return to their original shape once the load is removed. Elastance preserves the designs and shapes of structures. On the other hand, the compliance of certain tissues in the brain, especially weak-walled veins, allows them to buffer the impact of the relatively large volume of blood and the associated increase in pressure that is pumped into the cranial vault with each contraction phase of the heart roughly seventy times per minute. The strength of the arterial waves of blood and the pressure pumped in during each heart beat needs to be decreased and modified before sending it into the delicate internal structures of the brain.
The dark grey areas on the bran scan above is CSF. As you can see, CSF fills all the spaces, cracks and caves. The brain is also contained inside the cranial vault and surrounded by CSF that maintains its position and prevents contact with the bones of the vault. Although it is highly porous, the interior and exterior surfaces of the skull are more like limestone or granite in that it has poor permeability. The non-permeable hard shell of the skull protects the brain and keeps the weather out. Although it lacks permeability, the skull is penetrated by many holes called foramen and other openings, which makes it highly porous. Nerves, blood and CSF travel through these openings. Moreover, pressure in these openings can have a profound effect on fluid mechanics in the brain.
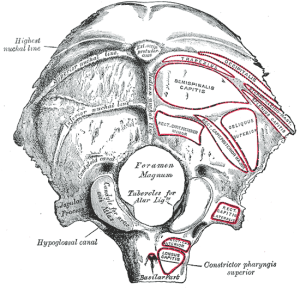 While it is not considered to be a factor that directly affects compliance (elasticity) in the brain, the foramen magnum and spinal canal play an important role in maintaining CSF volume and pressure in the brain. As shown in the picture on the left of the skull base, the foramen magum is the large hole in the base of the skull that connects the cranial vault to the spinal canal. The arterial pulsations and pressure waves that are pumped into the brain by the heart are not only buffered but a proportionate outflow in the amount of blood and CSF is also transferred out of the cranial vault and brain through the foramen magnum and into the spinal canal.
While it is not considered to be a factor that directly affects compliance (elasticity) in the brain, the foramen magnum and spinal canal play an important role in maintaining CSF volume and pressure in the brain. As shown in the picture on the left of the skull base, the foramen magum is the large hole in the base of the skull that connects the cranial vault to the spinal canal. The arterial pulsations and pressure waves that are pumped into the brain by the heart are not only buffered but a proportionate outflow in the amount of blood and CSF is also transferred out of the cranial vault and brain through the foramen magnum and into the spinal canal.Obstruction of venous and CSF pathways in the foramen magnum can affect intracranial pulsatility and pressure waves. In particular it can cause back pressure on the drainage system that results in increased turgor resulting in stiffness due to loss of compliance (elasticity). Obstruction to blood and CSF flow through the foramen magnum can also cause CSF inversion (reverse) flows, turblulence and water hammers in the brain. CSF inversion flows, turbulence and water hammers may play a destructive role that results in damage to periventricular structures.
The most common place for obstruction of CSF outflow to occur is in the craniocervical junction (upper cervical spine). The most common causes of obstruction in the craniocervical junction are malformations and mechanical strains such as misalignments. Obstructions due to malformations and mechanical strains indirectly but significantly affect intracranial compliance (elasticity) and the ability of the brain to absorb and control fluid mechanics caused by heart contractions.
To get a better understanding of how faulty fluid mechanics batter the brain, researchers and engineers are now plugging biphasic poroelastic properties of the brain into computational fluid dynamics and finite element analysis formulas to form computer models to predict and determine the cause of ventriculomegaly. They are also using physics formulas for computational fluid dynamics to determine flow through the different structures of the brain such as the ventricles. The different structures of the brain and the skull have complex shapes and different materials with different degrees of strength and compliance (elasticity), as well as their differing response to hydraulic pressure.
Hydraulic force is a product of pressure multiplied by the size of the area the pressure is being applied to, such as the volume of the ventricles or cisterns for example. A hydraulic pump can be used to increase force by applying pressure to a larger cylinder. Similarly, the pressure from the heart exerts more force on the larger pores and spaces of the brain compared to smaller ones. In this regard, the largest spaces in the brain are the ventricles and cisterns. The effects of hydraulic force may play a role in the ventriculomegaly seen in neurodegenerative condtions such as Alzheimer’s, Parkinson’s and multiple sclerosis. Constant strain from increased force in the ventricles and cisterns may cause a breakdown in the elastic properties of the brain so that the ventricles and surrounding structures can no longer return to their original shape, which is called plastic (permanent) deformation. Dr. Hakim also suggested, many years ago, that the greater size of the ventricles allow them to exert more force and thus maintain the ventriculomegaly with relatively lower pressure (turgor).
In addition to Hakim’s theory regarding ventriculomegaly, my theory regarding mega cisterns, which are enlarged cisterns, is that they are caused by inversion flows, turbulance and hydraulic forces that damage the brainstem and cerebellum resulting in atrophy of nearby structures. Mega Cisterns and atrophy of the brainstem are seen in mega cisterna magna, the Dandy-Walker Complex-Continuum, and a variant form of Parkinson’s disease called olivopontocerebellar atrophy, also known and Shy-Drager Syndrome or Multisystem Atrophy. Understanding these conditions will shed further light on the role of faulty fluid mechanics and hydraulics in neurodegenerative conditions of the brain. I have covered these conditions previously and will cover them more in future posts.
Hydrofracking is a term method engineer’s use to fracture rocks with water pressure. A similar situation called a water hammer can occur in the brain and damage delicate tissues. The location of the periventricular tissues predisposes them to compression, shear forces and water hammers that can cause damage. Loss of compliance in the brain magnifies the destructive forces. My next post will be on hydrofracking and brain atrophy (shrinkage).
For further information on enlargement of the ventricles and autonomic dysfunction called dysautonomia visit my website www.upright-health.com.
Posted in Alzheimer's, CSF, multiple sclerosis, Parkinson's 4 Comments
Pulsatility, Pressure Waves and Neurodegenerative Diseases
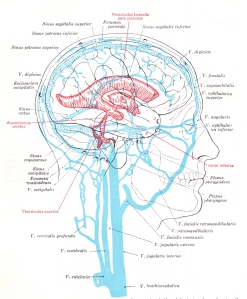 The red colored areas in the picture on the left represent the ventricles of the brain. You can click on the image to enlarge it and get a closer view. The ventricles of the brain contain and produce cerebrospinal fluid (CSF). CSF is mostly water with some sugar and other elements mixed in. CSF leaves the ventricles and enters the subarachnoid cisterns and spaces that surround the entire brain. The subarachnoid cisterns and spaces are part of the protective membranes of the brain and spinal cord called meninges.
The red colored areas in the picture on the left represent the ventricles of the brain. You can click on the image to enlarge it and get a closer view. The ventricles of the brain contain and produce cerebrospinal fluid (CSF). CSF is mostly water with some sugar and other elements mixed in. CSF leaves the ventricles and enters the subarachnoid cisterns and spaces that surround the entire brain. The subarachnoid cisterns and spaces are part of the protective membranes of the brain and spinal cord called meninges.CSF leaves the subarachnoid space and enters the superior sagittal sinus, which is part of the venous drainage system of the brain. The dural sinuses are the large striped blue colored veins in the picture on the left. The veins of the brain also empty into the dural sinuses. They are depicted as the smaller light blue vessels on the surface of the brain. The primary drainage routes of the dural sinuses empty into the internal jugular veins and the vertebral venous plexus of the spine. The internal jugulars and vertebral veins are the large, vertical, blue vessels beneath the skull. Increased pressure or obstruction of the venous outlets of the brain can affect CSF flow and volume. It can also effect pulsatility and pressure waves in the brain which will be explained further below.
 The brain scan on the right is from a paper published in the American Journal of Roetgenology in 2002 called Lesions of the Corpus Callosum: MR Imaging and Differential Considerations in Adults and Children. by E.C. Bourekas and others. The corpus callosum is a large white matter myelinated structure that covers the top of the lateral ventricles. In this image the corpus callosum is the dark grey area above the large white space below the arrows. The large white space is the lateral ventricle which is filled with CSF, and appears white in this image. The arrows are pointing to white spots in the corpus callosum called hyperintensity signals. They indicate demyelinating lesions in the white matter tracts of the corpus callosum.
The brain scan on the right is from a paper published in the American Journal of Roetgenology in 2002 called Lesions of the Corpus Callosum: MR Imaging and Differential Considerations in Adults and Children. by E.C. Bourekas and others. The corpus callosum is a large white matter myelinated structure that covers the top of the lateral ventricles. In this image the corpus callosum is the dark grey area above the large white space below the arrows. The large white space is the lateral ventricle which is filled with CSF, and appears white in this image. The arrows are pointing to white spots in the corpus callosum called hyperintensity signals. They indicate demyelinating lesions in the white matter tracts of the corpus callosum.Interestingly, the ventricles and periventricular areas (which is where the corpus callosum is located) are often involved in neurodegenerative diseases. For example, enlarged lateral ventricles have been associated with normal pressure hydrocephalus (NPH), Alzheimer’s and Parkinson’s disease. NPH is a condition that occurs in adults when the ventricles of the brain become enlarged due to an increase in CSF volume but pressure in the brain, called intracranial pressure, remains normal or just slightly elevated. Parkinson’s disease and Dandy-Walker syndrome are associated with an enlarged fourth ventricle, as well as enlargement of the subarachnoid cisterns. More recently, multiple sclerosis has been associated with an enlarged third ventricle. I cover CSF and the ventricles’ role in the conditions listed above in my book,“The Downside of Upright Posture – The Anatomical Causes of Alzheimer’s, Parkinson’s and Multiple Sclerosis.”
In any case, the enlarged ventricles are typically attributed to atrophy. The cause of the atrophy (decrease in size), however, is often unknown. In this regard, neurodegenerative conditons are also often associated with hyperintensity signals and degeneration of the delicate tissues located next to the ventricles called the periventricular area. Among other things, the periventricular area forms an interface between the brain and ventricles similar to different soil layers called strata or the tectonic plates of the earth. Just like soil strata and tectonic plates, the lobes of the upper brain can similarly slide on the periventricular surfaces of the lower brain and cause a strain.
The periventricular interface contains small blood vessels and delicate myelin covered nerves. Scientists have suspected for decades that myelin is more sensitive to shear stresses and strains. They maintain that enlargement of the ventricles can cause nearby myelin to over-stretch and snap. They further suspect that myelin is more easily damaged by decreases in blood flow (ischemia) and that mechanical stresses and strains may damage the smaller periventricular blood vessels. This could lead to chronic ischemia and atrophy (decrease in size) of the brain. Researchers suggest that the ventricles enlarge to fill the vacated space caused by the atrophy of the surrounding tissues. Interestingly, in addition to atrophy and enlarged ventricles, hyperintensity signals are often in the periventricular areas in Alzheimer’s and multiple sclerosis as mentioned and shown in the brain scan above. Among other things, hyperintensity signals can be a sign of demyelination. They can also be a sign of ischemia. In future posts I will explain how, because of its location, the periventricular area is caught between a rock and a hard place. Consequently, the periventricular area suffers the consequences of faulty hydraulics in the brain.
Researchers are currently studying the potential role of pulsating, strong, high pressure waves in neurodegenerative diseases as a cause of atrophy. The strong, pulsatile, high pressure waves come from the heart which pumps a relatively large volume of blood into the brain with each beat. This causes rhythmical pulsations of increased volume of blood in the brain that produces increased pressure waves that ripple through the entire brain from the point of entry to its exit routes within the cranial vault.
Under normal circumstances, arterial pulsations entering the brain are buffered in and by the subarachnoid cisterns and spaces. The subarachnoid cisterns and spaces are part of the protective membranes that surround the brain called the meninges, mentioned above. The impact of high pressure arterial pulsations from the heart are typically absorbed and reduced in the brain by the elasticity, technically called compliance, of the arteries, veins and the subarachnoid space of the brain and cervical spinal cord. The cervical spinal cord subarachnoid space communicates with the subarachnoid space in the brain.
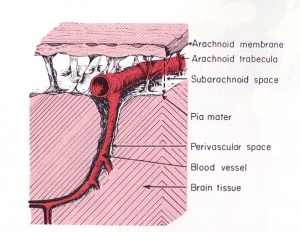 Most of the force from arterial pulsations is normally absorbed by veins in the subarchnoid space which have weak walls that are easily compressed. The impact of arterial pulsations in CSF and the rhythmical compression of the veins help to move venous blood and CSF through their pathways and out of the cranial vault. Scientists suspect that problems can occur if high arterial pressure waves aren’t sufficiently buffered in the subarachnoid space, but instead are directed into the core of the brain and the more delicate micro-sized capillary blood vessels.
Most of the force from arterial pulsations is normally absorbed by veins in the subarchnoid space which have weak walls that are easily compressed. The impact of arterial pulsations in CSF and the rhythmical compression of the veins help to move venous blood and CSF through their pathways and out of the cranial vault. Scientists suspect that problems can occur if high arterial pressure waves aren’t sufficiently buffered in the subarachnoid space, but instead are directed into the core of the brain and the more delicate micro-sized capillary blood vessels.In this regard, studies have shown that excessive pulsatile stresses in the small blood vessels of the brain can change the way their endothelial cells function. Endothelial cells form the innermost lining of blood vessels. They open and close their pores according to chemical and mechanical signals and stresses. Damage to the endothelial cells can affect blood flow. Weakness and thinning of the endothelial cells for example, can make them more susceptible to internal tears and penetration from elements carried in the blood stream such as fats. Constant pounding from high pressure waves can also cause thickening and a decrease in the size of the openings in the endothelial cells and thus decrease blood flow out of the blood vessels. High internal endothelial pressure can also cause stiffness or lack of compliance in the arterial system. In contrast to internal pressure, the small blood vessels can also be effected by external pressures from parts of the brain, the skull or CSF.
Scientists and engineers are now using biphasic poroelastic properties in computational fluid dynamics and finite element analysis to model tissues and fluid mechanics in the brain. Poroelasticity is a complex subject related to geotechnical engineering regarding soils and rocks. It is is also known as the consolidation theory in soil mechanics as first described by professor of physics M.A. Biot from Columbia University. Basically, porous materials contain spaces called pores or voids and are elastic. The flow of fluids through porous materials, such as rocks, is a separate study. Engineers use complex physics formulas and computer programs for computational fluid dynamics to predict hydraulics and fluid flow through soils and rocks.
Fluids inside poroelastic materials affect the material’s structural strength and the way it responds to stresses and strains (deformation). The many different types of soils and rocks all have different types of pores that affect their structural strength and their stability under stresses and strains. In addition to overall strains, engineers use finite element analysis to break down larger macrostrains into smaller microstrains located at intersections along the overall strain.
The brain is loaded with many non-spherical, irregularly shaped pores, ventricles (caves), fissures (cracks), sulci (valleys) and other assorted spaces and shapes that make it difficult to interpret and predict tissue deformation, fluid behavior and hydraulics based on brain scans. Tissue deformation and hydraulics in the brain are important to neurosurgeons for many reasons, including shunt surgery. The use of a mechanical model for more realistic geometry of the brain was proposed decades ago by Dr. S. Hakim, a neurosurgeon, who was one of the pioneers in NPH.
Dr. Hakim published a paper in Surgical Neurology in 1976 called, The Physics of the Cranial Cavity, Hydrocephalus, and Normal Pressure Hydrocephalus: Mechanical Interpretation and Mathematical Model. Dr. Hakim also introduced the concept of the brain being a sponge-like material (poroelastic). More recently, a paper was published by the Oxford University Computing Laboratory in 2004, “A Hydro-elastic Model of Hydrocephalus” by A. Smilie and others, which combines poroelasticity and fluid mechanics to, likewise, construct a mathematical model of the human brain and ventricles. Mathematical models provide clues as to how faulty hydraulics may play a significant role in neurodegenerative diseases.
In brief, for engineering purposes and computer modeling, the fluid mechanics in the cranial vault and and brain can be compared to hydraulic stresses in rocks and soils. My next post will be on the role of poroelasticity in brain pulsations, pressure waves and deformation, such as atrophy and enlarged ventricles. For further information regarding common signs and symptoms of neurodegenerative diseases that are most likely related to hydraulic stresses acting on the third ventricle, such as frequent urination, incontinence, cog fog, heat intolerance, etc., visit my website at upright-health.
Posted in Alzheimer's, CSF, ms lesions, Parkinson's 1 Comment
Blood, CSF and Battered Bones
 Fluid mechanics is the science of liquids, gases and plasmas, as well as the forces that act on them. Hydraulics is based on the science of fluid mechanics and the mechanical properties of fluids.
Fluid mechanics is the science of liquids, gases and plasmas, as well as the forces that act on them. Hydraulics is based on the science of fluid mechanics and the mechanical properties of fluids.Hydraulic pressure is the force exerted by a fluid against a given area such as the inside surface of a container or a pipe. The force is determined by properties of the fluid and the design and dimensions of the container or pipe. In theory, if two containers are linked with a pipe and filled with fluids, force applied against a large container and transmitted via the pipe to a smaller container decreases the force in the smaller container due to the decrease in its size. If pressure is exerted against a container connected to another one of equal size the force stays the same. If the pressure is transmitted to a larger container the force goes up due to the larger size of the area that the pressure is exerted against. In medical sciences, radiologists refer to fluid mechanics and hydraulics in the brain as cranial hydrodynamics.
Cranial hydrodynamics (hydraulics) are driven by cardiorespiratory pressure fluctuations. When the heart contracts it pumps a large quantity of blood into the brain under pressure. It then relaxes, which relieves the pressure. This causes the soft tissues of the brain to rhythmically deform and reform in continuous expansion and contraction cycles. The force cranial hydrodynamics exerts on the different areas of the brain is not uniform. It varies according to the design and dimensions of the different chambers transmitting the force, as well as those that receive it. Thus, a low pressure and force from a smaller chamber can generate greater force when it acts on a larger chamber in the cranial vault.
Poroelasticity is an engineering term used to describe the interaction between rocks and fluids that fill the rock’s pores. External pressue on rocks such as from a large body of water above, pounding waves or large buildings cause rocks to compress which increases pressure on the fluids that fill their pores. Conversely, increased fluid pressure in the pores of rocks such as ice can cause rocks to expand. Over time, poroelastic mechanics can cause rocks and soils to settle, subside, crack and deform. Poroelasticity can be used to describe deformation of the bones of the cranial vault and the deformation of the brain due obstruction of cerebrospinal fluid (CSF) flow.
Caves, caverns and cavities in rocks are often formed by the force of water. In this regard, the skull is a stone structure comprised of many rocks surrounding enclosed caves, caverns, cavities and pores formed in part by cranial hydrodynamics and the force of water. The cranial vault, for example, is a large fluid filled cave. Inside the cranial vault, the tough outer coat of the brain, called dura mater divides the cranial vault into caverns called fossas. It also forms caverns called dural sinuses. The openings in the skull called fissures and foramen are cavities that penetrate the bone stones of the skull. All bones have pores but the bones that cover the cranial vault have special, extra-large pores called diploic spaces located between the inner and outer plates of the skull bones. The dipolic spaces contain valveless veins. The diploic spaces and veins insulate, cool and help to maintain the temperature of the brain.
The bones of the cranial vault are like rocks constantly battered by blood and cerebrospinal fluid (CSF). The high pressure in the arteries is strong enough that it causes deformation leaving their distinct impression on the roof of the skull. Blood pressure in the veins is much lower so they don’t cause as much deformation and imprints on the skull bones. The largest veins of the brain called the dural sinuses, such as the superior sagittal sinus, the transverse and sigmoid sinuses, however, influence the shape of the special joints of the skull called sutures. The imprint they leave however, isn’t the same as the arterial imprints. Instead they leave behind a strange looking zig zag pattern similar to surgical sutures or stitches used in sewing.
Interestingly, the inside surface of the sutures of the skull next to the sinuses shows much smaller deformation, comparatively speaking, than the outside surface. The outer surface of the sutures and skull is instead effected by the much smaller diploic veins. The deformation and impression they leave behind are large and erratic and get progressively larger toward the back and bottom of the skull. I discussed the shape of the sutures in previous posts. They are a reflection of fluid mechanics in the brain. Suffice it to say that their shapes are not like veins but instead suggest lateral strains such as from water that sloshes from side to side in bucket while being carried.
 In addition to arteries and veins, cerebrospinal fluid (CSF) can also batter the bones of the skull. Left unchecked, CSF can cause the skull to enlarge in a child with hydrocephalus or Dandy-Walker syndrome. The previous post discussed Dandy-Walker Syndrome in children which is often associated with hydrocephalus and enlargement of the posterior fossa.
In addition to arteries and veins, cerebrospinal fluid (CSF) can also batter the bones of the skull. Left unchecked, CSF can cause the skull to enlarge in a child with hydrocephalus or Dandy-Walker syndrome. The previous post discussed Dandy-Walker Syndrome in children which is often associated with hydrocephalus and enlargement of the posterior fossa.The picture above on the right is of a child’s skull that was effected by hydrocephalus. Notice that the bones that typically make up the base of the skull all around the area where the ear would be are broken into many smaller sections. Those small sections of bone are called wormian or sesamoid bones. They are caused by rapid expansion of the skull, which stretches the bone to its limits. Bone development can’t keep pace and imperfections develop and voids are filled with pieces of bones to patch things over. They are similar to rock fractures caused by ice expansion and other internal forces inside the pores.
CSF is produced from blood and driven by pulsations from the circulatory system and respiration. Although it is extremely low compared to blood pressure, the hydraulic force from the pulsations of cerebrospinal fluid are strong enough to erode and leave impressions in the bones that form the roof over the cranial vault. Physical anthropologists and forensic scientists call the pits in the skull caused by CSF pulsations Pacchionian or arachnoid impressions. They are caused by the arachnoid granulations. The impressions are also known as granular foveolae. If you click on the picture at the top left of the page, you can see a large Pacchionian impression above the letter “e” in the word “bone.” A much smaller round Pacchionian impression can be seen above the larger one. As an aside, this skull also shows hyperostosis, which is associated with excess growth and thicker bones. Hyperostosis is sometimes associated with an increase in intracranial pressure due to the decrease in the inside dimensions and thus capacity of the cranial vault.
The superior sagittal sinus is located at the top of the brain. Several large reservoirs of veins called venous lacunae (lakes) are located on either side of the superior sagittal sinus. Venous blood from the brain enters the venous lacunae. CSF from the subarachnoid spaces flows through the one way valves of the arachnoid granualtions and into the venous lacuna and superior sagittal sinus. Lacuna means lake because its a large venous reservoir. This means that the pressure exerted by the smaller container of CSF against the larger venous lacuna increases the force acting on them. The force it generates is strong enough to put a dent in the roof of the skull. Blood in the venous lacuna then empties into the superior sagittal sinus and travels down through the transverse and sigmoid sinuses and into the internal jugular and the vertebral veins located in the posterior fossa.
The thought first occured to me decades ago when I first saw Pacchionian impressions and skulls with hydrocephalus, that if CSF is powerful enough batter and erode bone, then it certainly must be strong enough to batter and erode the much softer tissues of the brain. Recent evidence from studies being done in Latham, New York, by Dr. Scott Rosa using an upright phase contrast cine MRI by FONAR Corporation continue to confirm my hypothesis. The areas I have seen effected are the front of the posterior fossa called the clivus and the rear of the fossa called the supraocciput. Interestingly, among other things, radiologists look for erosion of the clinoid process of the clivus as a sign of increased intracranial pressure. Another potential sign they look for is an empty sella, which I discussed in previous posts. CSF backjets and turbulent flows can indeed erode bone. Moreover, in addition to bone, chronic CSF backjets and inversion flows can batter and erode the brain by similar hydraulic effects.
Normal pressure hydrocephalus (NPH) is a condition seen in adults and has been associated with Alzheimer’s and Parkinson’s diseases. More recently it has been implicated in multiple sclerosis. In NPH the ventricles, likewise, become enlarged but intracranial (CSF) pressure remains normal or just slightly elevated. In addition, the size of the skull is normal but the brain decreases in size. The decrease is currently blamed on atrophy. It puzzles researchers and engineers how low pressure conditions can cause the ventricles to enlarge. It is my opinion that it may be due to erosion and subsequent atrophy caused by constant battering of the brain by aberrant CSF flow. What’s more, it’s not just the pressure that does the damage in NPH. The force generated by the hydraulic pressures acting on the designs and dimensions of different parts of the brain has to be considered as well. In my next, post I will discuss how CSF can similarly batter the brain and cause it to shrink in size while pressure remains normal or just slightly elevated due to hydraulics and poroelasticity.
Posted in Alzheimer's, CSF, multiple sclerosis, Parkinson's 3 Comments
CSF and Cerebellar Symptoms in Alzheimer’s, Parkinson’s and MS
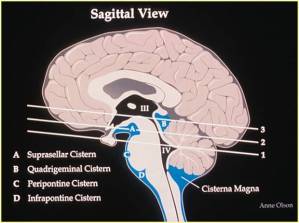 The cerebellum is often affected in neurodegenerative diseases such as Alzheimer’s,, Parkinson’s and multiple sclerosis (MS). Cerebellar signs include: problems with posture, balance, gait (walking) and coordination. Muscle coordination problems include disturbances in movements of the eyes such as nystagmus, as well as intention tremors and over shooting movements when attempting to do specific tasks with the arms or legs. Cerebellar signs can also include problems with speech, vertigo, nausea and vomiting. In this regard the cerebellum is often affected in different neurodegenerative diseases due its location in the posterior fossa above the foramen magnum.
The cerebellum is often affected in neurodegenerative diseases such as Alzheimer’s,, Parkinson’s and multiple sclerosis (MS). Cerebellar signs include: problems with posture, balance, gait (walking) and coordination. Muscle coordination problems include disturbances in movements of the eyes such as nystagmus, as well as intention tremors and over shooting movements when attempting to do specific tasks with the arms or legs. Cerebellar signs can also include problems with speech, vertigo, nausea and vomiting. In this regard the cerebellum is often affected in different neurodegenerative diseases due its location in the posterior fossa above the foramen magnum.The brain floats inside a jacket of water. The jacket of water includes the enlarged spaces, called cisterns (wells) beneath the bottom of the brain and surrounding the brainstem and cerebellum. The cisterns are the blue spaces in the drawing above from a neurology lecture by Dr. Anne Olsen. The cisterns support the brain and protect and cushion it from the hard walls of the cranial vault.
The cisterna magna is the largest of the cisterns and is located inferior to (below the bottom of) the cerebellum. The volume of cerebrospinal fluid (CSF) in the cisterna magna and other cisterns is crititcal to the health and function of the brainstem and cerebellum. An increase or a decrease in the normal volume of CSF in the cisterns can cause problems in the brainstem and cerebellum. For example, an insufficient volume of CSF can cause the brainstem and cerebellum to sink into the foramen magnum. On the other hand, it is my opinion that a chronic abnormal increase in CSF volume in the cisterns can lead to compression and subsequent degeneration of the brainstem and cerebellum.
Typically, hydrocephalus is associated with an increase in CSF volume in the chambers in the middle of the brain and brainstem, called ventricles, where it is produced. There is debate among experts, however, as to whether to include any abnormal increase in CSF volume inside the cranial vault, which would include those that can occur outside the ventricles in the subarachnoid spaces and cisterns located between the outer and middle layers of the protective membranes, called meninges, that surround the brain and cord. Currently, an increase in CSF volume in the cisterna magna is called a mega cisterna magna or a cystic posterior fossa. At this time, a mega cisterna magna is not considered to be a form of hydrocephalus but it is sometimes associated with hydrocephalus and enlarged ventricles in a rare condition called Dandy-Walker syndrome.
 Dandy-Walker syndrome is a congenital condition associated with a malformed and undersized cerebellum. The MRI on the right is an example of a Dandy Walker syndrome from a paper published in 2008 in the Internet Journal of Radiology called, Imaging of Congenital Malformations of the Brain by A.B. Shinagare and N.K. Patil from the Department of Radiology in Mumbai. The white arrow points to the cerebellum. The white dart points to the cover over the cerebellum and posterior fossa, which is exceptionally steep. The black dart near the bottom of the posterior fossa points to a dark gray area beneath the cerebellum. The dark gray is CSF in the cisterna magna of the posterior fossa. The black arrow points to the rear side of the pons portion of the brainstem, which is slightly compressed.
Dandy-Walker syndrome is a congenital condition associated with a malformed and undersized cerebellum. The MRI on the right is an example of a Dandy Walker syndrome from a paper published in 2008 in the Internet Journal of Radiology called, Imaging of Congenital Malformations of the Brain by A.B. Shinagare and N.K. Patil from the Department of Radiology in Mumbai. The white arrow points to the cerebellum. The white dart points to the cover over the cerebellum and posterior fossa, which is exceptionally steep. The black dart near the bottom of the posterior fossa points to a dark gray area beneath the cerebellum. The dark gray is CSF in the cisterna magna of the posterior fossa. The black arrow points to the rear side of the pons portion of the brainstem, which is slightly compressed.A normal healthy cerebellum should nearly fill the posterior fossa. In this case the cerebellum is extremely small. The malformation of the cerebellum is currently believed to be do to underdevelopment (atrophy), or to total lack of development (atresia). The increase in CSF volume in the cisterna magna is attributed to the decrease in size of the cerebellum. In other words, CSF simply moves in to fill the empy space.
Interestingly, Dandy-Walker syndrome is the complete opposite condition to a Chiari malformation. For example, Chiari malformations are often associated with an undersized posterior fossa. In Dandy-Walker, the posterior fossa is often enlarged. In Chiari malformations, a normal sized cerebellum gets pushed down into the foramen magnum. In Dandy-Walker the cerebellum is underdeveloped and small. Moreover, it often gets pushed up into the posterior fossa of the cranial vault along with the cover over the fossa, called the tentorium cerebelli. In Chiari malformations the cisterna magna is often compressed due to the descent of the cerebellum into the foramen magnum. In Dandy-Walker syndrome the cisterna magna is enlarged. Chiari malformations are also associated with an undersized foramen magnum. Dandy-Walker, on the other hand, is associated with an oversized foramen magnum. Chiari malformations also affect females about three times as often as males. On the other hand, at approximately sixty percent, males make up more than half the cases of Dandy-Walker syndrome. The one characteristic both conditions do share in common is that their cause is often unknown.
In Dandy-Walker the problem is believed to be caused by undersized or absent outlets that normally connect the fourth and lowest ventricle to the cisterns below. The fourth ventricle is located between the front of the cerebellum in the back and the pons of the brainstem in the front. It can be seen in the sketch of the cisterns at the top of the page indicated by the Roman numeral IV in the black space. The third ventricle is above it and is indicated by the Roman numeral III in the black space. The narrow black streak joing them is called the cerebral aqueduct.
The obstruction to CSF flow from the fourth ventricle to the cisterns causes the fourth ventricle to enlarge. Chronic enlargement of the fourth ventricle can compress and damage the cerebellum. In Dandy-Walker syndrome, the enlarged fourth ventricle is referred to as a cystic fourth ventricle. Because it involves the ventricles, a cystic fourth ventricle is technically a form of hydrocephalus. On the other hand, the enlarged cisterna magna seen in certain cases of Dandy-Walkers syndrome is not. Instead, the enlarged cistern is attributed to an underdevelopment resulting in an undersized cerebellum. CSF increases in volume in the cisterna magna as a result of the decrease in size of the cerebellum. Since the cisterns are outside the ventricles, technically speaking it is not hydrocephalus.
This is similar to the theory regarding the suspected cause of enlarged ventricles often seen in normal pressure hydrocephalus (NPH), which has been associated with Alzheimer’s disease, dementia and Parkinson’s disease as well as others. In Alzheimer’s disease the enlarged ventricles are attributed to atrophy; that is, a decrease in size of the brain. In other words, as the brain shrinks in size the ventricles enlarge and CSF volume increases to compensate for the decrease in size of the brain and to fill in the space.
While some cases of Dandy-Walker are clearly associated with undersized, blocked or absent CSF pathways, many are not. The problem is further complicated because the development of the ventricles, as well as the cisterns and CSF pathways start in utero (during preganancy) and continues after birth, which is when problems start to show up. Moreover, the skull is still open at birth, which allows it to accomodate an increase in CSF volume. Consequently, unless it is associated with an oversized head due to hydrocephalus, the problem often goes unnoticed initially . Whatever the cause, experts all agree that Dandy-Walker syndrome is associated with an imbalance between the rate of production of CSF and its absorption and removal from the brain.
Considering the above, both blood and CSF flow between the brain and cord pass through the foramen magnum and upper cervical spinal canal. Consequently, blockage of blood and CSF flow through the foramen magnum and upper cervical spinal canal can cause inversion flows, turbulance and standing waves to form in the brain, especially in the cisterna magna, which can affect the cerebellum among other things. It can also cause the posterior fossa and foramen magnum to enlarge similar to the affects of hydrocephalus on the upper portion of the cranial vault. This could explain the enlarged posterior fossa and foramen magnum in Dandy-Walker syndrome. Furthermore, it is my contention that chronic obstruction to CSF flow causes local turbulance, inversion flows and standing waves (clapotis) in the brain that can compress and erode the brain.
Other cisterns can similarly be affected in conditions that affect adults. For example, there is a variant of Parkinson’s disease called multi-system atropy (MSA) or olivopontocerebellar atrophy (OPCA) in which the cerebellum and sometimes parts of the brainstem, called the olives and pons, appear small and compressed similar to Dandy-Walker. It is my theory that many cases of Parkinson’s disease and variants of Parkinson’s are due to obstruction to CSF flow oftentimes due to Chiari malformations, which block blood between the brain and cord in the foramen magnum and upper cervical spinal canal. Moreover, obstruction to CSF flow most likely plays a role in multiple sclerosis and Alzheimer’s disease as well. The first place to feel the affect of blockage of CSF flow is the posterior fossa, which contains the brainstem and cerebellum.
In brief, hydrocephalus is associated with children. In contrast to children, adults get normal pressure hydrocephalus. Similarly, Chiari malformations and Dandy-Walker syndromes are associated with children. More recently however, it has been shown that adults can aquire Chiari 1 type malformations, and olivopontocerebellar atrophy (a variant of Parksinson’s) causes similar signs on brain scans to Dandy-Walker syndrome. In many cases they may share a similar cause, which is blockage of CSF flow that results in an imbalance between its rate of production and removal from the brain. Among other things, an increase in CSF volume in the fourth ventricle or cisterns can affect the cerebellum.
For further information on CSF flow and volume in the cisterns, dysautonomia and heat intolerance, visit my website at www.upright-health.com.
The Cisterns and Cine CSF Flow Studies
 The unusual images on the left and below were taken of the head and neck area looking at the patient from the side. The face is on the left side of the image. The images are called cine MRI because they are similar to cinema photography. In cinema photography many still pictures are taken and played back at high speed, which make the images appear to be moving.
The unusual images on the left and below were taken of the head and neck area looking at the patient from the side. The face is on the left side of the image. The images are called cine MRI because they are similar to cinema photography. In cinema photography many still pictures are taken and played back at high speed, which make the images appear to be moving.In this image the speckled black and white areas are air surrounding the patient, as well as air in the paranasal (air) sinuses, the nose, the mouth and the throat. The more uniform gray area is the patient’s skin, fat, bones and muscles. If you click on the image you will see the movement of cerebrospinal fluid (CSF). The streaks of black that quickly appear and disappear in the moving image is cerebrospinal fluid (CSF), which is mostly water with sugar and some other elements mixed in. Although this particular image shows CSF flow, cine MRI can also be used to show blood flow.
These cine MRI images are from the FONAR Corporation. FONAR Corporation was founded by Dr. Raymond Damadian who was instrumental in the development of today’s modern MRI scanners. More recently, Dr. Damadian invented the upright MRI, which is going to change the way we see injuries, degenerative changes and diseases of the spine, brain and cord. The images are from a study by Dr. Damadian of eight patients with multiple sclerosis called, The Possible Role of Cranio-Cervical Trauma and Abnormal CSF Hydrodynamics in the Genesis of Multiple Sclerosis, published in the journal of Physiological Chemistry and Physics and Medical NMR in 2011. All of the eight cases were associated with trauma and all of them showed obstruction of CSF flow. The image below on the right is one of the cases.
The problem with conventional MRIs is that they are taken with the patient lying down. The problem is that upright posture causes significant changes in the mechanical loads acting on the spine, as well as fluid flow in the brain and cord. In contrast to humans, in most mammals the primary forces acting on the spine, while standing on four legs, are tension and shear stresses. In humans, upright posture primarily causes compression loads on the segments of the spine. Compression causes the segments of the spine to cave, bulge and slip in different directions when there is instability. Many conditions of the spine, brain and cord appear normal or acceptable when an MRI is taken with the patient lying down because the abnormalities only show when the patient is upright. Dynamic or kinematic upright MRI takes images in different positions, such as foward or backward bending of the spine. Dynamic MRI images picks up even more problems that might otherwise be missed by upright MRI alone.
As mentioned above, cine MRI images use fast moving still pictures that are taken in pixels and digitized for computerized imaging. The cameras are gated. Gated simply means that the MRI cameras are timed to take the images at particular intervals. In this case they are gated (timed) to take images based on the beat of the heart. In these images, CSF (on it’s way out of the brain) appears as flashing streaks of black on the front and back side of the brain and cord. It then quickly disappears. The black streaks show up when a large volume of blood is pushed into the cranial vault and brain by the contraction of the heart. As it does, an equal amount of venous blood and CSF is driven out of the cranial vault and into the spinal canal and cord. If you study the images closely you will notice that the image at the top of the page shows a clear continuous and uninterrupted normal pattern of CSF flow between the brain and cord, as well as a champagne glass shape to the passages. Click on the image below and compare the differences.

In the moving image you see black streaks the same as in the normal cine CSF flow study above, but the streaks are interrupted in certain areas or not as dark. If you look at the area the black arrow is pointing to you will see that the dark streak suddenly stops compared to the normal cine CSF MRI image above. If you look for the shape of the champagne glass you will see it is barely noticeable or missing on the back side. Instead, there is a dark streak with intense white streaks within located at the top of the champagne glass in the back of the brain. Those mixed black and white streaks are out of synchrony with the normal flow of CSF and they are probably going in the wrong direction. In other words, they are turbulant inversion flows or backjets of CSF in the brain. They could also be standing waves, or as kayakers prefer to call them, clapotis.
The dural sinuses (veins) that drain blood from the brain during upright posture follow a similar course to the CSF seen as black streaks in these images and empty into the vertebral veins inside the spinal canal. When the heart contracts, venous blood is driven out of the cranial vault along with CSF and both must exit together through the foramen magnum in the base of the skull and into the spinal canal. The vertebral veins are located between the walls of the spinal canal and the outer covering of the cord called the dura mater. The space is thus called the epidural space. CSF passes through the subarachnoid space inside the cord. Therefore, if venous blood flow becomes obstructed in the epidural space at or below the foramen magnum in the cervical spinal canal, the hydraulic pressure that follows is transmitted to the subarachnoid space of the cord and can affect CSF flow.
It has been my theory for the past 30 years that the blockage of CSF flow is most likely one of the root causes of neurodegenerative diseases of the brain such as Alzheimer’s, Parkinson’s, and multiple sclerosis. A decrease in CSF flow can affect the brain in several ways. One of the ways I suspect it causes damage to the brain is from backjets (and turbulance) of CSF in the cisterns of the brain. The cisterns are on the front and back side of the brain stem and cerebellum. The outline of the cisterns in these images is the champagne glass shape. Over time, chronic CSF backjets, turbulance and standing waves can compress and damage the brain.
There are many conditions of the spine that can affect blood and CSF flow in the brain and cord. For further information on increased CSF volume and backjets in the cisterns check out my website page on atrophy dysautonomia. Or visit the website at www.upright-health.com.
CSF Cistern Compression of the Brainstem
CSF and blood are pumped into the brain under pressure similar to a bicycle pump filling a tire tube. The pressure of the pump comes from the heart and lungs. Since the brain is housed inside a closed container, which is filled to capacity, the increase in blood volume must be offset by a decrease in venous blood and cerebrospinal fluid (CSF). This is accomplished by pushing a proportionate amount of blood and CSF out through the large opening in the base of the skull called the foramen magnum and into the spinal canal.
Typically, when a radiologist views x-rays or MRI’s of the spine they don’t consider misalignments of the upper cervical spine or degeneration and changes in the normal curves of the lower spine to be a problem unless it causes contact with the spinal cord. This disregards the impact on the vertebral veins that are located between the spinal canal and cord. As the heart contracts blood and CSF are pushed into the spinal canal at the same time and thus compete for available space.
Humans use the occipital marginal sinus and emissary veins to drain the brain during upright posture. These veins empty into the vertebral veins of the spine. Misalignments of the upper cervical spine can affect blood and CSF flow as it passes between the cranial vault and spinal canal. Likewise, spondylosis (degenerative changes), stenosis (narrowing of the spinal canal) and scoliosis (abnormal curves) in the lower spine can also affect blood and CSF flow between the cranial vault and spinal canal.
 The picture on the left is used with permission from Johan Linder of Clapotis Sea Kayak in Sweden. The pumping of the heart causes CSF waves to form in the brain and spinal cord. Respiration further increases the size of the waves. More than the heartbeat or respiration, upright posture significantly increases the pressure of the waves that form at the bottom of the cranial vault. (To see the affects of upright posture venous pressure inside the skull see my previous posts with pictures of the sutures).
The picture on the left is used with permission from Johan Linder of Clapotis Sea Kayak in Sweden. The pumping of the heart causes CSF waves to form in the brain and spinal cord. Respiration further increases the size of the waves. More than the heartbeat or respiration, upright posture significantly increases the pressure of the waves that form at the bottom of the cranial vault. (To see the affects of upright posture venous pressure inside the skull see my previous posts with pictures of the sutures).
When waves collide they cause standing waves called clapotis. If waves of blood and CSF from the brain collide with waves in the cervical spine they will cause inversion (reverse) flows and standing waves to form in the cisterns that surround the brainstem and cerebellum. Chronic standing waves may lead to compression and subsequent malfunction and degeneration of the structures they surround. Increased CSF volume, backjets (inversion flows) and standing waves in the CSF may play a role in neurodegenerative diseases.
Multisystem atrophy (MSA) is a variant of Parkinson’s disease associated with dysautonomia and cerebellar signs. Dysautonomia is dysfunction (malfunction) of the autonomic (vegetative) nervous system which regulates all the vital and internal functions of the body. The cerebellum is important to posture, coordination, balance and gait (walking). Many neurodegnerative diseases are similarly associated with dysautonomia and cerebellar signs.
 There is a variant of MSA formerly referred to as olivopontocerebellar atrophy. It is associated with dysautonomia. It is also associated with atrophy, which means a decrease in the size of the brainstem and cerebellum. I suspect the atrophy is due to obstruction of CSF flow between the brain and cord that eventually erodes the brainstem and cerebellum similar to the impact of relentless pounding of waves of the Atlantic against the northeast coastline of North America.
There is a variant of MSA formerly referred to as olivopontocerebellar atrophy. It is associated with dysautonomia. It is also associated with atrophy, which means a decrease in the size of the brainstem and cerebellum. I suspect the atrophy is due to obstruction of CSF flow between the brain and cord that eventually erodes the brainstem and cerebellum similar to the impact of relentless pounding of waves of the Atlantic against the northeast coastline of North America.
The relentless pounding of waves can tear apart rocks. They can similarly compress and erode the brain. For further information on CSF, cisterns, atrophy of the brainstem, dysautonomia, cerebellar signs and Parkinsonism visit my website at www.upright-health.com or click on the link above.
Typically, when a radiologist views x-rays or MRI’s of the spine they don’t consider misalignments of the upper cervical spine or degeneration and changes in the normal curves of the lower spine to be a problem unless it causes contact with the spinal cord. This disregards the impact on the vertebral veins that are located between the spinal canal and cord. As the heart contracts blood and CSF are pushed into the spinal canal at the same time and thus compete for available space.
Humans use the occipital marginal sinus and emissary veins to drain the brain during upright posture. These veins empty into the vertebral veins of the spine. Misalignments of the upper cervical spine can affect blood and CSF flow as it passes between the cranial vault and spinal canal. Likewise, spondylosis (degenerative changes), stenosis (narrowing of the spinal canal) and scoliosis (abnormal curves) in the lower spine can also affect blood and CSF flow between the cranial vault and spinal canal.
 The picture on the left is used with permission from Johan Linder of Clapotis Sea Kayak in Sweden. The pumping of the heart causes CSF waves to form in the brain and spinal cord. Respiration further increases the size of the waves. More than the heartbeat or respiration, upright posture significantly increases the pressure of the waves that form at the bottom of the cranial vault. (To see the affects of upright posture venous pressure inside the skull see my previous posts with pictures of the sutures).
The picture on the left is used with permission from Johan Linder of Clapotis Sea Kayak in Sweden. The pumping of the heart causes CSF waves to form in the brain and spinal cord. Respiration further increases the size of the waves. More than the heartbeat or respiration, upright posture significantly increases the pressure of the waves that form at the bottom of the cranial vault. (To see the affects of upright posture venous pressure inside the skull see my previous posts with pictures of the sutures).When waves collide they cause standing waves called clapotis. If waves of blood and CSF from the brain collide with waves in the cervical spine they will cause inversion (reverse) flows and standing waves to form in the cisterns that surround the brainstem and cerebellum. Chronic standing waves may lead to compression and subsequent malfunction and degeneration of the structures they surround. Increased CSF volume, backjets (inversion flows) and standing waves in the CSF may play a role in neurodegenerative diseases.
Multisystem atrophy (MSA) is a variant of Parkinson’s disease associated with dysautonomia and cerebellar signs. Dysautonomia is dysfunction (malfunction) of the autonomic (vegetative) nervous system which regulates all the vital and internal functions of the body. The cerebellum is important to posture, coordination, balance and gait (walking). Many neurodegnerative diseases are similarly associated with dysautonomia and cerebellar signs.
 There is a variant of MSA formerly referred to as olivopontocerebellar atrophy. It is associated with dysautonomia. It is also associated with atrophy, which means a decrease in the size of the brainstem and cerebellum. I suspect the atrophy is due to obstruction of CSF flow between the brain and cord that eventually erodes the brainstem and cerebellum similar to the impact of relentless pounding of waves of the Atlantic against the northeast coastline of North America.
There is a variant of MSA formerly referred to as olivopontocerebellar atrophy. It is associated with dysautonomia. It is also associated with atrophy, which means a decrease in the size of the brainstem and cerebellum. I suspect the atrophy is due to obstruction of CSF flow between the brain and cord that eventually erodes the brainstem and cerebellum similar to the impact of relentless pounding of waves of the Atlantic against the northeast coastline of North America.The relentless pounding of waves can tear apart rocks. They can similarly compress and erode the brain. For further information on CSF, cisterns, atrophy of the brainstem, dysautonomia, cerebellar signs and Parkinsonism visit my website at www.upright-health.com or click on the link above.
Posted in Alzheimer's, chiari malformations, CSF, multiple sclerosis, Parkinson's Tagged csf flow, upper cervical spine, vertebral veins Leave a comment
Cervical Spondylosis and CSF Flow in the Cisterns

The brain is surrounded by a watery substance called cerebrospinal fluid (CSF), which is produced in chambers called ventricles located in the middle of the brain. In the MRI image on the right, the brain is white and CSF is black. The CSF pathways for the most part are smooth and there are no obstructions.
CSF volume and pressure in the brain change with the contraction and relaxation cycles of the heart. When the heart contracts, a large volume of blood in the arteries is driven into the brain. To compensate for the increase in arterial blood volume a proportionate amount of venous blood and CSF is squeezed out of the cranial vault and into the spinal canal.
The outflow of blood and CSF is affected by the design, dimensions and alignment of the foramen magnum in the bottom of the skull and the spinal canal of the upper cervical spine. Many inherited (genetic) and acquired conditions of the base of the skull and upper cervical spine can decrease blood and CSF flow through the foramen magnum and upper cervical spine. Inherited conditions include: Arnold-Chiari malformations, Dandy-Walker syndrome, craniosynostosis, Klippel-Feil (fused cervical segments) occipitalization (fused upper cervical spine and skull), as well as others. Aquired conditions include aging and injuries. Aging causes muscles, bones and connective tissues to degenerate, which can affect the tunnels nerves and blood vessels pass through. Injuries cause similar problems and hasten degeneration associated with aging.
 Cervical spondylosis is a general term used to describe degenerative conditions of the cervical portion of the spine. Spondylosis can also occur in the thoracic and lumbar spine as well. All forms of spondylosis affect the design, dimensions and alignment of the spinal canal. The spinal canal is a tunnel that contains the spinal cord. It also contains arterial blood vessels that supply the spinal cord with fresh oxygenated blood and the verebral venous plexus, which is a dense network of veins, that drains the spinal cord and brain. The remainder of the space is filled with loose fat.
Cervical spondylosis is a general term used to describe degenerative conditions of the cervical portion of the spine. Spondylosis can also occur in the thoracic and lumbar spine as well. All forms of spondylosis affect the design, dimensions and alignment of the spinal canal. The spinal canal is a tunnel that contains the spinal cord. It also contains arterial blood vessels that supply the spinal cord with fresh oxygenated blood and the verebral venous plexus, which is a dense network of veins, that drains the spinal cord and brain. The remainder of the space is filled with loose fat.After passing through the foramen magnum and spinal canal of the upper cervical spine, venous blood and CSF that has been squeezed out of the brain during contraction of the heart and exhalation must flow through the lower cervical spinal canal. In the picture above on the left the brain is black and CSF is white. If you look closely at the cervical spine you will notice that the spinal canal is constricted due to spondylosis. In medical terms it is called stenosis, which means narrow. The cause of the stenosis in this case is spondylosis (degeneration of the spine).
 In a previous post called CSF, Cisterns, Clapotis and Cysts, I discussed seawalls and standing waves called clapotis. The picture on the right is of Thunder Hole in Acadia National Park off the coast of Maine in North America. Over time the ocean eroded the shoreline and formed a tight canal. The water speeds up as it passes through the tight canal and crashes into the wall at the end causing it to sound like thunder and shoot straight up into the air.
In a previous post called CSF, Cisterns, Clapotis and Cysts, I discussed seawalls and standing waves called clapotis. The picture on the right is of Thunder Hole in Acadia National Park off the coast of Maine in North America. Over time the ocean eroded the shoreline and formed a tight canal. The water speeds up as it passes through the tight canal and crashes into the wall at the end causing it to sound like thunder and shoot straight up into the air.Alterations in the design and dimensions of the lower cervical spine such as from cartilage and connective tissue degeneration can affect blood and CSF flow in the spinal canal similar to land masses that jut out into rivers. Land masses and seawalls reflect incoming waves that then travel back out to sea. When they meet up with another incoming wave the two combine and form a standing wave that is twice the size of the individual waves.
If the design and dimensions of the cervical spinal canal are correct, the blood and CSF will flow smoothly with little resistance. If the path is obstructed by cervical spondylosis (degeneration) their flow will become turbulent. If it becomes sufficiently restricted and turbulent it will cause back pressure and standing waves to form in the brain. Overtime, standing waves can tear apart shorelines. They can similarly damage the brain.
The first areas to receive the brunt of the standing waves are the basal cisterns of the brain. The cisterns are dilated pouches in the subarachnoid space in the outer coverings of the brain. The cisterns are filled with CSF and protect the brain from contact with bones of the base of the skull. The subcompartment in the base of the skull, called the sella turcica for the pituitary gland is also affected. An increase in CSF volume and pressure in the cisterns and sella turcica can cause problems in the brainstem and pituitary gland. It may also explain why some patients with neurodegenerative diseases have problems with the autonomic nervous system referred to as dysautonomia.
Standing waves may play a role in Dandy-Walker syndromes, Arnold-Chiari malformations, arachnoid cysts, empty sella syndromes, multiple sclerosis, Parkinson’s disease, Shy-Drager syndrome, Alzheimer’s disease and other neurodegenerative conditions.
For more information on spondylosis visit my website http://www.upright-health.com/cervical-spondylosis.html .
CSF Fountains, Pulsations and Flow
 The famous neurosurgeon Dr. Harvey Cushing stated that cerebrospinal fluid (CSF) flow is the third circulation of the brain. More recently in chapter six of Clinical Neurology published by Lippencott in 2006, Dr. Joseph Madson and others elaborated on Dr. Cushings description of CSF flow. They stated that CSF pulsations are the fourth circulation of the brain.
The famous neurosurgeon Dr. Harvey Cushing stated that cerebrospinal fluid (CSF) flow is the third circulation of the brain. More recently in chapter six of Clinical Neurology published by Lippencott in 2006, Dr. Joseph Madson and others elaborated on Dr. Cushings description of CSF flow. They stated that CSF pulsations are the fourth circulation of the brain.The open sutures, as seen in the picture, on an infants skull are called fontanelles , which means little fountains. They are known as “soft spots” in layman’s terms. The soft spots were so named because you can feel the pulsations of the brain at the fontanelles.
The fontanelles separate the plates of bone that cover the brain called membranous bones. They are called membranous bones because they grow within the outside covering of the brain and develop along with the brain. The membrane of the brain is made of dura mater, which means hard mother in Latin, so the soft spots aren’t as soft as they appear. They are actually relatively tough and difficult to penetrate. If you look closely at the infant skull above you will notice that the edges of the sutures are relatively smooth compared to the adult skull below. The sutures develop their characteristic shape as an infant matures. In either case, like all bones, their shapes are caused by the stresses that strained them.
If a baby becomes dehydrated the soft spots will sink. On the other hand, if the volume of cerebrospinal fluid in the brain increases, such as in hydrocephalus, the soft spots will feel tense and bulge outward. Typically, the fontanelles eventually disappear and the membranous bones are joined by their opposing surface that form into the shapes of surgical sutures. Hense the joints of the skull are called sutures.
Hydrocephalus in children is caused by blockage of CSF flow. The blockage of CSF flow causes the volume of CSF in the brain to increase. The increase in CSF volume causes the sutures to stay open and the head to increase in size. On the other hand, in some cases, there is premature closing of the sutures called craniosynostosis. Most cases of craniosynostosis cause mild almost imperceptible malformations of the skull and have no impact on health. In certain cases, however, premature closure of the sutures can cause hydrocephalus due to resistance to growth and development of the brain and subsequently CSF volume.
 In any case, the shape of the soft spots and sutures of the skull are a reflection of cranial hydrodynamics, which is fluid mechanics in the brain and skull. The fluid mechanics are the result of electrical, circulatory and respiratory waves. Those waves are further amplified and modified by upright posture.
In any case, the shape of the soft spots and sutures of the skull are a reflection of cranial hydrodynamics, which is fluid mechanics in the brain and skull. The fluid mechanics are the result of electrical, circulatory and respiratory waves. Those waves are further amplified and modified by upright posture.Strong CSF pulsations are a sign of good circulation and health. Weak pulsations are a sign of ill health and old age. On the other hand, when they get out of hand, waves can move boulders in rivers and tear apart the most imposing shorelines and obstacles. They can also cause malformations of the skull, as well as cause the sutures to stay open, as mentioned above. The pulsations of the brain also cause the irregular wave-like shapes of the sutures. They even leave little impressions on the inside roof of the skull where special valves, called arachnoid granulations, squirt CSF into the venous drainage system of the skull called dural sinuses.
 If the pulsations can shape, indent and move the bones of the skull they can easily compress, dent and deform the brain and, in fact, they do. When the heart contracts a considerable amount of blood is driven into the brain, which compresses the brain, veins and CSF pathways. This drives venous blood and CSF out of the cranial vault and brain. When the heart relaxes, the brain, veins and CSF pathways expand which draws blood into the tissues of the brain, and pulls waste out of tissue spaces and into the drainage system ready to be removed on the next cycle. The heart thus causes the brain to rhythmically expand and contract.
If the pulsations can shape, indent and move the bones of the skull they can easily compress, dent and deform the brain and, in fact, they do. When the heart contracts a considerable amount of blood is driven into the brain, which compresses the brain, veins and CSF pathways. This drives venous blood and CSF out of the cranial vault and brain. When the heart relaxes, the brain, veins and CSF pathways expand which draws blood into the tissues of the brain, and pulls waste out of tissue spaces and into the drainage system ready to be removed on the next cycle. The heart thus causes the brain to rhythmically expand and contract.Problems occur when waves get out of control. I liken them to rogue waves and describe them in more detail on my prior post. When CSF volume gets out of control it can damage the brain. Likewise, when CSF waves get out of control they can damage the brain as well. The basal cisterns (wells) that surround the brainstem and cerebellum with CSF, are the first place to experience the brunt of rogue waves and the most likely to suffer the consequences. I suspect that chronic pounding from rogue waves can cause damage.
Rogue waves may play a role in arachnoid cysts, cystic ventricles as in Dandy-Walker syndrome and the variant of Parkinson’s called multisystem atropy or Shy-Drager. It most likely plays a role in empty sella syndrome and hormonal problems, as well as other conditions. I further suspect that one of the likely sources for destructive rogue waves in the brain comes from the cervical spine.
The first and most likely source of rogue waves is from malformations and misalignments in the upper cervical spine. Another is backjets due to whiplash, a phrase coined by Dr. Frans Schelling. Still another cause of the destructive, reflected waves is spondylosis lower down in the cervical spine.
Spondylosis is the term for degeneration of the spine. Among other things, spondylosis compresses the spinal canal and vertebral veins, which affects blood and CSF flow, as well as causing standing waves in the basal cisterns of the brain. Blockage of the vertebral veins affects blood and CSF flow in the brain. Overtime, chronic pounding from standing waves (clapotis-see prior posts) in the basal cisterns can compress the parts they surround and damage the brain. I will discuss spondylosis, seawalls and standing waves in next post.
For further information on related topics go to my website at www.upright-health.com.
Posted in Alzheimer's, ccsvi, CSF, multiple sclerosis, Parkinson's, spondylosis 1 Comment
CSF Currents, Winds and Tides
 In 1925 the famous neurosurgeon Dr. Harvey Cushing published one of his lectures in Lancet in which he described cerebrospinal fluid (CSF) as the third circulatory system of the brain. The dynamic flow of the third circulatory system of the brain and cord can be compared to a current that comes out of large lakes and rivers fed by rainfall and streams and connected by a gulf to a much larger ocean. Winds whip up the water and the currents and tides collide in the gulf, which results in waves.
In 1925 the famous neurosurgeon Dr. Harvey Cushing published one of his lectures in Lancet in which he described cerebrospinal fluid (CSF) as the third circulatory system of the brain. The dynamic flow of the third circulatory system of the brain and cord can be compared to a current that comes out of large lakes and rivers fed by rainfall and streams and connected by a gulf to a much larger ocean. Winds whip up the water and the currents and tides collide in the gulf, which results in waves.The sketch above on the right shows the Great Lakes of North America where rain water gathers from surrounding hills and streams. The water is carried by currents that flow out of the lakes by way of the Saint Lawrence River where it enters the Saint Lawrence Gulf, which is continuous with the ocean. Compared to the vast Atlantic Ocean, all the Great Lakes combined are much smaller in size and capacity.
While the current flows out of the Great Lakes to the ocean the tide of the ocean it runs into varies with the moon and time of day. Sometimes it moves out to sea in the same direction as the flow of the Saint Lawrence. Othertimes the tide comes in and flows against the river’s current. This creates conflict and turbulance where the two meet in the gulf. Over time the water turbulance caused by the ebb and flow of the tide erodes the coasts of Northern America and helps shape its shorelines.
Cerebrospinal fluid (CSF), a filtrate of blood, is basically water with some sugar and other elements mixed in. CSF is produced in the four ventricles (chambers) of the brain. From there it follows through various channels and into every nook and cranny of the brain. It also flows down through the spinal cord. For the most part, as far as we currently know, most CSF finds its way from the cord back to the brain where it eventually flows into the major veins of the brain and exits the skull by way of the internal jugular and vertebral veins.
Click on the sketch of the brain below to enlarge it. (This is a sagittal view meaning looking at one half of the brain and cord as though they were split from front to back.) In this analogy the person is lying on their side. Now look at the sketch as though it was a nautical map of many lakes and rivers with the brain and cord being the land masses. All the folds, creases, crevices and cracks you see in the brain are like large and small fiords filled with water (CSF). The coast of the brain is completely surrounded by the sea so that no surface is untouched by water (CSF). The cord is, likewise, surrounded by water. Both are further bound by large rivers, which are the dural sinuses (veins) of the brain and vertebral veins of the cord.
CSF begins its journey in the lateral ventricles (lakes) located in the center of the brain. The squiggly lines surrounding the lakes are like mountains from which water flows down through streams to fill the lakes. The arrows show the direction of the current and CSF flow in the brain and cord.
The first two lakes flow into the next lake (third ventricle) where additional water from surrounding hills enter the system. It then flows through a tight canal called an aqueduct and enters yet another lake (fourth ventricle) with a large land mass protruding into it. Again, rivers from the surrounding hills that line the coast contribute even more water but this is the last place where water enters the system.
From the last lake (the fourth ventricle) CSF flows out into a gulf called the basal cisterns of the brain. From here, in the gulf, it can flow in one of two directions. It can either flow back up to the top of the brain or it can flow down into the cord. At the bottom of the cord is a large sea called the lumbar cistern. The capacity and volume of CSF (water) in the cord and lumbar cistern, like the ocean, is far greater than the combined capacity of all the ventricles, cisterns and spaces in the brain.
The direction CSF takes when it enters the gulf of the basal cisterns depends on which way the tide is going which is determined by the gravitational pull of the earth, as well as the time of day, which will be explained below. If it gets strong enough, wind can also affect the current and flow of CSF (water) in the cisterns (gulf). It can even cause it to take alternative routes. In either case, once it leaves the (ventricles) lakes where it is produced, CSF moves through channels that don’t contribute any additional water. Those channels are depicted by spaces with stipled lines.
In the position described above (the person on their side) the tide is in and the flow of CSF in the brain and the cord is mostly upwards toward the top of the brain. When it reaches the top of the brain it empties into part of the drainage system of the brain called the venous lacunae, lacunae means lakes. The venous lacunae contain canals called arachnoid granulations that are small protrusions (villi) of the arachnoid layer (middle covering of the brain) that connect the CSF pathways to the largest vein of the brain called the superior sagittal sinus. They transfer CSF back into the blood stream through the venous drainage system.
After it leaves the stipled CSF pathways and enters the superior sagittal sinus by way of the arachnoid granulation, slightly further down you can see a white circle called a confluence. A confluence is a place where rivers meet. In this case several large veins (rivers) meet at the confluence. From here the large veins drain down into the basement of the skull called the posterior fossa and enter into either the internal jugular veins or vertebral veins.
The tide changes in this analogy when we turn the system upright. When we stand upright, the current speeds up and the tide flows away from the brain. During the night when we sleep the tide returns back toward the brain. Hanging upside down (inversion) causes a strong reversal in the tide. Straining while holding the breath, which is called a Valsalva maneuver also causes back pressure against the current and can, likewise, reverse tides. Strong tides can cause rivers to change their course in the brain and seek other outlets. In my book, The Downside of Upright Posture, I discuss giraffes, bats and whales and the forces they have to deal with. Giraffes and bats had to find ways to contend with tides caused by exceptional inversion flows from long necks and spending long periods of time hanging upside down. In giraffes it occurs when they lower their head to drink water. In bats the tides shift when they sleep. In humans tides shift when we wake up from lying down to sit or stand upright.
The first place to feel the affects of shifts in currents and tides in the brain is where they collide in the gulf of the basal cisterns. If you look closely at the picture you will see a cistern above and below the cerebellum. There are also cisterns below and in front of the cord. The cisterns in the spaces above the pons of the cord and the cerebellum surround the midbrain. Among other things the midbrain contains the cerebral aqueduct (canal for CSF flow) and the substantia nigra. The substantia nigra is where dopamine is produced and is affected in Parkinson’s disease. I suspect that increased volume and pressure in the ventricles and cisterns may play a role in Parkinson’s disease. Increased CSF volume and pressure in the ventricles and cisterns may play a role in other neurodegenerative diseases as well.
The wind in the system comes from respiration (breathing). Most times breathing merely creates ripples that help to move CSF along. Sometimes, however, it causes a great deal of back pressure, such as in a Valsalva maneuver mentioned above, which forces CSF to find alternative outlets to exit the brain in order to keep things flowing and prevent backups in the system.
 When it comes to the impact of currents, winds and tides, tide has a far greater influence on CSF flow. When large ocean tides rush into small river channels tidal bores (waves) occur. Where river currents and ocean tides collide standing waves called clapotis can occur. Tidal bores and clapotis (covered in my last blog) cause turbulance that moves depris which scour and undermine anything in its wake. Coasts are shaped by the relentless ebb and flow of daily tides. Anything that stands in its way or disrupts the ebb and flow of relentless tide and current is subject to erosion. The same thing happens in the brain.
When it comes to the impact of currents, winds and tides, tide has a far greater influence on CSF flow. When large ocean tides rush into small river channels tidal bores (waves) occur. Where river currents and ocean tides collide standing waves called clapotis can occur. Tidal bores and clapotis (covered in my last blog) cause turbulance that moves depris which scour and undermine anything in its wake. Coasts are shaped by the relentless ebb and flow of daily tides. Anything that stands in its way or disrupts the ebb and flow of relentless tide and current is subject to erosion. The same thing happens in the brain.When it comes to the brain the posterior fossa is the first area to feel the affect of tidal bores and clapotis. If the tidal waves are strong enough it can start to back up into the lakes (ventricles) and affect the structures that line their shores. The first ventricle (lake) to feel the affect is the fourth ventricle (lowest). Not surprisingly, the cisterns and ventricles are similarly affected in Dandy-Walker syndrome seen in children and a variant of Parkinson’s disease called multisystem atrophy or olivopontine cerebellar atrophy seen in adults. Both conditions are associated with enlarged cisterns and cystic (enlarged) fourth ventricles mentioned in previous posts.
Dandy-Walker sydrome is a congenital malformation of the brain originally referred to as Dandy-Walker cysts. It was named after Dr. Walter Edward Dandy and Dr. Earl Walker. The contributions of Dr. Dandy to neurosurgery and our understanding of CSF flow and hydrocephalus are legendary and far too numerous to describe here. Among other things he trained under Dr. Harvey Cushing mentioned above. The Dandy Walker cyst-like malformation is somewhat like a reverse Chiari malformation in that the posterior fossa is too large, the brainstem and cerebellum are too small and the cerebellum herniates upward into the tentorium cerebelli rather than downwards into the foramen magnum. Brain shrinkage and increased CSF volume has also been associated with Alzheimer’s disease and multiple sclerosis.
The choke point in the CSF and venous circulatory system of the brain is in the foramen magnum and upper cervical spinal canal. Degeneration (spondylosis) and misaligments of the lower cervical spine can further affect the current and flow of blood and CSF between the brain and cord. For additional information regarding the connection between the brain and cord visit our site at www.upright-health.com.
CSF, Clapotis, Cisterns and Cysts
 The picture on the right is an example of clapotis. It comes from a book called Sea Kayak by Gordon Brown who teaches classes in Scotland where sea and surf are notoriously rough. White water and open sea kayakers are attracted to waves and love to study all their subtleties.
The picture on the right is an example of clapotis. It comes from a book called Sea Kayak by Gordon Brown who teaches classes in Scotland where sea and surf are notoriously rough. White water and open sea kayakers are attracted to waves and love to study all their subtleties.Clapotis is a nautical term for standing waves. It is French for lapping of water. According to English translators it is pronounced as clap-o-tee, like a long sounding “o”, as in toe. According to my Canadian French connection, it is pronouned more like clap-ah-tee, similar to the short sound of ”o” as in copper. In either case, in French, the “s”, at the end of the word indicates that it is plural, meaning more than one wave, but it is silent.
Clapotis occur when waves clap together such as incoming ocean waves running into waves that have bounced off of objects such as rocky coasts or manmade seawalls. Clapotis can be explosive and sometimes roar from the rush of the water. Like the sound of the “s” on the end, sometimes they can be silent and gentle swells like those that occur between the land masses of a mainland and its barrier islands. The ocean waves are calmer but still reflect between these land masses.
As all sea faring people well know, however, silent or not, standing waves can be deceptive, destructive and even deadly. On the bottom side they scour and tear at the footers of manmade seawalls. They similarly severely undermine and damage coasts. On the top side they can toss and turn ships about like toys in a tub.
Rogue waves are a type of standing wave. They are also known as freak or killer waves because they suddenly spring up seemingly out of nowhere and significantly increase the height and strength of a wave. They often travel against prevailing winds and currents and are sometimes preceded by deep troughs that look like a hole in the ocean. Killer waves can run aground, wreck, roll and swallow unsuspecting ships, sometimes in a matter of minutes and sometimes only seconds. For centuries scientists scoffed at sailors and claimed the sailors were spinning tall tales from too much time spent isolated at sea. New evidence, however, has rocked their boat. Sailors were right, these waves do exist. As yet, we know very little about them or what stirs them up. What we do know is that fluids basically follow pressure gradients and the path of least resistance.
In physics, clapotis are considered to be transverse waves because they can rise up. In other words, they travel up and down in a two dimensional plane. Consequently, clapotis cannot occur in rigid containers, such as water pipes in homes, because rigid containers can’t expand and allow the wave to rise. Instead rigid containers cause longitudinal waves. Longitudinal waves are caused by alternating compression and expansion of fluids or air within a confined space. For example, longitudinal waves occur in muscial instruments that use pipes to make sound. In contrast to transverse waves, longitudinal waves travel in one plane.
Unlike standing waves, water hammers occur in rigid containers, such as pipes, when a forceful stream of moving water is suddenly stopped. The rapid change in velocity causes a collision similar to a standing wave but the outcome is different. Because the wave cannot increase in height it causes compression (a longitudinal movement), which increases pressure that travels back through the pipes. The stiff pipes absorb the energy, which causes them to shake along their course. Unlike the “s” at the end of clapotis, water hammers are not silent. They make a loud banging noise like someone hammering on the plumbing. Over time, water hammers can break pipe joints.
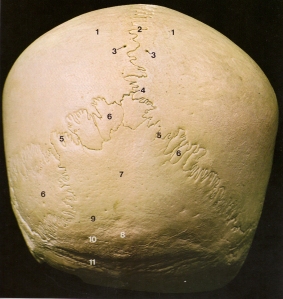 When it comes to standing waves and water hammers, the latest research is starting to connect faulty cerebrospinal fluid (CSF) flow with the cause of neurodegenerative diseases such as Alzheimer’s, Parkinson’s and multiple scleriosis, which is the subject of my book, “The Downside of Upright Posture”. I started looking into the role of CSF in neurodegenerative diseases about thirty years ago because of my background in upper cervical chiropractic and craniopathy, which led me to the subject of physical anthropology.
When it comes to standing waves and water hammers, the latest research is starting to connect faulty cerebrospinal fluid (CSF) flow with the cause of neurodegenerative diseases such as Alzheimer’s, Parkinson’s and multiple scleriosis, which is the subject of my book, “The Downside of Upright Posture”. I started looking into the role of CSF in neurodegenerative diseases about thirty years ago because of my background in upper cervical chiropractic and craniopathy, which led me to the subject of physical anthropology.Upper cervical chiropractic taught me the importance of the upper cervical spine and base of the skull to human health. Craniopathy taught me about the design of the human skull and the movement of cerebrospinal fluid through the brain and cord. Because of craniopathy, I also became interested in the base and sutures of the skull. In particular, I became interested in the sutures that unite the membranous bones of the skull that form the cover over the cranial vault, which contains the brain.
The picture above on the left shows the sutures at the back and bottom of the skull. Like all bones, the sutures are a reflexion of the mechanical stresses that strained and shaped them. Early anatomists called them sutures because they thought they looked somewhat similar to surgical stitches. But to me they look more like waves and they are shaped that way for a reason. They are similar to a seismic recording of pressure fluctuations and movement in the skull and cranial vault. The pressure fluctuations come from a combination of neurological (electrical), circulatory and respiratory waves. Upright posture and bipedal walking further amplify those waves.
 CSF is a watery fluid produced in cavities of the brain called ventricles. CSF flows out of the ventricles and into the cisterns and subarachnoid spaces of the brain and spinal cord. The role of CSF is to cushion, protect and support the brain to prevent it from sinking inside the cranial vault. It also carries waste out of the brain.
CSF is a watery fluid produced in cavities of the brain called ventricles. CSF flows out of the ventricles and into the cisterns and subarachnoid spaces of the brain and spinal cord. The role of CSF is to cushion, protect and support the brain to prevent it from sinking inside the cranial vault. It also carries waste out of the brain.CSF is under constant fluctuating hydraulic pressures due to the pumping of the heart which increases arterial pressure in the brain when it contracts. Likewise, breathing causes changes in pressure inside the ribcage. During exhalation pressure inside the ribcage increases. Among other things this increases venous pressure which is transmitted to the vertebral veins. The vertebral veins are connected to the dural sinuses of the brain and like the dural sinuses, have no valves to prevent inversion (reverse) flows. Consequently, respiratory pressure changes are transmitted to the brain and exhalation increases intracranial pressure.
Because the cranial vault is a closed container, the increase in blood volume and intracranial pressure needs to be controlled. When things are working properly, any excess CSF volume and pressure is typically vented out of the cranial vault via the foramen magnum and down into the subarachnoid space of the spinal canal. Inherited (genetic) and acquired (aging and injuries) structural problems in the cervical spine can cause back pressure against the venting mechanism. If outgoing CSF waves meet resistance or inversion flows of blood and CSF waves coming up from the vertebral veins and subarachnoid space (contains CSF) in the spinal canal then clapotis (standing waves) or water hammers can occur.
In the sketch above on the right, the brain is like a landmass inside the cranial vault surrounded by a sea of CSF and venous blood in vessels with no valves to prevent inversion flows. The skull is a fairly rigid container. Consequently, the amplitude of any standing waves (clapotis) in the brain is limited. Thus the standing wave that occurs as CSF in the brain claps into CSF in the cord as it attempts to flow through the foramen magnum and out of the cranial vault becomes more like a water hammer.
In either case, the first areas of the brain to receive the brunt of either clapotis or water hammers are the basal cisterns that surround the cerebellum and brainstem. It is possible that over time, chronic clapotis (standing waves) or constant banging from water hammers in the basal cisterns weaken and eventually erode the soft tissues of the brain the same as rocky coasts.
Similarly, I suspect that standing waves and water hammers may also play a role in the formation of arachnoid cysts and empty sella syndromes, as well as the Dandy-Walker and Shy-Drager syndrome (a variant of Parkinson’s disease) type cysts seen in the ventricles and cisterns.
For a better understanding of the big picture read my book. For further information visit my website at www.upright-health.com.
Posted in Alzheimer's, arachnoid cysts, chiari malformations, CSF, Dandy-Walker syndrome, dementia, demyelination, Devic's disease, Ehlers Danlos Syndrome, empty sella syndrome, ms lesions, multiple sclerosis, neuromyelitis optica, optic neuritis, optic spinal multiple sclerosis, Parkinson's, physical anthropology, spondylosis, syrinxes Leave a comment
The Missed Measure of Man
The missed measure of man was overlooked during earlier investigations of human cranial capacity that focused on its relationship to intelligence. That is what the book to the right set about to disprove. Unfortunately, the subject of cranial capacity due to it’s ties to human intelligence has since become taboo to discuss due to political correctness. This is unfortunate because cranial capacity may play a key role in neurodegenerative diseases such as Alzheimer’s, Parkinson’s and multiple sclerosis and has nothing to do with intelligence. The missed measure of man that was overlooked is the design, layout and capacity of the posterior fossa in particular.
Some scientists once believed that there was a direct correlation between cranial capacity and human intelligence. It is a myth I cover in the last chapter in my book. The first problem is that there is no direct linear correlation between brain size and intelligence. If there were then elephants and whales would be smarter than humans. Similarly speaking, parrots have small cranial capacities but are far more intelligent (due to the way we test intelligence) than many mammals with much larger brains. Furthermore, regardless of race, females tend to have a smaller cranial capacity compared to males and Einstein, who was considered by many to be a genius, had an exceptionally small cranial capacity. In fact, his cranium was at the very low end of female capacity.
There is another problem and that is the way we measure intelligence. The brain is a survival organism. It’s job it to help us manipulate and master our environment. IQ tests are prejudiced against indigenous people who must master and remember many things about their environment and rely on ingenuity to survive and thrive. IQ tests fail to measure the subtleties and full spectrum of human intellect such as creativty, imagination and intuition among other things. Instead, modern IQ tests measure abstractions and memory in ways that may be important to people living in industrialized socities but are useless to indigenous people. Many people with so called high IQ’s wouldn’t be able to survive in similar circumstances. The bottom line is that the correlation between IQ and cranial capacity doesn’t work.
Presumably there are about one hundred billion nerves cells in the brain. Interestingly, the cerebellum sits in the posterior fossa and has more nerves that the rest of the brain put together. The truth is no one has actually counted. It is simply a guess based on average brain weight, the amount of fat and other factors. The average brain in humans weighs 1300-1400 grams or about 2.75-3.5 pounds. About half of it is fat. The rest of it is nerve cells. As far as we know for now, until proven otherwise, all humans are born with roughly the same number of nerve cells in the brain give or take a few billion or so. Bigger heads simply have bigger brains with larger nerves and more fat, not necessarily more nerves.
Nonetheless, a great deal of time and energy was wasted at the time measuring the size of the head and the capacity of the cranial vault. The famous book by Jay Gould pictured above was published in 1984 called The Mismeasure of Man. In it Gould refutes the arguements of the day, some of which were racially motivated.
Disregarding the old ignorant debates about cranial capacity and intelligence, there are many important issues to consider when it comes to race, gender and health. Just as females and males have different health concerns, certain health conditions have a higher incidence in particular races and ethnic groups. For example, thalasemia and sickle cells affect Asians and Africans far more than northern Europeans. Europeans living on the Mediterranean, however, are likewise effected. Thalasemia and sickle cell anemia are believed to have been protective mechanisms against malaria. The downside is they predispose afflicted people to anemia. Just as blood cells affect our physiology so does the design of the skull.
It is easy to see racial differences, including mixed races, simply by looking at the face. In this regard, it is interesting to note that the design of the facial part of the skull is intimately connected to the design of the base of the skull. They grow together during development and have a strong influence on one another. Their growth in childhood follows the musculoskeletal system of the rest of the body.
Together, the face and base of the skull determine the basic layout of the floor of the cranial vault. The bones that form the curved walls and cap the top of the cranial vault follow the growth of the brain. The cover over the cranial vault stops growing early in life when the brain stops growing in size.
 There are significant racial and gender differences in the incidence of multiple sclerosis. There are also geographic differences but that’s a different story. When it comes to race, people of Asian and African descent appear to have a distinct advantage in that they appear to have a much lower incidence of MS than European people. When it comes to gender, regardless of race, females appear to have a distinct disadvantage in that they have a significantly higher incidence of MS compared to males. The difference in incidence in both race and gender may be due to design diffferences in the posterior fossa.
There are significant racial and gender differences in the incidence of multiple sclerosis. There are also geographic differences but that’s a different story. When it comes to race, people of Asian and African descent appear to have a distinct advantage in that they appear to have a much lower incidence of MS than European people. When it comes to gender, regardless of race, females appear to have a distinct disadvantage in that they have a significantly higher incidence of MS compared to males. The difference in incidence in both race and gender may be due to design diffferences in the posterior fossa.
The white lines in the brain scan above represent the outline of the posterior fossa. The top line is missing because it represents the opening in the covering over the posterior fossa. The covering is called the tentorium cerebelli. The opening is called the tentorial notch or incisura. The scan is from a paper called, “Dimensions of the posterior fossa in patients symptomatic for Chiari 1 malformation but without cerebellar tonsillar descent,” by Sekula et. al., published in Fluids and Barriers of the CNS in 2005.
Among other things, a smaller or hypoplastic posterior fossa is more susceptible to Chiari malformations. In this regard, females most likely have a smaller posterior fossa compared to most males. They also have a higher incidence of multiple sclerosis compared to males.
Up until the eighth decade, they also have a higher incidence and get Alzheimer’s sooner than males. Females are also far more susceptible to Chiari malformations and to Dandy-Walker syndrome. Dandy-Walker syndrome, as you may recall, is related to enlarged ventricles and cysts that effect CSF flow mentioned in the previous post. The increased incidence of these particular conditions in females may have to do with the design of the posterior fossa, especially its capacity.
When it comes to race, a fairly recent orthodontic study on racial differences in craniofacial design done in Scotland showed that Europeans tend to have a shorter clivus in the base of the skull. This is interesting because a shorter clivus could decrease the capacity of the posterior fossa in Europeans compared to Asian and African designs. Thus, if the old arguments regarding a correlation between cranial capacity and IQ were true, then European brains would have fewer nerves compared to Asian and African brains. In addition to the capacity of the posterior fossa, other design issues to consider are the angles and pitch of the clivus and the tentorium cerebelli, as well as the angle of the base of the skull to the upper cervical spine.
Another issue to consider is, although they don’t get classic MS, Asians and Africans do get optic spinal multiple sclerosis and Devic’s disease. What’s more, Devic’s tends to be relatively more severe and disabling. Both optic spinal multiple sclerosis and Devic’s may be variants of multiple sclerosis due to design differences in the posterior fossa. The problem may lie in our method of diagnosing MS, which is based on classic lesions. Apparently, Asian and African people don’t get classic lesions. Aside from that, they otherwise get similar signs and symptoms. Consequently, many cases of MS among African and and Asian races may have been and continue to be overlooked and marginalized.
In addition, the condition of hydrocephalus is as old as the human race. It started with standing upright. All races are equally susceptible. Lastly, as we continue to learn more from upright MRI, just as I predicted in my book, it appears Chiari malformations also referred to as cerebellar tonsillar ectopia (CTE) are far more common than once thought. They can occur later in life due to trauma, aging and misalignments of the upper cervical spine that cause the brainstem to get pulled down or to sag slightly, due to low pressure, toward the base of the skull and into the foramen magnum. Tethered cords from a genetically short cord or from degeneration and abnormal curvatures of the spine can also cause CTE. Humans are susceptible to CTE by design and CTE can cause hydrocephalic-like conditions. Furthermore, hydrocephalic conditions and CTE may be at the core and cause of many neurodegenerative diseases. One of the causes lies in the design, layout and capcity of the posterior fossa. Other causes will be discussed as my blog and website continue to grow. For further information visit my website at www.upright-health.com.
Some scientists once believed that there was a direct correlation between cranial capacity and human intelligence. It is a myth I cover in the last chapter in my book. The first problem is that there is no direct linear correlation between brain size and intelligence. If there were then elephants and whales would be smarter than humans. Similarly speaking, parrots have small cranial capacities but are far more intelligent (due to the way we test intelligence) than many mammals with much larger brains. Furthermore, regardless of race, females tend to have a smaller cranial capacity compared to males and Einstein, who was considered by many to be a genius, had an exceptionally small cranial capacity. In fact, his cranium was at the very low end of female capacity.
There is another problem and that is the way we measure intelligence. The brain is a survival organism. It’s job it to help us manipulate and master our environment. IQ tests are prejudiced against indigenous people who must master and remember many things about their environment and rely on ingenuity to survive and thrive. IQ tests fail to measure the subtleties and full spectrum of human intellect such as creativty, imagination and intuition among other things. Instead, modern IQ tests measure abstractions and memory in ways that may be important to people living in industrialized socities but are useless to indigenous people. Many people with so called high IQ’s wouldn’t be able to survive in similar circumstances. The bottom line is that the correlation between IQ and cranial capacity doesn’t work.
Presumably there are about one hundred billion nerves cells in the brain. Interestingly, the cerebellum sits in the posterior fossa and has more nerves that the rest of the brain put together. The truth is no one has actually counted. It is simply a guess based on average brain weight, the amount of fat and other factors. The average brain in humans weighs 1300-1400 grams or about 2.75-3.5 pounds. About half of it is fat. The rest of it is nerve cells. As far as we know for now, until proven otherwise, all humans are born with roughly the same number of nerve cells in the brain give or take a few billion or so. Bigger heads simply have bigger brains with larger nerves and more fat, not necessarily more nerves.
Nonetheless, a great deal of time and energy was wasted at the time measuring the size of the head and the capacity of the cranial vault. The famous book by Jay Gould pictured above was published in 1984 called The Mismeasure of Man. In it Gould refutes the arguements of the day, some of which were racially motivated.
Disregarding the old ignorant debates about cranial capacity and intelligence, there are many important issues to consider when it comes to race, gender and health. Just as females and males have different health concerns, certain health conditions have a higher incidence in particular races and ethnic groups. For example, thalasemia and sickle cells affect Asians and Africans far more than northern Europeans. Europeans living on the Mediterranean, however, are likewise effected. Thalasemia and sickle cell anemia are believed to have been protective mechanisms against malaria. The downside is they predispose afflicted people to anemia. Just as blood cells affect our physiology so does the design of the skull.
It is easy to see racial differences, including mixed races, simply by looking at the face. In this regard, it is interesting to note that the design of the facial part of the skull is intimately connected to the design of the base of the skull. They grow together during development and have a strong influence on one another. Their growth in childhood follows the musculoskeletal system of the rest of the body.
Together, the face and base of the skull determine the basic layout of the floor of the cranial vault. The bones that form the curved walls and cap the top of the cranial vault follow the growth of the brain. The cover over the cranial vault stops growing early in life when the brain stops growing in size.
 There are significant racial and gender differences in the incidence of multiple sclerosis. There are also geographic differences but that’s a different story. When it comes to race, people of Asian and African descent appear to have a distinct advantage in that they appear to have a much lower incidence of MS than European people. When it comes to gender, regardless of race, females appear to have a distinct disadvantage in that they have a significantly higher incidence of MS compared to males. The difference in incidence in both race and gender may be due to design diffferences in the posterior fossa.
There are significant racial and gender differences in the incidence of multiple sclerosis. There are also geographic differences but that’s a different story. When it comes to race, people of Asian and African descent appear to have a distinct advantage in that they appear to have a much lower incidence of MS than European people. When it comes to gender, regardless of race, females appear to have a distinct disadvantage in that they have a significantly higher incidence of MS compared to males. The difference in incidence in both race and gender may be due to design diffferences in the posterior fossa.The white lines in the brain scan above represent the outline of the posterior fossa. The top line is missing because it represents the opening in the covering over the posterior fossa. The covering is called the tentorium cerebelli. The opening is called the tentorial notch or incisura. The scan is from a paper called, “Dimensions of the posterior fossa in patients symptomatic for Chiari 1 malformation but without cerebellar tonsillar descent,” by Sekula et. al., published in Fluids and Barriers of the CNS in 2005.
Among other things, a smaller or hypoplastic posterior fossa is more susceptible to Chiari malformations. In this regard, females most likely have a smaller posterior fossa compared to most males. They also have a higher incidence of multiple sclerosis compared to males.
Up until the eighth decade, they also have a higher incidence and get Alzheimer’s sooner than males. Females are also far more susceptible to Chiari malformations and to Dandy-Walker syndrome. Dandy-Walker syndrome, as you may recall, is related to enlarged ventricles and cysts that effect CSF flow mentioned in the previous post. The increased incidence of these particular conditions in females may have to do with the design of the posterior fossa, especially its capacity.
When it comes to race, a fairly recent orthodontic study on racial differences in craniofacial design done in Scotland showed that Europeans tend to have a shorter clivus in the base of the skull. This is interesting because a shorter clivus could decrease the capacity of the posterior fossa in Europeans compared to Asian and African designs. Thus, if the old arguments regarding a correlation between cranial capacity and IQ were true, then European brains would have fewer nerves compared to Asian and African brains. In addition to the capacity of the posterior fossa, other design issues to consider are the angles and pitch of the clivus and the tentorium cerebelli, as well as the angle of the base of the skull to the upper cervical spine.
Another issue to consider is, although they don’t get classic MS, Asians and Africans do get optic spinal multiple sclerosis and Devic’s disease. What’s more, Devic’s tends to be relatively more severe and disabling. Both optic spinal multiple sclerosis and Devic’s may be variants of multiple sclerosis due to design differences in the posterior fossa. The problem may lie in our method of diagnosing MS, which is based on classic lesions. Apparently, Asian and African people don’t get classic lesions. Aside from that, they otherwise get similar signs and symptoms. Consequently, many cases of MS among African and and Asian races may have been and continue to be overlooked and marginalized.
In addition, the condition of hydrocephalus is as old as the human race. It started with standing upright. All races are equally susceptible. Lastly, as we continue to learn more from upright MRI, just as I predicted in my book, it appears Chiari malformations also referred to as cerebellar tonsillar ectopia (CTE) are far more common than once thought. They can occur later in life due to trauma, aging and misalignments of the upper cervical spine that cause the brainstem to get pulled down or to sag slightly, due to low pressure, toward the base of the skull and into the foramen magnum. Tethered cords from a genetically short cord or from degeneration and abnormal curvatures of the spine can also cause CTE. Humans are susceptible to CTE by design and CTE can cause hydrocephalic-like conditions. Furthermore, hydrocephalic conditions and CTE may be at the core and cause of many neurodegenerative diseases. One of the causes lies in the design, layout and capcity of the posterior fossa. Other causes will be discussed as my blog and website continue to grow. For further information visit my website at www.upright-health.com.
Posted in Alzheimer's, arachnoid cysts, chiari malformations, cranial capacity, CSF, Dandy-Walker syndrome, dementia, Devic's disease, human intellect, measure intelligence, multiple sclerosis, neuromyelitis optica, optic neuritis, optic spinal multiple sclerosis, Parkinson's, physical anthropology 5 Comments
Cysts, Syrinxes and CSF
Cavities such as cysts and syrinxes that may or may not contain cerebrospinal fluid (CSF) are seen in the brain and cord. In this post we are concerned with the types that contain CSF. Faulty fluid mechanics in the brain and cord can cause these types of cavities to form. Likewise, cysts and syrinxes can cause faulty fluid mechanics in the brain and cord.
Cysts sometimes develop in the middle layer of the three protective coverings of the brain and cord, called meninges. If you look at the picture below, toward the bottom on the right hand side, there is a label pointing to a dark line called dura mater. The dura mater is the tough outer covering that surrounds the brain and cord. Above the dura mater is another label, called the arachnoidea, which points to a white line surrounding the brain and cord. The arachnoid mater is the middle layer of the meninges. Still another label above that points to a black line called the pia mater, which is the inner most layer of the covering of the brain and cord. The subarachnoid space is the stipled area that lies between the arachnoid and pia mater.
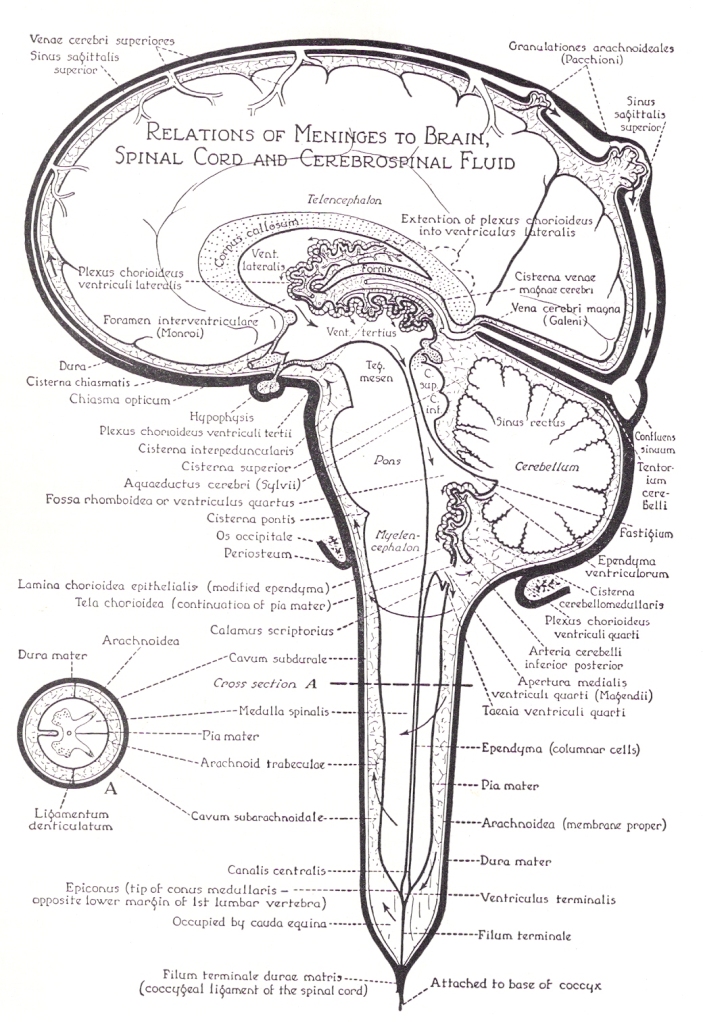 Arachnoid cysts are fairly common. They project out from the arachnoid mater covering and subarachnoid space. They are also called leptomeningeal cysts. Arachnoid cysts tend to occur in certain places in the brain and cord. One of the common areas is the middle fossa of the cranial vault, as well as the Sylvian fissure of the brain which is located in the middle fossa. The Sylvian fissure is a deep fold which separates the frontal, temporal and parietal lobes of the brain.
Arachnoid cysts are fairly common. They project out from the arachnoid mater covering and subarachnoid space. They are also called leptomeningeal cysts. Arachnoid cysts tend to occur in certain places in the brain and cord. One of the common areas is the middle fossa of the cranial vault, as well as the Sylvian fissure of the brain which is located in the middle fossa. The Sylvian fissure is a deep fold which separates the frontal, temporal and parietal lobes of the brain.
Other common areas for arachnoid cysts are, within the covering over the posterior fossa called the tentorium cerebelli (the black line over top of cerebellum), the cisterna magna (the stipled area beneath the cerebellum), which is a cistern located between the cerebellum and the medulla oblongata, and the suprasellar region, which is a cavity in a bone in the skull that houses the pituitary gland (the hypophysis hanging down beneath the front of the brain).
If you look at the middle of the brain in the picture above, the arrows start in the lateral ventricles and flow down through the third ventricle, the cerebral aqueduct, and into the fourth ventricle. They then leave the fourth ventricle and enter the stipled area which represents the subarachnoid space.
Enlarged ventricles are typically referred to as ventriculomegaly. Enlargement of the fourth ventricle, however, is sometimes classified as a cyst or cystic ventricle. A well known example of a cystic fourth ventricle is seen in Dandy-Walker syndrome which occurs in children.
Some cysts are acquired later in life, such as from trauma. Trauma can cause cysts due to tears in the meninges. It is currently maintained, however, that most people are born with arachnoid cysts. Some are caused by genetic weakness in the tissues or design flaws in the subarachnoid space. I suspect that still others may occur due to intrauterine positions of the fetus during pregnancy that can potentially increase pressure in critical areas of the brain and cord.
Some cysts are formed in the cord and are called syrinxes from the Greek word tube. If you look at the picture above you will see a canal going down through the center of the cord. The label that points to it on the left near the bottom of the canal is the canalis centralis, which means central canal of the cord. Syrinxes typically start and are found in the central canal but they can spread outwards and affect other parts of the cord.
Syrinxes are typically expansions in the central canal of the cord. The central canal is connected to the lowest ventricle in the brain, which is the fourth. These syrinxes are also referred to as syringomyelia. Similar to cysts, syrinxes are sometimes connected to and sometimes more isolated from CSF pathways, which can trap fluids.
Sometimes the cysts and syrinxes communicate with normal CSF pathways. In the case of subarachnoid cysts the fluid can flow more freely between the cyst and subarachnoid space. In other cases, the cyst is more isolated by connective tissues so that fluids that manage to find there way into the space, find it hard to get out.
Cysts and syrinxes are sometimes associated with significant pressure that causes fluids to eject forcefully when penetrated surgically. The force from the hydraulic nature of cysts and syrinxes can consequently compress nearby tissues. The turbulant flow and subsequent pounding they create can also erode nearby tissues like waves beating on rocky cliffs on a shoreline. Turbulant flow can, likewise, erode bone. In the skull it leaves impressions that look like little dents on the inside roof of the cranial vault. Researchers now suspect that the turbulant CSF flow caused by Chiari malformations may play a role in the formation of syrinxes in the central canal of the cord.
Chiari malformations obstruct CSF flow through the foramen magnum of the skull and the upper cervical spine, which can cause normal pressure hydrocephalus (NPH) in adults. Lastly, Chiari malformations and NPH have been associated with multiple sclerosis and other neurodegenerative conditions.
Cysts and syrinxes speak volumes about CSF and the hydraulic stress it causes in the brain and cord. What’s more, obstruction of CSF flow through the foramen magnum and upper cervical spine and the faulty fluid mechanics and hydraulic stresses it creates may be one of the root causes of Alzheimer’s, Parkinson’s and multiple sclerosis, as well as other neurodegenerative diseases. Ventriculomegaly (enlargement of a ventricle) has been associated with all three of these conditions. Two variants of Parkinson’s disease are also associated with cystic conditions within the ventricles and cisterns. In most cases, the cause of cysts and syrinxes is unknown.
I will be covering more on cysts and syrinxes on this blog and my website in future posts. For now, for further information click on syringomyelia above or visit my website at www.upright-health.com.
Cysts sometimes develop in the middle layer of the three protective coverings of the brain and cord, called meninges. If you look at the picture below, toward the bottom on the right hand side, there is a label pointing to a dark line called dura mater. The dura mater is the tough outer covering that surrounds the brain and cord. Above the dura mater is another label, called the arachnoidea, which points to a white line surrounding the brain and cord. The arachnoid mater is the middle layer of the meninges. Still another label above that points to a black line called the pia mater, which is the inner most layer of the covering of the brain and cord. The subarachnoid space is the stipled area that lies between the arachnoid and pia mater.
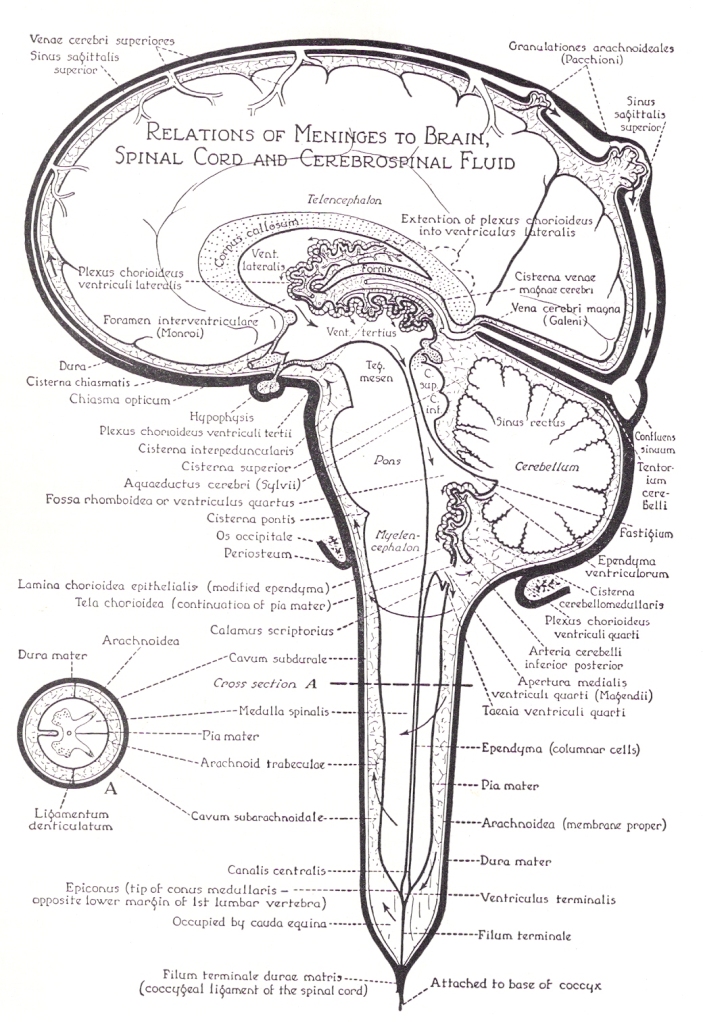 Arachnoid cysts are fairly common. They project out from the arachnoid mater covering and subarachnoid space. They are also called leptomeningeal cysts. Arachnoid cysts tend to occur in certain places in the brain and cord. One of the common areas is the middle fossa of the cranial vault, as well as the Sylvian fissure of the brain which is located in the middle fossa. The Sylvian fissure is a deep fold which separates the frontal, temporal and parietal lobes of the brain.
Arachnoid cysts are fairly common. They project out from the arachnoid mater covering and subarachnoid space. They are also called leptomeningeal cysts. Arachnoid cysts tend to occur in certain places in the brain and cord. One of the common areas is the middle fossa of the cranial vault, as well as the Sylvian fissure of the brain which is located in the middle fossa. The Sylvian fissure is a deep fold which separates the frontal, temporal and parietal lobes of the brain.Other common areas for arachnoid cysts are, within the covering over the posterior fossa called the tentorium cerebelli (the black line over top of cerebellum), the cisterna magna (the stipled area beneath the cerebellum), which is a cistern located between the cerebellum and the medulla oblongata, and the suprasellar region, which is a cavity in a bone in the skull that houses the pituitary gland (the hypophysis hanging down beneath the front of the brain).
If you look at the middle of the brain in the picture above, the arrows start in the lateral ventricles and flow down through the third ventricle, the cerebral aqueduct, and into the fourth ventricle. They then leave the fourth ventricle and enter the stipled area which represents the subarachnoid space.
Enlarged ventricles are typically referred to as ventriculomegaly. Enlargement of the fourth ventricle, however, is sometimes classified as a cyst or cystic ventricle. A well known example of a cystic fourth ventricle is seen in Dandy-Walker syndrome which occurs in children.
Some cysts are acquired later in life, such as from trauma. Trauma can cause cysts due to tears in the meninges. It is currently maintained, however, that most people are born with arachnoid cysts. Some are caused by genetic weakness in the tissues or design flaws in the subarachnoid space. I suspect that still others may occur due to intrauterine positions of the fetus during pregnancy that can potentially increase pressure in critical areas of the brain and cord.
Some cysts are formed in the cord and are called syrinxes from the Greek word tube. If you look at the picture above you will see a canal going down through the center of the cord. The label that points to it on the left near the bottom of the canal is the canalis centralis, which means central canal of the cord. Syrinxes typically start and are found in the central canal but they can spread outwards and affect other parts of the cord.
Syrinxes are typically expansions in the central canal of the cord. The central canal is connected to the lowest ventricle in the brain, which is the fourth. These syrinxes are also referred to as syringomyelia. Similar to cysts, syrinxes are sometimes connected to and sometimes more isolated from CSF pathways, which can trap fluids.
Sometimes the cysts and syrinxes communicate with normal CSF pathways. In the case of subarachnoid cysts the fluid can flow more freely between the cyst and subarachnoid space. In other cases, the cyst is more isolated by connective tissues so that fluids that manage to find there way into the space, find it hard to get out.
Cysts and syrinxes are sometimes associated with significant pressure that causes fluids to eject forcefully when penetrated surgically. The force from the hydraulic nature of cysts and syrinxes can consequently compress nearby tissues. The turbulant flow and subsequent pounding they create can also erode nearby tissues like waves beating on rocky cliffs on a shoreline. Turbulant flow can, likewise, erode bone. In the skull it leaves impressions that look like little dents on the inside roof of the cranial vault. Researchers now suspect that the turbulant CSF flow caused by Chiari malformations may play a role in the formation of syrinxes in the central canal of the cord.
Chiari malformations obstruct CSF flow through the foramen magnum of the skull and the upper cervical spine, which can cause normal pressure hydrocephalus (NPH) in adults. Lastly, Chiari malformations and NPH have been associated with multiple sclerosis and other neurodegenerative conditions.
Cysts and syrinxes speak volumes about CSF and the hydraulic stress it causes in the brain and cord. What’s more, obstruction of CSF flow through the foramen magnum and upper cervical spine and the faulty fluid mechanics and hydraulic stresses it creates may be one of the root causes of Alzheimer’s, Parkinson’s and multiple sclerosis, as well as other neurodegenerative diseases. Ventriculomegaly (enlargement of a ventricle) has been associated with all three of these conditions. Two variants of Parkinson’s disease are also associated with cystic conditions within the ventricles and cisterns. In most cases, the cause of cysts and syrinxes is unknown.
I will be covering more on cysts and syrinxes on this blog and my website in future posts. For now, for further information click on syringomyelia above or visit my website at www.upright-health.com.
Kyphosis, Stenosis and Multiple Sclerosis
 The spine has four curves. Two of them curve forward toward the belly side of the body. They are the cervical (neck) and lumbar (low back) spines. The other two arch backward toward the back and buttocks. They are the thoracic spine which supports the ribcage, and the sacrum which sits in the back of the pelvis beneath the low back. It is the pedestal the spine rests on and, similar to the thoracic spine, bends backward to support a load.
The spine has four curves. Two of them curve forward toward the belly side of the body. They are the cervical (neck) and lumbar (low back) spines. The other two arch backward toward the back and buttocks. They are the thoracic spine which supports the ribcage, and the sacrum which sits in the back of the pelvis beneath the low back. It is the pedestal the spine rests on and, similar to the thoracic spine, bends backward to support a load.
The term kyphosis refers to the normal curves of the thoracic spine and sacrum. It also refers to an exaggeration of the thoracic curve that causes a pronounced hump or backward bend in the upper back called a Gibbus deformity that pitches the shoulders and neck forward of the normal gravity line. Exaggerated kyphosis also causes a loss in height. In severe cases it can interfere with breathing as it alters the rib cage which contains the lungs and heart. Exaggerated kyphosis is sometimes referred to as hyperkyphosis.
 The term kyphosis can also be used to describe an abnormal curve of the spine that goes in the opposite or wrong direction. For example, it can be used to describe a reversal of the curve in the low back. More commonly, it is used to describe a reversal of the normal curvature in the cervical spine, which is the neck. The x-ray on the right is a good example of a kyphotic (backwards) curve in the cervical spine. Kyphosis occurring in any area of the spine can be inherited as a developmental design problem or it can be acquired later in life through trauma, aging and diseases such as arthritis, osteoporosis, compression fractures and Parkinson’s disease.
The term kyphosis can also be used to describe an abnormal curve of the spine that goes in the opposite or wrong direction. For example, it can be used to describe a reversal of the curve in the low back. More commonly, it is used to describe a reversal of the normal curvature in the cervical spine, which is the neck. The x-ray on the right is a good example of a kyphotic (backwards) curve in the cervical spine. Kyphosis occurring in any area of the spine can be inherited as a developmental design problem or it can be acquired later in life through trauma, aging and diseases such as arthritis, osteoporosis, compression fractures and Parkinson’s disease.Scoliosis is an abnormal lateral (sidewards) curve of the spine. Scoliosis is sometimes associated with kyphosis and is referred to as kyphoscoliosis. Scoliosis is typically a problem that becomes apparent in childhood. It affects females far more than males. Adults, however, can acquire scoliosis later in life due to trauma, degenerative conditions of the spine, inherited and acquired connective tissue disorders and other causes.
Scoliosis has been shown to cause functional stenosis of the spinal canal and subsequent compression of the vertebral veins which decreases venous blood flow. The problem occurs as the veins get compressed against the inside curvature of the spinal canal. Kyphosis most likely causes functional stenosis of the spinal canal and vertebral veins similar to scoliosis.
The images below are used with permission from a member of the TiMS website who underwent testing for chronic cerebrospinal venous insufficiency (CCSVI). The patient was found to have impingement of both internal jugular veins which was corrected by the placement of stents. Subsequent to placement of the stents the patient had considerable improvement in signs and symptoms.
 The image is composed of three different views superimposed on one screen. The view to the left is a plain view x-ray of the upper back and neck. If you look closely at the spinous processes (they look like teardrops that go down the middle of the spine) you will see that they deviate to the left side of the spine. Likewise, if you follow the contour of the sides of the spine you will see that the spine is curved to the left. Since the x-rays were taken from front to back the left side of the film is the right side of the patient.
The image is composed of three different views superimposed on one screen. The view to the left is a plain view x-ray of the upper back and neck. If you look closely at the spinous processes (they look like teardrops that go down the middle of the spine) you will see that they deviate to the left side of the spine. Likewise, if you follow the contour of the sides of the spine you will see that the spine is curved to the left. Since the x-rays were taken from front to back the left side of the film is the right side of the patient.The middle image is a venogram which is an MRI with contrast dye injected into the veins. In this case, the red arrow points to an area of impingement or stenosis of the internal jugular veins just in front of the upper cervical spine. The impingement decreases blood flow through the internal jugular veins, which can back up in the brain.
The image on the right is an x-ray of the stents that were inserted using interventional radiology. More often, most physicians doing the procedure use venoplasty in which a balloon is inserted into the vein and then filled to stretch the vein and open it up. Venoplasty is subject to restenosis. Stents are tubes placed in the veins that spring outward to keep the veins open. Stents are more durable and less likely to re-stenose but pose more problems due to clots. In cases such as the one above it is a tough choice, but if the structural problem causing the impingement is permanent then durability may become more of a factor to consider in choosing procedures.
If you look closely at the above image to the right and follow the contour of the spine you will notice that it arches backwards slightly. As mentioned at the start, the neck or cervical spine should arch gently forward toward the chin. In this particular case the cervical spine is kyphotic or going in the opposite direction that it should.
The internal jugular veins exit the skull through the jugular foramen on the floor of the skull just in front of the transverse process of the C1 vertebra of the upper cervical spine called atlas. After exiting the skull the internal jugular veins join the external jugular veins and follow the curve of the cervical spine on their way down from the head and back to the heart. In the case above, the internal jugulars like the cervical spine bend backward due to the cervical kyphosis. This causes a sharp change in the course of the normal direction of blood flow out of the brain as the internal jugular veins bend around the upper cervical spine. In addition to possibly impinging the internal jugular veins where they exit the skull in front of the transverse process of C1 (atlas), kyphosis most likely compresses the vertebral veins on the inside curve of the cervical spine similar to what scoliosis does in the rest of the spine. Kyphosis and scoliosis most likely play a significant role in CCSVI and CCVBP.
The angle of the upper cervical spine to the base of the skull is important to blood and CSF flow going into and out of the brain and cord. Likewise, the relationship of the base of the skull and upper cervical spine to the curve in the lower cervical spine is important to blood and CSF flow. Inherited and acquired misalignments and disorders of the upper cervical spine, as well as spondylosis (degeneration), scoliosis and other abnormal curves including kyphosis affect blood and CSF flow to the brain and cord. They also cause malpositioning and thus mechanical stress and strain of the brainstem and cord within the skull and spinal canal.
For further information on the upper cervical angle visit my website.
http://www.upright-health.com/upper-cervical-angle.html
Scoliosis, Chiari malformations and CCSVI
The spine is the frame of the body. Its alignment affects all the organs and vessels that surround or are attached to it, including the brain and its blood vessels. The spine also houses the cord, as well as its blood vessels and cerebrospinal fluid (CSF) pathways.
This post is about the impact of scoliosis on the contents of the posterior fossa of the skull, which includes the drainage system of the brain. Abnormal curvatures in the spine alter the normal alignment and relationship of the head and spine, and as a result, the normal relationship of the brain and cord. Curvatures also alter their circulatory routes.
While there may be an attachment of the covering of the upper cord to the foramen magnum, for the most part, the brain is unattached and floats freely inside compartments within the cranial vault. Similarly, the spinal cord is unattached and moves fairly freely inside the spinal canal to accommodate movement of the spine. The end of the spinal cord, called the filum terminale, attaches to the tail end of the spine, called the coccyx. Certain movements of the spine, such as flexion stretch and strain the cord somewhat. Abnormal curvatures of the spine stretch and strain the spine that much more and thus deform the cord and brainstem.
Scoliosis is an abnormal sidewards curvature of the spine. It is typically thought of as a childhood condition but adults can get scoliosis as well. A thoracolumbar scoliosis affects the thoracic and lumbar spines. The thoracic spine is attached to the ribcage. The lumbar spine is the low back.
A double major scoliosis starts in the low back and pelvis and bends one way and then reverses itself and bends the other way in the thoracic spine. The thought is the second curve is to help balance the head on the spine. This may not be the case all the time. The x-ray above is of a young female not quite seventeen. It is a perfect example of a double major scoliosis. The x-ray was contributed to Wikimedia by the University of Utah Hospital Department of Radiology from a case in 2009.
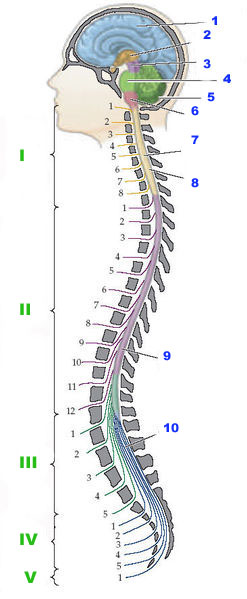 In most cases the cause of childhood scoliosis is unknown but it affects females far more than it does males. In this regard there is also a connection of scoliosis to tethered cord syndromes. In tethered cord the spinal cord is genetically too short for the length of the spine. This creates a strain putting tension on the cord, which causes a downward traction on the brainstem.
In most cases the cause of childhood scoliosis is unknown but it affects females far more than it does males. In this regard there is also a connection of scoliosis to tethered cord syndromes. In tethered cord the spinal cord is genetically too short for the length of the spine. This creates a strain putting tension on the cord, which causes a downward traction on the brainstem.
Compared to males, females finish developing neurologically much earlier than males. The body, however, can continue to grow and outgrow the length of the cord. It makes sense that the normal growth of the spine could be restrained by the tension caused by the cord thus resulting in a scoliosis. This could explain why tall females seem to be somewhat more susceptible to scoliosis.
In addition to tethered cords, scoliosis can also alter the normal position of the brain within the cranial vault. Tethered cords for example pull the brain down toward the foramen magnum and base of the skull. Head tilts and twists due to scoliosis, likewise, alter the normal alignment of the brain on top of the spine and inside the cranial vault. It is not surprising then, that scoliosis is also associated with Chiari malformations in which the cerebellum is dislocated to a position out of the posterior fossa and into the foramen magnum.
Adults can acquire scoliosis later in life due to injuries and degeneration of the spine such as from arthritis or osteoporosis. Parkinson’s disease also affects the normal alignment of the spine causing it to bend forward into flexion. Rheumatoid arthritis can cause severe destruction of the spine and subsequent scoliosis. Tethered cords can also be caused in adults by injuries and scar tissue inside the spinal canal that restrict the normal movement of the cord.
In addition to scoliosis, kyphosis is an abnormal backwards curve in the spine. Parkinson’s disease and osteoporosis can cause kyphosis. Some people are born with a kyphosis. Kyphosis of the cervical spine can occur as a result of whiplash injuries. Kyphosis, like scoliosis, alters the normal course of blood vessels. It can also create tension in the cord similar to scoliosis when it tethers the cord.
In addition to Chiari malformations and tethered cords, scoliosis and kyphosis alter the normal course of blood vessels and cerebrospinal fluid (CSF) pathways and can thus affect blood and CSF flow. Scoliosis and kyphosis most likely play a significant role in chronic cerebrospinal venous insufficiency, better known as CCSVI. It’s another topic I will cover in the future.
To get a better picture of the potential impact of scoliosis, Chiari malformation, and tethered cord on the brainstem and cerebellum in the posterior fossa click on the following link http://www.upright-health.com/posterior-fossa-chiari.html .
This post is about the impact of scoliosis on the contents of the posterior fossa of the skull, which includes the drainage system of the brain. Abnormal curvatures in the spine alter the normal alignment and relationship of the head and spine, and as a result, the normal relationship of the brain and cord. Curvatures also alter their circulatory routes.
While there may be an attachment of the covering of the upper cord to the foramen magnum, for the most part, the brain is unattached and floats freely inside compartments within the cranial vault. Similarly, the spinal cord is unattached and moves fairly freely inside the spinal canal to accommodate movement of the spine. The end of the spinal cord, called the filum terminale, attaches to the tail end of the spine, called the coccyx. Certain movements of the spine, such as flexion stretch and strain the cord somewhat. Abnormal curvatures of the spine stretch and strain the spine that much more and thus deform the cord and brainstem.
Scoliosis is an abnormal sidewards curvature of the spine. It is typically thought of as a childhood condition but adults can get scoliosis as well. A thoracolumbar scoliosis affects the thoracic and lumbar spines. The thoracic spine is attached to the ribcage. The lumbar spine is the low back.
A double major scoliosis starts in the low back and pelvis and bends one way and then reverses itself and bends the other way in the thoracic spine. The thought is the second curve is to help balance the head on the spine. This may not be the case all the time. The x-ray above is of a young female not quite seventeen. It is a perfect example of a double major scoliosis. The x-ray was contributed to Wikimedia by the University of Utah Hospital Department of Radiology from a case in 2009.
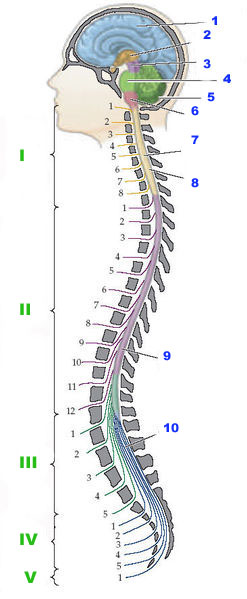 In most cases the cause of childhood scoliosis is unknown but it affects females far more than it does males. In this regard there is also a connection of scoliosis to tethered cord syndromes. In tethered cord the spinal cord is genetically too short for the length of the spine. This creates a strain putting tension on the cord, which causes a downward traction on the brainstem.
In most cases the cause of childhood scoliosis is unknown but it affects females far more than it does males. In this regard there is also a connection of scoliosis to tethered cord syndromes. In tethered cord the spinal cord is genetically too short for the length of the spine. This creates a strain putting tension on the cord, which causes a downward traction on the brainstem.Compared to males, females finish developing neurologically much earlier than males. The body, however, can continue to grow and outgrow the length of the cord. It makes sense that the normal growth of the spine could be restrained by the tension caused by the cord thus resulting in a scoliosis. This could explain why tall females seem to be somewhat more susceptible to scoliosis.
In addition to tethered cords, scoliosis can also alter the normal position of the brain within the cranial vault. Tethered cords for example pull the brain down toward the foramen magnum and base of the skull. Head tilts and twists due to scoliosis, likewise, alter the normal alignment of the brain on top of the spine and inside the cranial vault. It is not surprising then, that scoliosis is also associated with Chiari malformations in which the cerebellum is dislocated to a position out of the posterior fossa and into the foramen magnum.
Adults can acquire scoliosis later in life due to injuries and degeneration of the spine such as from arthritis or osteoporosis. Parkinson’s disease also affects the normal alignment of the spine causing it to bend forward into flexion. Rheumatoid arthritis can cause severe destruction of the spine and subsequent scoliosis. Tethered cords can also be caused in adults by injuries and scar tissue inside the spinal canal that restrict the normal movement of the cord.
In addition to scoliosis, kyphosis is an abnormal backwards curve in the spine. Parkinson’s disease and osteoporosis can cause kyphosis. Some people are born with a kyphosis. Kyphosis of the cervical spine can occur as a result of whiplash injuries. Kyphosis, like scoliosis, alters the normal course of blood vessels. It can also create tension in the cord similar to scoliosis when it tethers the cord.
In addition to Chiari malformations and tethered cords, scoliosis and kyphosis alter the normal course of blood vessels and cerebrospinal fluid (CSF) pathways and can thus affect blood and CSF flow. Scoliosis and kyphosis most likely play a significant role in chronic cerebrospinal venous insufficiency, better known as CCSVI. It’s another topic I will cover in the future.
To get a better picture of the potential impact of scoliosis, Chiari malformation, and tethered cord on the brainstem and cerebellum in the posterior fossa click on the following link http://www.upright-health.com/posterior-fossa-chiari.html .
Spondylosis, Stenosis, Cog Fog and Dementia

Dementia is a loss of cognitive ability, such as loss of memory, concentration, language and problem solving. Dementia is seen in many neurodegenerative diseases including Alzheimer’s and Parkinson’s disease. Furthermore, cog fog is a common complaint among multiple sclerosis patients. Cog fog is simply a milder form of cognitive impairment compared to what is commonly considered to be dementia. In any case, dementia and cog fog may share similar causes.
The x-ray on the left is a lateral (side) view of a fairly normal cervical spine. The bones, cartilage and joints are all normal in size, shape and spacing. The gray spaces are the discs made of cartilage, and posterior to them are the facets or joints that separate the vertebral segments of the spine.
There are many different types of inherited disorders that can affect the normal design of the base of the skull and cervical spine and thus impair blood and cerebrospinal fluid (CSF) flow in the brain and cord. They fall into categories called: craniosynostosis, craniodyostosis and craniocervical junction abnormalities, which is the base of the skull and upper cervical spine. One of the first types of inherited disorders of connective tissues I studied when I began my research is a condition called craniocleidodysostosis. It is a very rare condition in which cartilage in an infant fails to turn into bone resulting in significant deformation of the skull, clavicals and spine among other things. I also grew up witnessing first hand the impact of severe rheumatoid arthritis on the upper cervical spine and the serious neurological consequences it can have. Both my mother and her mother, my grandmother died quite young due to complications including a slipped odontoid process of the second cervical vertebra (C2) called axis. Rheumatoid arthritis is also considered to be an inherited disorder of connective tissues. The inflammatory arthritides are a separate subject I cover at another time.
In addition to inherited disorders, even more people are affected by acquired disorders due to diseases such as rheumatoid arthritis mentioned above, psoriatic arthritis, lupus erythematosis and osteoarthritis to name just a few. Lastly, everyone is affected by degeneration of the spine due to injuries and aging. Diseases and trauma simply speed up the process and generally make it worse. Inherited disorders tend to show up early in life because of the design flaws. Conditions related to trauma show up later, in midlife, and conditions related to aging degeneration tend to show up late in life. In brief, I categorize all of the different conditions collectively under the umbrella term craniocervical syndromes. The list of craniocervical syndromes is long. Although the different types of craniocervical syndromes are rare by themselves, collectively they affect many people.
 Degeneration of the cervical spine is called spondylosis. This lateral view x-ray of the neck shows spondylosis in the lower cervical spine. If you look at the gray spaces between the bones and compare it to the picture above you will see that they are much thinner. As mentioned above, the gray spaces are the cartilage or discs of the spine. The bones show distortion on the front side and are less square with pointed edges due to compression that caused their inner support structures to collapse.
Degeneration of the cervical spine is called spondylosis. This lateral view x-ray of the neck shows spondylosis in the lower cervical spine. If you look at the gray spaces between the bones and compare it to the picture above you will see that they are much thinner. As mentioned above, the gray spaces are the cartilage or discs of the spine. The bones show distortion on the front side and are less square with pointed edges due to compression that caused their inner support structures to collapse.When the bones, cartilage and connective tissues of the spine, such as the ligaments degenerate they sometimes bulge and buckle backward which invades the space of the spinal canal and outlets for the spinal nerves. Technically it’s called stenosis. Stenosis means narrowing. When it becomes severe enough stenosis can compress the nerve roots and cord causing neurological signs and symptoms. It may even lead to dementia.
More and more evidence is starting to link head injuries to Alzheimer’s disease, Parkinson’s disease and dementia. Controversy, likewise, continues to surround the role of trauma in multiple sclerosis. Research has come a long way in understanding traumatic brain injuries which occur immediately after the trauma. In contast to traumatic brain injuries that occur at the time of the accident the symptoms of cog fog and dementia start to show up many years, sometimes decades later even when they are from the same cause.
In this regard, head and neck injuries often occur together. Unless it is fractured, the skull is oftentimes undamaged. The bones, cartilage and connective tissues of the spine, however, are much more vulnerable to serious strains and sprains that can initiate the degenerative process. In contrast to nerves, the hard and soft tissues of the spine breakdown slowly over years, which leads to spondylosis.
 The brain scan on the left is a perfect example of spondylosis. The cord is the long gray tube that drops down from the brainstem. The white area is blood and cerebrospinal fluid. If you look down at the lower cervical spine you can see that the white area is indented. The indentations are caused by degeneration of the bones, cartilage and connective tissues that spread into the spinal canal and if severe enough, compress the cord.
The brain scan on the left is a perfect example of spondylosis. The cord is the long gray tube that drops down from the brainstem. The white area is blood and cerebrospinal fluid. If you look down at the lower cervical spine you can see that the white area is indented. The indentations are caused by degeneration of the bones, cartilage and connective tissues that spread into the spinal canal and if severe enough, compress the cord.Oftentimes, however, spondylosis compresses the thecal sac of the cord without compressing the cord directly. But the thecal sac contains the vertebral veins of the cord so that compression can lead to what is called venous hypertension, which is an increase in venous pressure.
Acccording to a study done by Rutger’s University, vertebral venous hypertension is one of the most overlooked causes of ischemia of the arterial blood supply to the cord. The arterial blood supply to the cervical cord comes from the vertebral arteries. In this regard, the vertebral arteries also supply the lower inner lobes of the brain, thalamus, hypothalmaus, brainstem and cerebellum. Furthermore, the brain sits further upstream and above the level of the neck making it more susceptible to decreased blood flow from the vertebral arteries due to distance and gravity. Vertebral venous hypertension, that is, back pressure against the vertebral veins, can thus decrease blood flow to the brain the same way it decreases blood flow to the cord by decreasing the pressure gradient. It can also affect the drainage of the brain, as well as CSF flow in the brain and cord, which is closely connected to venous flow.
The health of the cervical spine is important to the health of the brain. Cervical spondylosis and stenosis may play a role in chronic edema, ischemia and normal pressure hydrocephalus. It may also play a role in cog fog and dementia.
For further information on head injuries and dementia check out the following links: dementia and Parkinson’s, Dementia and Neck Injuries
Craniocervical Syndromes, EDS and MS
There are many different types of inherited and acquired disorders, as well as degenerative conditions (aging and wear and tear) of the cervical spine, especially the upper cervical spine (skull and upper cervical spine). I refer to them as craniocervical syndromes in my book. Craniocervical syndromes can cause and array of neurological signs and symptoms related to the brain and cord.
Craniocervical syndromes cause problems by compressing blood and cerebrospinal fluid pathways going into and out of the brain and cord. They can also cause compressive myelopathy of the cervicomedullary cord; which is compression of the lower brainstem and upper cord. Craniocervical syndromes can thus cause an array of signs and symptoms.
In the brain scan above the cauliflower looking structure, at the lower rear part of the brain, is the cerebellum. In front of and below the cerebellum is a verticle tube-like structure which is the brainstem and cord. At the top of the tube-like structure is a round protruding belly-like part of the brainstem in front of the cerebellum called the pons. Above the pons is the midbrain of the brainstem and below it is the medulla oblongata which is the lowest part of the brainstem that connects to the highest part of the spinal cord. Pons is the Latin word for bridge. The pons was called a bridge because it links the midbrain, cerebellum and medulla of the brainstem together.
In front of the pons and behind a black circular structure (the sphenoid sinus) is a white triangular shaped structure with what could be described as a white cup at the very top. The structure is the clivus of the base of the skull. The cup is the compartment in the skull that contains the pituitary gland, which is the master gland that controls the endocrine system. The very bottom of the clivus is the front side of the foramen magnum. This is a large opening in the base of the skull to accommodate the brainstem and cord. Across from it and under the cerebellum (cauliflower) is a thin white strip which is part of the occipital bone that forms the rear of the foramen magnum.
Just below the bottom of the clivus on the front side of the foramen magnum is a white peg-like structure with a black line shaped like a cap over it. The peg-like structure is the dens or odontoid part of the second cervical vertebra below the skull. The dens sits in a pocket of the atlas or first cervical vertebra. The dens is a pivot joint for left and right rotation of the neck. The black line, in front and back of the dens, is fluid that lubricates the joint. A ligament holds the dens in place inside the atlas formed pocket and keeps it from moving posteriorly (back) causing it to compress the spinal cord.
 The cerebellum sits in its own compartment called the posterior fossa. The dark shadow above the cerebellum is the tent-like covering over the posterior fossa called the tentorium cerebelli. The covering is not flat but angles upward. There is a whole in the covering called the incisura for the brainstem to pass through to the foramen magnum and cord below. In the graphic picture on the left, the green area is the right half of the tentorium cerebelli that covers the cerebellum in the posterior fossa below. It divides the brain into upper and lower comparments. The light red area represents the falx cerebri, which is a vertical curtain of connective tissue similar to the tentorium that divides the brain into left and right halves. A similar vertical curtain of connective tissue, called the falx cerebelli, also separtes the posterior fossa and cerebellum into left and right sides.
The cerebellum sits in its own compartment called the posterior fossa. The dark shadow above the cerebellum is the tent-like covering over the posterior fossa called the tentorium cerebelli. The covering is not flat but angles upward. There is a whole in the covering called the incisura for the brainstem to pass through to the foramen magnum and cord below. In the graphic picture on the left, the green area is the right half of the tentorium cerebelli that covers the cerebellum in the posterior fossa below. It divides the brain into upper and lower comparments. The light red area represents the falx cerebri, which is a vertical curtain of connective tissue similar to the tentorium that divides the brain into left and right halves. A similar vertical curtain of connective tissue, called the falx cerebelli, also separtes the posterior fossa and cerebellum into left and right sides.
The posterior fossa and upper cervical spine are critical to blood and CSF flow and contain some of the most crucial components of the brain and cord. Many conditions affect the upper cervical spine and base of the skull predisposing humans to neurodegenerative conditions and subsequent diseases. This is due to the unique design of the skull, spine and circulatory system of the brain and cord as a result of upright posture.
One genetic condition in particular underscores the role of craniocervical syndromes in neurodegenerative conditions due to it’s design flaws. That condition is Ehlers-Danlos syndrome or EDS. Even the short version of EDS is far too long to discuss here but is discussed on my website. In brief, certain cases of Ehlers-Danlos Syndrome (EDS) affect the design of the skull and some affect the upper cervical spine resulting in Chiari malformations and hydrocephalus type condtions among other things.
I will discuss other craniocervical syndromes that can cause similar problems as the website develops. The design of the base of the skull and upper cervical spine needs to be studied much further. It may be a key culprit in many neurodegenerative conditions. Upright MRI will shed much more light on this in the future.
For additional information on this and other related topics as well as my book go to my website at www.upright-health.com.
Craniocervical syndromes cause problems by compressing blood and cerebrospinal fluid pathways going into and out of the brain and cord. They can also cause compressive myelopathy of the cervicomedullary cord; which is compression of the lower brainstem and upper cord. Craniocervical syndromes can thus cause an array of signs and symptoms.
In the brain scan above the cauliflower looking structure, at the lower rear part of the brain, is the cerebellum. In front of and below the cerebellum is a verticle tube-like structure which is the brainstem and cord. At the top of the tube-like structure is a round protruding belly-like part of the brainstem in front of the cerebellum called the pons. Above the pons is the midbrain of the brainstem and below it is the medulla oblongata which is the lowest part of the brainstem that connects to the highest part of the spinal cord. Pons is the Latin word for bridge. The pons was called a bridge because it links the midbrain, cerebellum and medulla of the brainstem together.
In front of the pons and behind a black circular structure (the sphenoid sinus) is a white triangular shaped structure with what could be described as a white cup at the very top. The structure is the clivus of the base of the skull. The cup is the compartment in the skull that contains the pituitary gland, which is the master gland that controls the endocrine system. The very bottom of the clivus is the front side of the foramen magnum. This is a large opening in the base of the skull to accommodate the brainstem and cord. Across from it and under the cerebellum (cauliflower) is a thin white strip which is part of the occipital bone that forms the rear of the foramen magnum.
Just below the bottom of the clivus on the front side of the foramen magnum is a white peg-like structure with a black line shaped like a cap over it. The peg-like structure is the dens or odontoid part of the second cervical vertebra below the skull. The dens sits in a pocket of the atlas or first cervical vertebra. The dens is a pivot joint for left and right rotation of the neck. The black line, in front and back of the dens, is fluid that lubricates the joint. A ligament holds the dens in place inside the atlas formed pocket and keeps it from moving posteriorly (back) causing it to compress the spinal cord.
 The cerebellum sits in its own compartment called the posterior fossa. The dark shadow above the cerebellum is the tent-like covering over the posterior fossa called the tentorium cerebelli. The covering is not flat but angles upward. There is a whole in the covering called the incisura for the brainstem to pass through to the foramen magnum and cord below. In the graphic picture on the left, the green area is the right half of the tentorium cerebelli that covers the cerebellum in the posterior fossa below. It divides the brain into upper and lower comparments. The light red area represents the falx cerebri, which is a vertical curtain of connective tissue similar to the tentorium that divides the brain into left and right halves. A similar vertical curtain of connective tissue, called the falx cerebelli, also separtes the posterior fossa and cerebellum into left and right sides.
The cerebellum sits in its own compartment called the posterior fossa. The dark shadow above the cerebellum is the tent-like covering over the posterior fossa called the tentorium cerebelli. The covering is not flat but angles upward. There is a whole in the covering called the incisura for the brainstem to pass through to the foramen magnum and cord below. In the graphic picture on the left, the green area is the right half of the tentorium cerebelli that covers the cerebellum in the posterior fossa below. It divides the brain into upper and lower comparments. The light red area represents the falx cerebri, which is a vertical curtain of connective tissue similar to the tentorium that divides the brain into left and right halves. A similar vertical curtain of connective tissue, called the falx cerebelli, also separtes the posterior fossa and cerebellum into left and right sides.The posterior fossa and upper cervical spine are critical to blood and CSF flow and contain some of the most crucial components of the brain and cord. Many conditions affect the upper cervical spine and base of the skull predisposing humans to neurodegenerative conditions and subsequent diseases. This is due to the unique design of the skull, spine and circulatory system of the brain and cord as a result of upright posture.
One genetic condition in particular underscores the role of craniocervical syndromes in neurodegenerative conditions due to it’s design flaws. That condition is Ehlers-Danlos syndrome or EDS. Even the short version of EDS is far too long to discuss here but is discussed on my website. In brief, certain cases of Ehlers-Danlos Syndrome (EDS) affect the design of the skull and some affect the upper cervical spine resulting in Chiari malformations and hydrocephalus type condtions among other things.
I will discuss other craniocervical syndromes that can cause similar problems as the website develops. The design of the base of the skull and upper cervical spine needs to be studied much further. It may be a key culprit in many neurodegenerative conditions. Upright MRI will shed much more light on this in the future.
For additional information on this and other related topics as well as my book go to my website at www.upright-health.com.
Posted in ccsvi, chiari malformations, Devic's disease, Ehlers Danlos Syndrome, multiple sclerosis, optic spinal multiple sclerosis, physical anthropology Tagged Arnold–Chiari malformation, Base of skull, Brainstem, Cervical vertebrae, Ehlers–Danlos syndrome, Foramen magnum, Posterior cranial fossa, Spinal cord 7 Comments
C1, C2 and CSF Flow
The picture on the left is from promotional material for Fonar Corporation’s upright MRI. In this regard, my theory is that humans are predisposed to neurodegenerative diseases such as Alzheimer’s, Parkinson’s and multiple sclerosis due to the unique design of the skull, spine and circulatory system of the brain as a result of upright posture. In addition to blood flow, upright posture also changes CSF flow. Besides its added benefit in many other health conditions, when it comes to blood and CSF flow, upright MRI is the wave of the future in brain research.
Cerebrospinal fluid (CSF) flow is called the third circulation of the brain and it is the least understood. CSF production and flow is critical to brain cushioning and protection. In terms of protection CSF is important to brain support to prevent the brain from sinking in the cranial vault. Conversely, excess CSF volume compresses the brain.
CSF comes from arterial blood that has been filtered through the blood brain barrier to the point where it is mostly water. CSF leaves the brain through the venous system. Therefore, backups in the venous drainage system affect cerebrospinal fluid (CSF) flow and drainage. Although it uses other routes as well, such as cranial and spinal nerves and the lymphatic system, most of the cerebrospinal fluid (CSF) produced by the brain eventually makes its way up to the superior sagittal sinus where it empties into the venous system.
The superior sagittal sinus, depicted in the graphic image on the right, is the largest dural sinus located at the top of the brain. The superior sagittal sinus contains arachnoid granulations that act as one way check valves for the flow of CSF from the subarachnoid space to the sinus. Click on the image for a better view. The pulsatile nature and the pressure generated by the CSF outflow through the arachnoid granulations is powerful enough to scour impressions into the roof of the cranial vault.Cerebrospinal fluid (CSF) flow is called the third circulation of the brain and it is the least understood. CSF production and flow is critical to brain cushioning and protection. In terms of protection CSF is important to brain support to prevent the brain from sinking in the cranial vault. Conversely, excess CSF volume compresses the brain.
CSF comes from arterial blood that has been filtered through the blood brain barrier to the point where it is mostly water. CSF leaves the brain through the venous system. Therefore, backups in the venous drainage system affect cerebrospinal fluid (CSF) flow and drainage. Although it uses other routes as well, such as cranial and spinal nerves and the lymphatic system, most of the cerebrospinal fluid (CSF) produced by the brain eventually makes its way up to the superior sagittal sinus where it empties into the venous system.
About sixty percent of the CSF produced in the brain ends up in the spinal cord. Eventually most of the CSF in the spinal cord makes its way back up through the subarachnoid space of the cord and into the subarchnoid space of the brain. From there it travels up to the superior sagittal sinus and arachnoid granulations to exit the brain along with venous blood.
The movement of CSF is driven by cardiovascular waves arising from the heart and blood vessels. During the contraction phase of the heart cycle (systole) pressure in the arteries of the brain increases. The increase in blood pressure drives CSF out of the brain through the upper cervical spine because as blood volume rises CSF volume must decrease. During the relaxation phase (diastole) the pressure drops and CSF enters the cranial vault through the subarachnoid space of the upper cervical spine. In addition, because the veins of the vertebral venous plexus of the spine have no valves, respiratory pressure changes are transmitted to the brain and amplify the cardiovascular waves. In brief, as pressure in the chest cavity drops during inspiration, due to the diaphram moving down and the chest wall moving out, CSF is pulled out of the cranial vault. As pressure in the chest cavity increases during exhalation CSF is driven into the cranial cavity. Thus, combined cardiorespiratory waves are important to the movement of CSF through the brain and cord.
The CSF that leaves the brain on its way down to the cord , however, must first pass through the tight neural (spinal) canal of the the upper cervical spine. Likewise, on its return trip back to the brain, it must again pass through the neural canal of the upper cervical spine. Therefore, the upper cervical spine is a critical link in the flow of CSF between the subarachnoid space of the brain and the cord. Under normal circumstances cardiorespiratory waves move CSF through the neural canal of the upper cervical spine unimpeded with good pulsatility and continue to drive it through the subarachnoid space up to the superior sagittal sinus.
Genetic design flaws, such as Chiari malformations, and acquired disorders from injuries or disease can impede the pulsatility and flow of CSF through the upper cervical spine. Restrictions in CSF flow that cause a decrease in its volume, can, in turn, cause Chiari malformations and pressure conus conditions. Furthermore, any condition that restricts CSF flow can lead to hydrocephalus-like conditions. It is therefore important to maintain the correct volume of CSF in order to provide sufficient brain support and protection, as well as to prevent hydrocephalus.
The picture above shows a fairly severe rotational misalignment of the upper cervical spine to the right. Click on the image for a better view. The dart shaped structure in the upper cervical spine is the spinous process of C2. It should be in the midline. The misalignment was caused by a motorcycle accident in which the victim landed on the right side of his head causing his head to snap to the left while simultaneously shifting and twisting his upper cervical spine to the right. Misalignments, such as the one above (due to micro or macro trauma), genetic design flaws (Chiari malformations), diseases (rheumatoid arthritis) and degenerative conditons (aging) of the upper cervical spine can affect the vertebral arteries that supply the brain, as well as the vertebral veins that drain the brain during upright posture. They can also cause deformation of the subarachnoid space and consequently, they can affect CSF flow going into and out of the brain and cord.
While CCSVI treatment can improve venous drainage, which may further relieve hydrocephalic conditions in certain cases, it cannot improve CSF flow through the subarachnoid space of the upper cervical spine. Furthermore, increasing venous drainage of the brain and consequently decreasing CSF volume without a proportionate rise in passive CSF production could compromise brain support causing it to sink in the vault resulting in a condition similar to a pressure conus or Chiari malformation. Over drainage of the brain may thus present problems similar to spinal taps which can cause headaches due to a pressure conus condition following CSF removal. Over drainage is probably less likely in younger cases where the passive CSF pressure gradient and CSF production remains strong. Older patients, on the other hand, may have a lower CSF pressure gradient and thus a decrease in passive production of CSF due to aging of the brain and chronic craniocervical back pressure against the vertebral veins and subarachnoid space.
The flow of CSF clearly plays a role in normal pressure hydrocephalus (NPH), which has been associated with Alzheimer’s and Parkinson’s disease. It also plays a role in Chiari malformations, which cause signs and symptoms similar to MS. I discuss CSF production and flow thoroughly in my book. I will be discussing it more here in future posts as well as on my new website at: http://www.upright-health.com/.
Chiari Malformations and Cranial Nerves
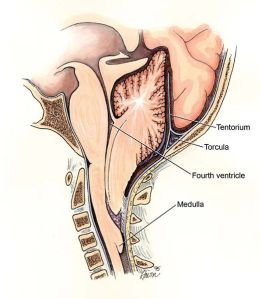 Chiari malformations are typically associated with herniation of the brainstem into the foramen magnum in the base of the skull as shown in the picture on the left. More recently, it has come to include what is called a Zero Chiari Malformation in which the cerebellum comes in contact with the base of the cranial vault without herniation into the foramen magnum. This has prompted some researchers to suggest that Chiari malformations include any decrease in cerebrospinal fluid volume (CSF) sufficient enough to cause the brain to sink and come in contact with the bones of the base of the skull.
Chiari malformations are typically associated with herniation of the brainstem into the foramen magnum in the base of the skull as shown in the picture on the left. More recently, it has come to include what is called a Zero Chiari Malformation in which the cerebellum comes in contact with the base of the cranial vault without herniation into the foramen magnum. This has prompted some researchers to suggest that Chiari malformations include any decrease in cerebrospinal fluid volume (CSF) sufficient enough to cause the brain to sink and come in contact with the bones of the base of the skull.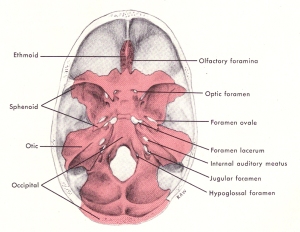 Considering the above, in addition to the foramen magnum there are other large holes in the base of the skull through which cranial nerves and blood vessels pass, as seen in the picture on the right. It is possible that the cranial nerves may herniate into the openings or come in contact with the base of the skull due to Chiari malformations in which the volume of CSF falls too low, as mentioned above. The consequence would be similar, as well, that is cause compression of nerves and circulatory routes.
Considering the above, in addition to the foramen magnum there are other large holes in the base of the skull through which cranial nerves and blood vessels pass, as seen in the picture on the right. It is possible that the cranial nerves may herniate into the openings or come in contact with the base of the skull due to Chiari malformations in which the volume of CSF falls too low, as mentioned above. The consequence would be similar, as well, that is cause compression of nerves and circulatory routes. The brain floats within the cranial vault. Typically, it is prevented from sinking into the foramen magnum by the cisterns of the brain which are filled with cerebrospinal fluid (CSF). The cisterns are also strategically placed to provide cushioning, support and protection from the hard bones of the cranial vault as seen in the picture on the left.
The brain floats within the cranial vault. Typically, it is prevented from sinking into the foramen magnum by the cisterns of the brain which are filled with cerebrospinal fluid (CSF). The cisterns are also strategically placed to provide cushioning, support and protection from the hard bones of the cranial vault as seen in the picture on the left.Symptoms of MS often include cranial nerves. Common complaints include dizziness, ringing in the ears or loss of hearing, trigeminal neuralgia, burning tongue and dry mouth. By far, however, the cranial nerve most commonly involved in MS is the optic nerve. Optic neuritis is, in fact, one of the most frequent symptoms of MS. Even Asians and African-Americans who, otherwise, have a much lower incidence of MS, get optic neuritis. They also get transverse myelitis, but that’s another topic entirely. I will be covering the different cranial nerve signs, as well as transverse myelitis on my new website starting with the optic nerve.
The optic nerve is the second most superior (highest) nerve in the cranial vault. The highest cranial nerve is the olfactory nerve to the nose which is located in the anterior fossa or forehead area of the base of the skull. The optic nerve lies in the middle fossa behind the eye sockets. Most of the cranial nerves are in the posterior fossa along with the brainstem and cerebellum.
It’s position in the cranial vault and the optic canal may be the reason why optic neuritis is one of the most common signs and symptoms of MS, optic-spinal MS and Devic’s disease. Typically, the optic nerve is protected by the chiasmatic cistern, which is one of the highest cisterns in the brain. Among other things trauma and failure of the CSF support system of the brain may play a role in optic neuritis. For further information on optic neuritis click on the link below to my new website. The website can also be found in the links section of the sidebar under upright-health.
http://www.upright-health.com/optic-neuritis.html
Skull Design and Brainstem Compression
 When it comes to physical anthropology and skull shapes race is a highly contentious issue. It’s not clear-cut because there are many variations among races. To keep it simple I refer to the different skull shapes as square, rectangular and round designs based on their overall outlines and the shapes of the orbits of the eyes and nose.
When it comes to physical anthropology and skull shapes race is a highly contentious issue. It’s not clear-cut because there are many variations among races. To keep it simple I refer to the different skull shapes as square, rectangular and round designs based on their overall outlines and the shapes of the orbits of the eyes and nose.Basically there are three distinct shapes in the design of the human skull, European, Asian and African. Although, there are slight variations, the cranial capacity is roughly the same and varies from about 1200 to 1800 cc. Asians tend to have the largest cranial capacity followed in size by European and African designs. Regardless of size, however, humans have roughly the same amount of nerves in the brain. Larger brains simply have larger nerves and support tissues, not necessarily more nerves.
The human brain is relatively large compared to body size. The base of the skull, however, is relatively short. This short base is due to forward migration of the foramen magnum over time toward the middle of the skull beneath the mass of the head and brain. The foramen magnum is the large hole in the base of the skull through which the brainstem passes to the cord.
 In the picture on the left the front part of the base of the skull is from the back of the nose to the notch in the yellow colored bone called the sella turcica where the pituitary gland is located. Unlike the picture, it tends to slop upwards slightly. The base then bends downward at a steep angle along the back of the yellow colored bone and along the blue colored bone. Technically, together the two bones are called the clivus portion of the base. The face of the brainstem and most of the cranial nerves are located just above the clivus. The foramen magnum for the cord is at the bottom of the clivus. The rear portion of the base extends behind the foramen magnum. The rear portion of the base is also called the posterior fossa. The base of the posterior fossa also slopes upwards.
In the picture on the left the front part of the base of the skull is from the back of the nose to the notch in the yellow colored bone called the sella turcica where the pituitary gland is located. Unlike the picture, it tends to slop upwards slightly. The base then bends downward at a steep angle along the back of the yellow colored bone and along the blue colored bone. Technically, together the two bones are called the clivus portion of the base. The face of the brainstem and most of the cranial nerves are located just above the clivus. The foramen magnum for the cord is at the bottom of the clivus. The rear portion of the base extends behind the foramen magnum. The rear portion of the base is also called the posterior fossa. The base of the posterior fossa also slopes upwards. In some skulls the angle of the clivus is relatively steep. In others it is flatter. Regardless of the angle of the clivus, all humans are predisposed to the brainstem sinking into the foramen magnum due to its location beneath the skull. A Chiari malformation occurs when the brainstem sinks into the foramen magnum as seen in the brain scan to the right.
In some skulls the angle of the clivus is relatively steep. In others it is flatter. Regardless of the angle of the clivus, all humans are predisposed to the brainstem sinking into the foramen magnum due to its location beneath the skull. A Chiari malformation occurs when the brainstem sinks into the foramen magnum as seen in the brain scan to the right.Typically, the brainstem is surrounded by cisterns filled with cerebrospinal fluid (CSF) which allows the brain to float above the foramen magnum and base of the skull thus preventing contact with the bones of the base and foramen magnum. In a Chiari malformation, it is typically the tonsillar portion of the cerebellum that gets trapped in the foramen magnum.
In this regard, among other things, the design of the posterior fossa may explain why people of European race have a much higher incidence of multiple sclerosis than people of Asian and African races. While the floor of the posterior fossa slopes slightly upwards in all races, it is considerably shorter in European skulls than it is in Asian and African ones. The rear wall of the posterior fossa in European skulls also slant outward. Thus European designs tend to crowd the cerebellum, comparatively speaking, from front to back more than Asian and African designs. They also pitch the cerebellum forward and downward toward the foramen magnum. Additionally, the design of the shorter sloped floor and slanted rear wall also affects the length, pitch and layout of the drainage system of the brain. Shorter distances and reduced angles in the base of the European skull most likely reduces curves and provides less resistance to reverse flows of venous blood in the dural sinuses.
Lastly, in contrast to European skulls, the jaws of Asian skulls are more in line with the face which improves balance on top of the cervical spine and makes them more energy-efficient. Protruding muzzles in European designs also create greater swing weights when the head is whiplashed as in trauma. In contrast to taller and narrower European and Asian skull faces, African skulls have shorter, wider and deeper faces. The lower wider face lowers the center of gravity and swing weight, and like Asian skulls, may provide better protection to the head and neck, as well as the brain and cord in whiplash type traumas.
In brief, the similar designs of the Asian and African posterior fossa of the rear portion of the base of the skull may provide better protection for the brain from whiplash, inversion flows and classic MS. On the other hand, it may also explain why Asian and African races tend to get a variant of MS called optic-spinal multiple sclerosis and Devic’s disease. Both conditions are associated with optic neuritis and transverse myelitis rather than classic MS lesions, signs and symptoms.
The different signs and symptoms in the above conditions may be the consequence of different points of contact and compression of the underside of the brain against the base of the vault and within the foramen magnum. The differences in contact points may be due to design differences in the base of the skull. In my next post I will discuss the location of the brainstem and cranial nerves in relationship to the base of the skull and foramen magnum. Their location makes them highly susceptible to compression by either an increase or a decrease in CSF volume in the cisterns.
For additional information on this and related topics visit my website at http://www.upright-health.com.
Round Heads and Devic’s MS
 My clinic partner in chiropractic school was part Japanese and part Hawaiian. He had a huge round head. I used to tease him and say it was so big and round you could bowl with it. His eyes, which were mere slits, would get even smaller as he broke out in a grin. I would look him square in the eyes and say how do you see out of those things and the remaining slits would turn to dashes as his grin stretched and strained his cheeks to the max.
My clinic partner in chiropractic school was part Japanese and part Hawaiian. He had a huge round head. I used to tease him and say it was so big and round you could bowl with it. His eyes, which were mere slits, would get even smaller as he broke out in a grin. I would look him square in the eyes and say how do you see out of those things and the remaining slits would turn to dashes as his grin stretched and strained his cheeks to the max.The roundness of the head and eye sockets is evident in the well cast skull seen above. Permission to use the pictures of the skull in this post was granted by Bone Clones Inc. The aperture of the nose is also rounder compared to the more triangular shape of European skull design.
The head is the sound box of the human voice. The tonal quality of the voice is affected by the design of the head, especially the mouth, nose and air sinuses, called the paranasal sinuses.
The bridge of the nose, called the glabella, sits above the opening. Behind the bridge are the ethmoid sinuses. The large maxillary sinuses lie beneath the cheek bones to the sides of the nose. The frontal sinuses are in the forehead just above the nose. The sphenoid sinus sits behind and between the eyes. Singing resonates in the sinuses and escapes through the nose. Yoga kundalini exercise uses the AUM chant to resonate the sphenoid sinus and stimulate the pituitary gland which sits above the sphenoid sinus. The difference in shape of the nasal opening affects the escape of air like the difference in shape between f holes in violins and jazz guitars and round holes in country guitars.
 In this regard, the design of the African-American skull is a perfect shape for singing. One of the finest quality voices ever recorded was that of Nat King Cole. Rich and mellow the music would escape his head with near perfect unobstructed flow.
In this regard, the design of the African-American skull is a perfect shape for singing. One of the finest quality voices ever recorded was that of Nat King Cole. Rich and mellow the music would escape his head with near perfect unobstructed flow.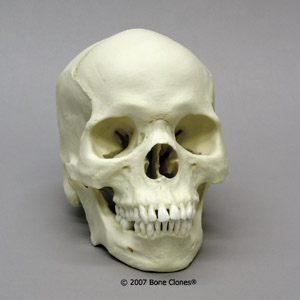 If you strip away the flesh it’s easy to see that the roundness of an African-American skull is closer in design to Asian skulls. The head is not box-like as in European designs, but smoother and rounder. The eye sockets are also rounder. The nasal aperture is especially round.
If you strip away the flesh it’s easy to see that the roundness of an African-American skull is closer in design to Asian skulls. The head is not box-like as in European designs, but smoother and rounder. The eye sockets are also rounder. The nasal aperture is especially round.The difference in the round designs versus square European designs may explain why Asians and African-Americans have a much lower incidence of MS. On the other hand, it may explain why they get a particularly devastating variant form of MS called Devic’s disease.
The floor of the base of Asian and African skulls is longer than European skulls. The back wall of the head in Asians is taller but slightly more sloped than African designs which are steeper. The longer base and steep rear wall distribute more of the weight of the brain behind the foramen. On the other hand, it positions the brainstem over the foramen magnum prediposing it to sinking into a Chiari malformation.
Chiari malformations were once considered to be a herniation of the brainstem into the foramen magnum thus compressing it. More recent research suggests that the definition should be changed to include any decrease in CSF volume which causes the brain to sink and come in contact with the bones of the cranial vault. Recent research has also linked Chiari malformations with trauma, MS and chronic fatigue syndrome among other things.
Devic’s disease is associated with neuromyelitis optica and transverse myelitis but typically has no MS-like lesions in the brain. While transverse myelitis is associated with hyperintensity signals in the cord, the lesions differ from MS in that they are longer and tend to span several segments of the spine. Devics disease can result in blindness and muscle weakness in the arms and legs. It can also cause respiratory failure.
The optic nerve sits beneath the weight of the frontal lobes of the brain. It is protected from compression by cerebrospinal fluid (CSF) in the interchiasmatic cistern, which is the highest cistern in the brain. In round skull designs Chiari malformations most likely result in contact of the frontal lobe of the brain against the vault thus compressing the optic nerve. Herniation of the brainstem into the foramen magnum further compresses the long nerve tracts from the brain that go to the cord resulting in muscle weakness and respiratory stress.
Let’s consider a hypothetical example of a European, Asian and African-American traveling together in a car that gets into a traumatic motor vehicle accident. Soon afterwards they all develop problems with loss of vision and weakness in the legs. Brain scans show white spots in the brain of the European and in the cord of the Asian and African-American. In this case the European person is diagnosed with MS and the Asian and African-American with Devic’s disease. In all three cases, it will be blamed on an immunolgical problem, when in fact it is simply a different response to the same traumatic cause.
For more information on this and related topics visit my website at http://www.upright-health.com
Square Heads and MS
 Many years ago when I was a young boy, the carpenter’s union was mostly comprised of men of Scandinavian descent from Norway and Sweden. The other trades colloquially referred to them as square heads. Technically, square heads are called brachycephalic, which means that the head is as wide as it is long similar to a box. The bust on the left is perfect example of a famous square head. Rather than square, some European designs are dolichocephalic. Dolichocephalic heads have relatively longer bases and narrower widths.
Many years ago when I was a young boy, the carpenter’s union was mostly comprised of men of Scandinavian descent from Norway and Sweden. The other trades colloquially referred to them as square heads. Technically, square heads are called brachycephalic, which means that the head is as wide as it is long similar to a box. The bust on the left is perfect example of a famous square head. Rather than square, some European designs are dolichocephalic. Dolichocephalic heads have relatively longer bases and narrower widths.In contrast to Asian designs, European skulls are also prognathic. Prognathic means protruding jaws. In Europeans skulls, the muzzle which contains the nose and jaw protrudes out from the face. In round Asian skulls the jaws and nose are in line with the face. Interestingly, northern Europeans have a much higher incidence of multiple sclerosis than Asians. On the other hand Asians get a variant form of MS called Devic’s disease. In addition, African-Americans also have a low incidence of MS but likewise get a particularly aggressive form of Devic’s disease.

If you strip away the flesh the square shape of the European skull becomes more apparent. The perfect replica cast skull on the right was copied with permission from Bone Clones Inc. The most telltale signs that indicate race are in the shape of the eyes and nose. In this case the eye openings are clearly square. Even more characteristic is the triangular shape of the nose. In Asian and African-American skulls the opening for the eyes and the aperture of the nose are rounder.
The previous post contained a picture of a severely artificially deformed skull. Among other things, the shape of the head affects the pitch and layout of the base of the skull and the venous drainage system of the brain. The length and width of the base of the skull affects the position of the brain within the cranial vault.
A short length in the base from the front to the back of the cranial vault, predisposes the brain to crowding and a condition called Chiari malformations in which the cerebellum or brainstem gets pushed down into the foramen magnum. Chiari malformations can block both venous blood and cerebrospinal fluid (CSF) pathways causing CCSVI and hydrocephalus type conditions. Chiari malformations used to be considered a childhood problem for the most part. Recently, however, studies show that trauma can cause Chiari malformations in adults. What’s more, Chiari malformations have also been associated with multiple sclerosis.
 The graphic of the skull on the left shows the relative size of the large head compared to the relatively small human neck. In the ape the head is small and the neck is large. The body is also supported by four extremities and the head is much closer to the ground so slips and falls are less likely and the distance to the ground is much closer.
The graphic of the skull on the left shows the relative size of the large head compared to the relatively small human neck. In the ape the head is small and the neck is large. The body is also supported by four extremities and the head is much closer to the ground so slips and falls are less likely and the distance to the ground is much closer.Humans on the other hand are tall and top-heavy and standing upright and balanced over a narrow base rooted in the feet is actually quite a feat. Upright posture makes it easier to fall and unfortunately in humans, the head has a further distance to the ground and so falls generate more force.
People living in northern climates are exposed to far more winter related whiplash type traumas than people living in southern climates. Motor vehicle accidents and winter sports and activities such as hockey, skiing and snow mobiles significantly increase the risk and the forces involved in trauma.
When it comes to MS and trauma, it’s not so much the size of the head that matters as it is how it stacks up on the cervical spine. Moreover, it is also how the brain stacks up over the large hole in the base of the skull called the foramen magnum. Brachycephalic, Asian and African designs, as well as skulls with short lengths in their base are more balanced on top of the cervical spine. On the other hand, they stack more of the brainstem over the foramen magnum. This predisposes the brainstem and cerebellum to getting pushed down, or sinking into the foramen in a Chiari malformation and or pressure conus type condition.
In brief, racial differences in the design of the skull may account for the higher incidence of classic multiple sclerosis seen in northern Europeans. It may further explain why Asian and African-Americans have a lower incidence of MS but get a more severe variant form called Devic’s disease also know as neuromyelitis optica (NMO). In the next post I will cover Asian and African-American skull designs.
For additional information on this and related topics visit my website at http://www.upright-health.com.
Skull Design and CCVBP
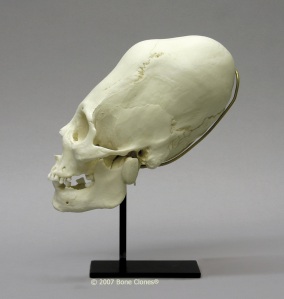 The picture on the left is a life-like cast of an artificially deformed skull from the former indigenous people of Peru. Permission to use the picture was granted by Bone Clones. I began my research into role of venous drainage problems in neurodegenerative diseases of the brain and cord about thirty years ago while studying an artificially deformed crania nearly identical to the one on the above. In addition to upper cervical strains, certain designs and deformation of the skull can affect the drainage system of the brain.
The picture on the left is a life-like cast of an artificially deformed skull from the former indigenous people of Peru. Permission to use the picture was granted by Bone Clones. I began my research into role of venous drainage problems in neurodegenerative diseases of the brain and cord about thirty years ago while studying an artificially deformed crania nearly identical to the one on the above. In addition to upper cervical strains, certain designs and deformation of the skull can affect the drainage system of the brain.No one knows exactly why the former people of Peru and Bolivia chose to intentionally deform a child’s skull, but they did it to quite a few them. I won’t elaborate on all the different theories as to why they did it, nor will I offer my own theory at this time. For now, suffice it to say, what caught my attention was the altered shapes and open state of the special joints that link the bones of the cranial vault together called sutures. The sutures were so named by early anatomists because they are typically shaped like stitches. In contrast to stitches, if you click on the image you will see the sutures in the rear are smooth and open and don’t look like the usual stitch shapes. What’s more, this person was old enough that the sutures should have started to close on the inside.

In this case the severe deformation caused a change in the normal pitch and layout of the drainage system of the brain, including the dipolic veins. As you recall from previous posts, the diploic veins of the skull are located between the inner and outer layer of the skull bones. (See the picture above.)
The shapes of the sutures are actually similar to a seismic recording of fluid mechanics in the brain etched into the shapes of the bones. In the case of the artificially deformed skulls, the change in the shape of the skull caused chronic craniocervical venous back pressure and increased venous pressure in the diploic veins inside the diploe causing the sutures to stay open and altering their shapes.
There was still a hitch though. Except in some rare pathologies, the sutures of most skulls, even those associated with venous drainage problems, start to close on the inside regardless of whether or not they stayed open on the outside.
In some of the artificially deformed skulls, as in the example above, they were open all the way through and not even close to uniting. That suggested to me, that in addition to venous drainage problems, design problems and deformation of the of the skull can cause an increase in pressure inside the skull, called intracranial pressure (ICP). Aside from tumors and strokes, hydrocephalus in children causes an increase in the volume of CSF and ICP, which causes the sutures to stay open.
CSF flow as you recall flows from the ventricles in the core of the brain where it is produced, to the superior sagittal sinus vein at the top of the skull where it mixes with venous blood to exit the skull. Consequently, an increase in venous pressure in the superior sagittal sinus decreases the CSF pressure gradient, which decreases CSF flow. A decrease in CSF outflow increases CSF volume in the brain. The problem is that when adults get hydrocephalus later in life the sutures are closed so when CSF volume increases then either the brain or blood have got to decrease in volume. In this regard, the brain is more compressible than blood. The closed sutures also keep a cap on ICP similar to a counter-weight on a pressure cooker. Consequently, in contrast to children adults get low or normal pressure hydrocephalus (NPH).
The above skull shows how gross deformation of the skull can affect the venous drainage system. There are many different types of normal and pathological variations in the design of the skull, as well as different types of strains and deformation of the skull and spine. Some problems we inherit, others are acquired through disease, aging and injuries. Some are clearly visible, others are not so easily seen or recognized. One thing is becoming readily clear with modern MR angiograms, venograms and cine MR however; that is, strains and deformation of the upper cervical spine and base of the skull can cause chronic venous back pressure (edema), decreased arterial blood flow (ischemia) and decreased CSF flow, which has been linked to NPH, Alzheimer’s and Parkinson’s disease.
For more information on this and related topics visit my website at http://www.upright-health.com
Posted in Alzheimer's, ccsvi, multiple sclerosis, Parkinson's, physical anthropology 1 Comment
Cervical Subluxations and CCVBP
 In a previous post I discussed the role of the vertebral veins, also knowns as the vertebral venous plexus (VVP), in causing chronic craniocervical venous back pressure (CCVBP) and subsequent neurodegenerative conditions and diseases such as multiple sclerosis. Like CCSVI, CCVBP can lead to chronic venous backups and edema in the brain. It can also affect cerebrospinal fluid (CSF) pressure gradients and subsequent flow and volume. Correct CSF volume is essential to brain cushioning, protection and support. Consequently, in addition to MS, CCVBP may play a role in normal pressure hydrocephalus (NPH), which has been associated with Parkinson’s and Alzheimer’s disease.
In a previous post I discussed the role of the vertebral veins, also knowns as the vertebral venous plexus (VVP), in causing chronic craniocervical venous back pressure (CCVBP) and subsequent neurodegenerative conditions and diseases such as multiple sclerosis. Like CCSVI, CCVBP can lead to chronic venous backups and edema in the brain. It can also affect cerebrospinal fluid (CSF) pressure gradients and subsequent flow and volume. Correct CSF volume is essential to brain cushioning, protection and support. Consequently, in addition to MS, CCVBP may play a role in normal pressure hydrocephalus (NPH), which has been associated with Parkinson’s and Alzheimer’s disease.I next discussed the vertebral-basilar arterial supply to the brain and its likely role in chronic ischemia which, like chronic edema from backed up veins, is one of the main suspects in demyelination and other neurodegenerative conditions and subsequent diseases. Lastly, I posted pictures of the tight neurovascular tunnels the VVP and vertebral-basilar arteries must pass through in the upper cervical spine and foramen magnum in the base of the skull on its way to the motherboard of the brain, the brainstem.
 In light of the above, the picture below on the right is of Greek techno music producer, CostumeNational of fightforccsvi.com. The picture was taken with his permission from Dr. Scalfani’s MS website forum called, ThisIsMS.com.
In light of the above, the picture below on the right is of Greek techno music producer, CostumeNational of fightforccsvi.com. The picture was taken with his permission from Dr. Scalfani’s MS website forum called, ThisIsMS.com.The forum is a wonderful group of MS patients who have provided me with a rare opportunity and unbelievable insight into the mystery of MS that they openly and gladly share. Weakened by their condition, they are nonetheless strong and quite fiery in spirit. Together they have formed a formidable group that is shaking up scientists and researchers around the world. Their determined efforts are helping lead the way and shape future research not only for solving MS, but other devastating neurodegenerative conditions as well, such as Alzheimer’s and Parkinson’s disease, NPH, Huntington’s chorea, ALS, PLS and others too numerous to mention here. It is invaluable, to say the least, to have so many cases to study and follow in one location. They provide a wealth of information that demands further retrospective analysis and investigation, such as I am in the process of doing, but on a much larger scale.
This particular type of picture is called an open mouth odontoid image because
 the odontoid process of the second cervical vertebra, called axis or C2, is in the center of the image. It’s called the odontoid process because it looks like a tooth that sticks straight up from the body of the vertebra.
the odontoid process of the second cervical vertebra, called axis or C2, is in the center of the image. It’s called the odontoid process because it looks like a tooth that sticks straight up from the body of the vertebra.The odontoid process fits neatly into a notch in its mate directly above called Atlas or C1 beneath the base of the skull. The odontoid process permits greater pivotal action in the upper cervical spine. In my opinion, the odontoid process also reduces the size of the body of the vertebra, which may help to reduce pressure in the area during head and neck movement. The red line indicates the center line of the spine. The triangular dart-like shapes pointing upward are the spinous process of the cervical vertebra. In a normal spine, they should all line up on the red line.
If you look through the open mouth you will see one of the darts is way off to one side. You will note by the marker on the film that it indicates the right side. That particular dart is the spinous process of the second cervical vertebra (C2) called axis. The degree of misalignment in this case is severe.
According to CostumeNational, about eight years ago, he was riding a motorcycle when he crashed into a car, which threw him to the ground landing on the right side of his shoulder and head. The force of the fall from the weight of his propelled body magnified by the speed he was traveling at severely snapped his neck to the left and left him unconscious.
As the x-ray evidence clearly shows, when he came to later in the hospital, although no one knew it at the time, his head and neck were no longer aligned properly. Instead it remained in the wicked tilt to the left the same as it was after impact. Eight years later he started to develop optic neuritis in his left eye on the low side of the head tilt. Head tilts cause the brain, blood and CSF inside the cranial vault to shift to the low side just like water in a glass, which can increase pressure on the optic nerve and may play a role in optic neuritis.
Interestingly, he had no lesions in the brain but he did show a hyperintensity signal precisely at the location of the kink in the upper cervical spine. The highly suspicious, characteristic symptom of optic neuritis was next followed by cerebral, as well as cord signs and symptoms identical to MS. Nonetheless, without brain lesions, his case falls into the uncertain category of cracks, a no-man’s land not considered to be classic MS.
There is a major principle in neurology when it comes to the brain and the cranial vault, called the Monroe-Kellie principle. According to the Monroe-Kellie principle there are essentially three elements inside the cranial vault which include the brain, blood and CSF. Since the cranial vault is a closed container for the most part, if the volume of one of the elements increases, then one or both of the other two elements must decrease in volume. A brain tumor for example can compress blood and CSF vessels as can Chiari malformations mentioned in previous posts. Likewise, an increase in blood or CSF volume can compress the brain.
The same principle holds true for the spine and spinal canal, which, like the cranial vault, is for the most part a closed container. In other words, there is no free space inside the spinal canal. Instead, the space between the inside walls of the spinal canal and the cord is filled with the VVP. Therefore a kink in the upper cervical spinal canal as in the case above puts a kink in the drainage system of the brain and cord. It also causes venous back pressure and hypertension around the cord. Lastly, it increases resistance to CSF flow on its way back to the brain from the cord.
In my next post I will discuss precision line analysis used by upper cervical chiropractors to analyze mechanical strains such as the one above. After that we will then look at some of the common signs and symptoms of MS which share a lot in common with AD and PD.
For additional information on this and related topics visit my website at http://www.upright-health.com.
Chronic Ischemia and MS Lesions
According to Schelling venous back jets into the brain and shear stresses in the cord combined with cerebrospinal fluid reflux are likely causes of demyelination. Other researchers have suggested that chronic edema and normal pressure hydrocephalus can damage myelin simply by stretching it. Zamboni suggests that venous drainage problems lead to iron accumulation, which initiates neurodegenerative processes. There is still another theory that suggests that demyelination may be due to chronic ischemia, that is, decreased blood flow to the brain and cord. For now, I will focus on the blood supply to the brain and ignore the cord.
As depicted in the picture above, blood is delivered to the brain via the anterior and posterior blood supply routes. The anterior blood supply routes are the internal carotid arteries. They are called anterior because they are in the front of the neck. The posterior blood supply routes are the vertebral-basilar arteries in the back of the neck. The carotid arteries travel along either side of the trachea (windpipe) and enter the brain through an opening in the base of the skull called the foramen lacerum where it passes through the cavernous sinus of the drainage system of the brain. (Click on any picture to enlarge it and get a closer view).
As shown in the picture above, the vertebral arteries pass through holes in the transverse processes of the cervical spine. They exit the spine at the first cervical vertebra and enter into a memebrane between the base of the skull and the first cervical vertebra. The membrane is called the suboccipital cavernous sinus or atlantooccipital membrane as seen in the picture on the right.
After traveling through the suboccipital cavernous sinus for a short distance the vertebral arteries turn in and head upward. They next pass through the foramen magnum as shown in the picture on the left. Shortly after passing through the foramen magnum the vertebal arteries unite to become the basilar artery. Before uniting the vertebral artery gives off two branches. One is called the posterior inferior cerebellar artery because it supplies the lower rear aspect of the cerebellum. The other artery is called the anterior spinal artery.
The two anterior spinal arteries then unite and head back down through the foramen magnum to supply the entire length of the anterior aspect of the spinal cord. Another artery called the posterior spinal artery branches off either the posterior inferior cerebellar arteries or the anterior spinal arteries to become the posterior spinal artery. The posterior spinal artery supplies the posterior aspect of the entire length of the cord. The cord also gets its blood supply from what are called radicular arteries. For now we will overlook the possible role of the anterior and posterior spinal arteries in chronic ischemia of the spinal cord and focus on the vertebral-basilar arteries and ischemia of the brain. In brief, chronic ischemia of the cord may play a role in amyotrophic lateral sclerosis and primary lateral sclerosis.
The vertebral-basilar arteries supply most of the the motherboard of the brain, which is the brainstem and cerebellum. Except for the nose and eyes it also supplies all the cranial nerves, which control the muscles and senses of the head and neck down to the shoulders, as well as autonomic function of the internal organs via the vagus cranial nerve. In this regard, the vertebral-basilar arteries also supply the hypothalamus, which is the control center for autonomic vegetative functions in the body, and the thalamus, which is the sensory switchboard or router of the brain.
In additon to the brainstem and cerebellum, the vertebral-basilar arteries supply the inner parts of the temporal, and the inner parts and rear pole of the occipital lobes of the brain. Among other things, the inner temporal lobe is important to memory. The occipital lobe is important for interpreting visual signals which is likewise dependant upon memory.
The areas located at the tail ends of the anterior and posterior blood supply routes are called the watershed areas of the brain. The watershed areas of the brain are the weakest point in the blood supply routes and oftentimes are the ones most affected by decreases in blood flow. Like the brain the cord also has watershed areas which I will leave out of this discussion. One of the watershed areas in the brain is around the periventricular areas where MS lesions are often found. Alzhiemer’s and migraine headaches also have a predilection for periventricular white matter lesions. Many researchers believe that the white matter lesions in MS, migraines and Alzheimer’s disease are caused by chronic ishemia.
While the lesions are typically found higher up in the brain above the covering over the cerebellum, many of the symptoms associated with MS come from cranial nerves supplied by the vertebral-basilar arteries. Symptoms such as dizziness and fatigue are mostly likely signs of ischemia. Likewise, the lesions seen in certain cases of MS, especially those associated with migranous symptoms are most likely caused by chronic ischemia. In addition, the vertebral-basilar arteries are the ones most commonly involved in ministrokes called transient ischemic attacks. The design of the skull, spine and circulatory system of the brain predisposes humans to upper cervical strains and subsequent compression and back pressure against the posterior blood supply routes, which are the vertebral-basilar arteries. The outcome is chronic ischemia in the areas of the brain they supply.
In my next post I will discuss upper cervical strains and deformation of neurovascular tunnels. Upper cervical strains and deformation of critical neurovascular tunnels are most likely one of the major causes of chronic ischemia and edema in the brain. They may also play a role in normal pressure hydrocephalus, but that’s an entirely different story more related to Parkinson’s and Alzheimer’s disease.
For additional information on this and related topics visit my website at http://www.upright-health.com.
As depicted in the picture above, blood is delivered to the brain via the anterior and posterior blood supply routes. The anterior blood supply routes are the internal carotid arteries. They are called anterior because they are in the front of the neck. The posterior blood supply routes are the vertebral-basilar arteries in the back of the neck. The carotid arteries travel along either side of the trachea (windpipe) and enter the brain through an opening in the base of the skull called the foramen lacerum where it passes through the cavernous sinus of the drainage system of the brain. (Click on any picture to enlarge it and get a closer view).
As shown in the picture above, the vertebral arteries pass through holes in the transverse processes of the cervical spine. They exit the spine at the first cervical vertebra and enter into a memebrane between the base of the skull and the first cervical vertebra. The membrane is called the suboccipital cavernous sinus or atlantooccipital membrane as seen in the picture on the right.
After traveling through the suboccipital cavernous sinus for a short distance the vertebral arteries turn in and head upward. They next pass through the foramen magnum as shown in the picture on the left. Shortly after passing through the foramen magnum the vertebal arteries unite to become the basilar artery. Before uniting the vertebral artery gives off two branches. One is called the posterior inferior cerebellar artery because it supplies the lower rear aspect of the cerebellum. The other artery is called the anterior spinal artery.
The two anterior spinal arteries then unite and head back down through the foramen magnum to supply the entire length of the anterior aspect of the spinal cord. Another artery called the posterior spinal artery branches off either the posterior inferior cerebellar arteries or the anterior spinal arteries to become the posterior spinal artery. The posterior spinal artery supplies the posterior aspect of the entire length of the cord. The cord also gets its blood supply from what are called radicular arteries. For now we will overlook the possible role of the anterior and posterior spinal arteries in chronic ischemia of the spinal cord and focus on the vertebral-basilar arteries and ischemia of the brain. In brief, chronic ischemia of the cord may play a role in amyotrophic lateral sclerosis and primary lateral sclerosis.
The vertebral-basilar arteries supply most of the the motherboard of the brain, which is the brainstem and cerebellum. Except for the nose and eyes it also supplies all the cranial nerves, which control the muscles and senses of the head and neck down to the shoulders, as well as autonomic function of the internal organs via the vagus cranial nerve. In this regard, the vertebral-basilar arteries also supply the hypothalamus, which is the control center for autonomic vegetative functions in the body, and the thalamus, which is the sensory switchboard or router of the brain.
In additon to the brainstem and cerebellum, the vertebral-basilar arteries supply the inner parts of the temporal, and the inner parts and rear pole of the occipital lobes of the brain. Among other things, the inner temporal lobe is important to memory. The occipital lobe is important for interpreting visual signals which is likewise dependant upon memory.
The areas located at the tail ends of the anterior and posterior blood supply routes are called the watershed areas of the brain. The watershed areas of the brain are the weakest point in the blood supply routes and oftentimes are the ones most affected by decreases in blood flow. Like the brain the cord also has watershed areas which I will leave out of this discussion. One of the watershed areas in the brain is around the periventricular areas where MS lesions are often found. Alzhiemer’s and migraine headaches also have a predilection for periventricular white matter lesions. Many researchers believe that the white matter lesions in MS, migraines and Alzheimer’s disease are caused by chronic ishemia.
While the lesions are typically found higher up in the brain above the covering over the cerebellum, many of the symptoms associated with MS come from cranial nerves supplied by the vertebral-basilar arteries. Symptoms such as dizziness and fatigue are mostly likely signs of ischemia. Likewise, the lesions seen in certain cases of MS, especially those associated with migranous symptoms are most likely caused by chronic ischemia. In addition, the vertebral-basilar arteries are the ones most commonly involved in ministrokes called transient ischemic attacks. The design of the skull, spine and circulatory system of the brain predisposes humans to upper cervical strains and subsequent compression and back pressure against the posterior blood supply routes, which are the vertebral-basilar arteries. The outcome is chronic ischemia in the areas of the brain they supply.
In my next post I will discuss upper cervical strains and deformation of neurovascular tunnels. Upper cervical strains and deformation of critical neurovascular tunnels are most likely one of the major causes of chronic ischemia and edema in the brain. They may also play a role in normal pressure hydrocephalus, but that’s an entirely different story more related to Parkinson’s and Alzheimer’s disease.
For additional information on this and related topics visit my website at http://www.upright-health.com.
MS Lesions of the Cervical Cord
Multiple Sclerosis is technically a neurodegenerative disease of the brain. Classically MS is associated with two or more supratentorial (above the covering over the cerebellum) periventricular hyperintensity signals. The lesions are the white spots on the brain scan on the right. The large shadows in the middle of the brain shaped like a butterfly are the lateral ventricles. The periventricular area surrounds the ventricles. In addition to the brain, however, some MS patients also get lesions in the cervical cord.
Demyelinating type lesions in the cervical cord without lesions in the brain are not considered to be classic signs of MS. Lesions below the cervical cord are, likewise, not considered to be MS. Instead they are given different names.In this post I will stick to MS lesions in the cervical cord and disregard lesions of the lower cord such as those seen in amyotrophic lateral sclerosis (ALS), primary lateral sclerosis, Devic’s Disease (neuromyelitis optica) and others. I will also ignore the lesions sometimes associated scoliosis and abnormal curvatures of the spine.
 According to Schelling, the lesions seen in the cervical cord in MS are due to stretch and shear stress. Many types of trauma, such as whiplash in the picture on the left, cause hyperflexion and hyperextension of the spine. The strain can occur in a front to back motion or from side to side. At the same time, whiplash type traumas also strain the spinal cord inside the spinal canal.
According to Schelling, the lesions seen in the cervical cord in MS are due to stretch and shear stress. Many types of trauma, such as whiplash in the picture on the left, cause hyperflexion and hyperextension of the spine. The strain can occur in a front to back motion or from side to side. At the same time, whiplash type traumas also strain the spinal cord inside the spinal canal.The spinal cord, like the brain has three protective coats called meninges. The outer coat is called the dura mater. The middle coat is called the subarachnoid mater and the inner coat is called the pia mater. Except for the attachment of the tail end of the cord, called the filum terminale, to the tail bone, called the coccyx, the spinal cord moves freely, unattached inside the spinal canal.

The three coats are held together by denticulate ligaments that attach the inner pia mater to the outer dura mater at the nerve roots. Click on the image on the right for a closer look. The subarchnoid space lies between the subarchnoid mater and the pia mater and contains a significant volume of cerebrospinal fluid, called CSF. There is also lymph like fluid that serves as a lubricant between the outer coat of the dura mater and the middle coat of the subarachnoid mater. This allows the inner contents of the cord to move somewhat independently to a limited degree.
 According to Schelling, mechanical strains of the spine can take the cord to extreme limits of stretch. It can also cause shear stress within the cord between the pia mater on the inside and the dura mater on the outside. The stress points occur at the attachment of the denticulate ligament. Furthermore, violent back jets of CSF in the subarachnoid space amplify the strain like a boat moored to a dock hit by hurricane force waves. The waves amplify the strain and rip the ropes and boats from their moorings. Similarly, violent waves of CSF flowing through the subarachnoid space amplify the strain acting on the denticulate ligaments. When they reach a critical threshold, engineer’s call the yeild point, the denticulate connective tissue attachments of the pia mater to the dura mater will tear. The strained tissues of the pia mater further damage the meylinated nerve tracts they cover. Click on the image above to get a closer look. This is a cross section of the cord and shows the inside. The H shape in the middle of the cord is the grey matter. The myelinated white fiber tracts surround it. The blue area is the subarachnoid space which contains CSF.
According to Schelling, mechanical strains of the spine can take the cord to extreme limits of stretch. It can also cause shear stress within the cord between the pia mater on the inside and the dura mater on the outside. The stress points occur at the attachment of the denticulate ligament. Furthermore, violent back jets of CSF in the subarachnoid space amplify the strain like a boat moored to a dock hit by hurricane force waves. The waves amplify the strain and rip the ropes and boats from their moorings. Similarly, violent waves of CSF flowing through the subarachnoid space amplify the strain acting on the denticulate ligaments. When they reach a critical threshold, engineer’s call the yeild point, the denticulate connective tissue attachments of the pia mater to the dura mater will tear. The strained tissues of the pia mater further damage the meylinated nerve tracts they cover. Click on the image above to get a closer look. This is a cross section of the cord and shows the inside. The H shape in the middle of the cord is the grey matter. The myelinated white fiber tracts surround it. The blue area is the subarachnoid space which contains CSF.
The lesions seen in the cervical cord are micro tears in the meninges and nearby myelinated nerve pathways . The tears cause scars to form called sclerotic plaques. Because they occur on the outside along the flanks of the cord, the tears tend to effect the outside structures of the cord.
The outside of the cord (see picture to left)contains the long myelinated high speed primary nerve pathways of the central nervous system. Primary nerves go from the brain to particular destination levels in the cord. The long white tracts on the outside of the cord contain both sensory nerves for detecting sensations related to the environment, muscle tone and balance, and motor nerves for running the muscles. Tears in the area of the denticulate ligaments thus affect nearby myelinated nerves in the cord resulting in muscle weakness and warped sensations called paresthesias.
In brief, according to Schelling, one of the likely causes of the lesions of multiple sclerosis seen in the brain are due to violent venous back jets associated with trauma. The lesions seen in the cervical cord are due to severe overstretching and shear stresses within the cord itself magnified by hydraulic stress from CSF waves. There is still more to the story, however, that needs further exploration and explanation. That’s where my theory may help to fill in some of the missing pieces to the puzzle.
My theory is that craniocervical syndromes can cause chronic edema (swelling), ischemia (decreased blood flow) and NPH (normal pressure hydrocephalus) conditions in the brain. Similar events can occur in the cord due to abnormal conditions of the spine. These chronic conditions can, in turn initiate neurodegenerative processes such as the glutamate cascade, which follows strokes.
In my next post I will discuss the posterior blood supply routes to the brain and circulation to the cord. The veins are not the only problem in MS. The arteries are a big part of the problem as well. In addition to MS, I suspect that certain cases of sclerosis of the long myelin tracts of the lower cord, such as ALS and PLS are probably due more to chronic ischemia. This is probably why lesions sometimes also show up in cases of abnormal curvatures of the spine such as scoliosis and kyphosis. Oxidative stress and chronic ischemia are chief suspects in the cause of demyelination and the shape of the spine, and thus the spinal canal, affect arterial and venous blood flow in the cord.
For additional information on this and related topics visit my website at http://www.upright-health.com.
Pressure and Shear Stress in MS Lesions
According to Schelling one of the likely causes of MS lesions is venous back jets into the brain. He proposes that one of the possible sources arises from normal cardiorespiratory waves. The other is from trauma. In either case venous blood flows backwards and into the brain.
One route of venous back jets into the brain is through the jugular veins. Schelling proposes that certain people are born with or acquire incompetent valves in the jugulars that fail to check the reverse flows. The other route is through the vertebral veins which have no valves to prevent reverse flows. In the picture above, the jugular veins are the large veins in the front of the neck. The vertebral veins are the smaller veins in the back of the neck. The large veins inside the skull are called dural sinuses.
 Typically most, but not all veins have valves to check and prevent back flow. Technically speaking none of the dural sinuses have valves. The alignment of some of the cerebral veins however serves to prevent reverse flows to a limited degree, which I won’t go into here. Disregarding that little piece of not so trivial information, the large veins of the brain basically have no valves.
Typically most, but not all veins have valves to check and prevent back flow. Technically speaking none of the dural sinuses have valves. The alignment of some of the cerebral veins however serves to prevent reverse flows to a limited degree, which I won’t go into here. Disregarding that little piece of not so trivial information, the large veins of the brain basically have no valves.
If you click on the image and enlarge it you will find little boxes with the names of the veins as you mouse over them. Following the veins backwards, upstream and counter current to normal flow, the jugular and vertebral veins next connect to the sigmoid sinus, the S shaped sinus directly above them. The transverse sinus is the short flat sinus that runs from the sigmoid sinus to the back of the skull. At that small circular junction at the back of the skull is another sinus that runs forty-five degrees upward and toward the middle of the brain. It’s called the straight sinus. Going straight up, beyond the junction of the transverse and straight sinus is the largest sinus of the brain that runs up to the top of the brain. It’s called the superior sagittal sinus. The superior cerebral veins attach to it. As an aside, these are the veins mentioned above that attach to the superior sagittal sinus at angles counter current to blood flow. It has been suggested that their angle of attachment may serve as a semi valve-like mechanism.
Now if you follow the straight sinus inward you will see it connects to the Great Vein of Galen, the Basal Vein of Rosenthal and the internal cerebral veins. These veins all drain the core of the brain. More importantly, regarding this discussion they go to the periventricular areas of the brain. If you click on the picture and enlarge it once more, you will see a large shadow in the middle of the brain. The shadow you see is the lateral ventricle. The ventricles of the brain produce and are filled with cerebrospinal fluid (CSF) which is made mostly of water. CSF cushions, protects and supports the brain. If you look down by the vertebral veins you will see another shadow. That shadow is the spinal cord. Among other things it contains the subarachnoid space surrounding the cord, which is likewise filled with CSF. The subarachnoid space is part of the protective covering of the brain and cord called meninges. The ventricles, subarachnoid space and CSF pathways likewise have no valves. In contrast to being inside the cord, the vertebral veins surround the cord inside the spinal canal.
I would like to put aside cardiorespiratory waves, which I disagree with as a source of injury to the brain, and focus on trauma. In contrast to relatively mild normal cardiorespiratory waves, trauma produces massive uncontrolled forces that can reflux into the brain under significant pressure. In this regard, the vertebral veins contain a large volume of unchecked blood. The subarachnoid spaces at the lumbar cistern of the cord also contain a significant volume of unchecked CSF. Lastly, the valves of the jugular veins have physical limitations which may be easily overwhelmed by massive forces.
 According to Schelling venous back jets and massive refluxes from trauma simply follow the course of the dural sinuses. It makes sense then that the lesions in MS tend to show up around the largest veins in the brain and get progressively smaller as you follow the veins upstream counter-current to flow. MS lesions also tend to show up in the periventricular areas, which, as mentioned above, drain into the straight sinus system. The ventricles are depicted in red in the sketch to the left.
According to Schelling venous back jets and massive refluxes from trauma simply follow the course of the dural sinuses. It makes sense then that the lesions in MS tend to show up around the largest veins in the brain and get progressively smaller as you follow the veins upstream counter-current to flow. MS lesions also tend to show up in the periventricular areas, which, as mentioned above, drain into the straight sinus system. The ventricles are depicted in red in the sketch to the left.
In other words venous blood back jets into the brain and stretches the largest veins of the brain that take the brunt of the crushing force, causing them to balloon out and strain nearby surrounding myelinated nerves. Researchers studying normal pressure hydrocephalus surmized many years ago that stretching from something as simple as edema alone was enough to break myelin. Basically speaking, myelin, is simply no match for the massive forces generated by whiplash and other similar severe type traumas. Trauma can generate significant pressure in the veins of the entire body never mind the brain. What’s more, pressure associated with trauma often causes rapid, acute rises in surrounding tissue pressures.
In contrast to trauma, normal inversion and Valsalva maneuvers cause reverse flows into the brain. Hanging upside down or standing on your head causes inversion flows. A Valsalva maneuver is performed by blowing real hard against maximum resistance. Pilots and scuba divers use Valsalva maneuvers to control pressure in the brain and ears respectively. The famous trumpet player “Satchmo” Louis Armstrong performed Valsalva maneuvers when he played long powerful high sustained notes. His neck and facial veins would buldge and his eyes would literally pop out. Technically speaking, he should have blown his cork before middle age if inversion flows were a problem. Instead he lived a good and long life. Additionally, Olympic style competition weight lifters do Valsalva maneuvers when they lift heavy weights. In this regard, Valsalva maneuvers are beneficial in that they help shore up, stabilize and strengthen the spine.
 In light of inversion flows and Valsalva maneuvers, I decided decades ago to study bats, whales and giraffes because of the extreme inversion flows they face during head inversion and deep dives. It turned out to be a great idea. As I expected, these mammals appear to have developed compensatory mechanisms. Based on my studies, it is my opinion that giraffes use the extra large spaces inside their skull called diploe as a drip pan to catch blood that has been rerouted during head inversion. I discussed the diploe in humans and their role in brain cooling in previous posts.
In light of inversion flows and Valsalva maneuvers, I decided decades ago to study bats, whales and giraffes because of the extreme inversion flows they face during head inversion and deep dives. It turned out to be a great idea. As I expected, these mammals appear to have developed compensatory mechanisms. Based on my studies, it is my opinion that giraffes use the extra large spaces inside their skull called diploe as a drip pan to catch blood that has been rerouted during head inversion. I discussed the diploe in humans and their role in brain cooling in previous posts.
This extra large rather handsome looking giraffe with the beautiful bedroom eyes and full sensous lips, also has a particularly distguished prominent bump over the paranasal bones of the nose. I believe that large giraffes use these extra special, strategically located bumps, called accessory horns, to further increase the capacity of the accessory drainage system of the diploe during head inversion. The challenge for humans is just the opposite. Humans developed compensatory mechanisms to contend with upright posture. Interestingly, the valveless veins of the skull and spine appear to play similar roles in all the mammals mentioned above. What is even more fascinating is that humans and whales use the vertebral veins to stabilize intracranial pressure (ICP) and fluid mechanics in the brain but in completely opposite ways. In brief, moderate inversion flows don’t appear to be the problem. On the other hand, acute venous back jets are an entirely different story.
Unfortunately, back jets don’t explain the full story behind the lesions you find in the cord. Again, that’s where Schelling’s theory makes the most sense. I will discuss cord lesions in MS in my next post. In contrast to massive pressure from venous back jets that stretch nearby myelin in the brain, according to Schelling the myelin in the cord simply snaps due to shear forces acting on attachment points inside the cord itself. Those shear forces are amplified by a Tsunami of CSF waves flowing backwards through the subarchnoid space of the cord.
For additional information on this and related topics visit my website at http://www.upright-health.com.
One route of venous back jets into the brain is through the jugular veins. Schelling proposes that certain people are born with or acquire incompetent valves in the jugulars that fail to check the reverse flows. The other route is through the vertebral veins which have no valves to prevent reverse flows. In the picture above, the jugular veins are the large veins in the front of the neck. The vertebral veins are the smaller veins in the back of the neck. The large veins inside the skull are called dural sinuses.
 Typically most, but not all veins have valves to check and prevent back flow. Technically speaking none of the dural sinuses have valves. The alignment of some of the cerebral veins however serves to prevent reverse flows to a limited degree, which I won’t go into here. Disregarding that little piece of not so trivial information, the large veins of the brain basically have no valves.
Typically most, but not all veins have valves to check and prevent back flow. Technically speaking none of the dural sinuses have valves. The alignment of some of the cerebral veins however serves to prevent reverse flows to a limited degree, which I won’t go into here. Disregarding that little piece of not so trivial information, the large veins of the brain basically have no valves.If you click on the image and enlarge it you will find little boxes with the names of the veins as you mouse over them. Following the veins backwards, upstream and counter current to normal flow, the jugular and vertebral veins next connect to the sigmoid sinus, the S shaped sinus directly above them. The transverse sinus is the short flat sinus that runs from the sigmoid sinus to the back of the skull. At that small circular junction at the back of the skull is another sinus that runs forty-five degrees upward and toward the middle of the brain. It’s called the straight sinus. Going straight up, beyond the junction of the transverse and straight sinus is the largest sinus of the brain that runs up to the top of the brain. It’s called the superior sagittal sinus. The superior cerebral veins attach to it. As an aside, these are the veins mentioned above that attach to the superior sagittal sinus at angles counter current to blood flow. It has been suggested that their angle of attachment may serve as a semi valve-like mechanism.
Now if you follow the straight sinus inward you will see it connects to the Great Vein of Galen, the Basal Vein of Rosenthal and the internal cerebral veins. These veins all drain the core of the brain. More importantly, regarding this discussion they go to the periventricular areas of the brain. If you click on the picture and enlarge it once more, you will see a large shadow in the middle of the brain. The shadow you see is the lateral ventricle. The ventricles of the brain produce and are filled with cerebrospinal fluid (CSF) which is made mostly of water. CSF cushions, protects and supports the brain. If you look down by the vertebral veins you will see another shadow. That shadow is the spinal cord. Among other things it contains the subarachnoid space surrounding the cord, which is likewise filled with CSF. The subarachnoid space is part of the protective covering of the brain and cord called meninges. The ventricles, subarachnoid space and CSF pathways likewise have no valves. In contrast to being inside the cord, the vertebral veins surround the cord inside the spinal canal.
I would like to put aside cardiorespiratory waves, which I disagree with as a source of injury to the brain, and focus on trauma. In contrast to relatively mild normal cardiorespiratory waves, trauma produces massive uncontrolled forces that can reflux into the brain under significant pressure. In this regard, the vertebral veins contain a large volume of unchecked blood. The subarachnoid spaces at the lumbar cistern of the cord also contain a significant volume of unchecked CSF. Lastly, the valves of the jugular veins have physical limitations which may be easily overwhelmed by massive forces.
 According to Schelling venous back jets and massive refluxes from trauma simply follow the course of the dural sinuses. It makes sense then that the lesions in MS tend to show up around the largest veins in the brain and get progressively smaller as you follow the veins upstream counter-current to flow. MS lesions also tend to show up in the periventricular areas, which, as mentioned above, drain into the straight sinus system. The ventricles are depicted in red in the sketch to the left.
According to Schelling venous back jets and massive refluxes from trauma simply follow the course of the dural sinuses. It makes sense then that the lesions in MS tend to show up around the largest veins in the brain and get progressively smaller as you follow the veins upstream counter-current to flow. MS lesions also tend to show up in the periventricular areas, which, as mentioned above, drain into the straight sinus system. The ventricles are depicted in red in the sketch to the left.In other words venous blood back jets into the brain and stretches the largest veins of the brain that take the brunt of the crushing force, causing them to balloon out and strain nearby surrounding myelinated nerves. Researchers studying normal pressure hydrocephalus surmized many years ago that stretching from something as simple as edema alone was enough to break myelin. Basically speaking, myelin, is simply no match for the massive forces generated by whiplash and other similar severe type traumas. Trauma can generate significant pressure in the veins of the entire body never mind the brain. What’s more, pressure associated with trauma often causes rapid, acute rises in surrounding tissue pressures.
In contrast to trauma, normal inversion and Valsalva maneuvers cause reverse flows into the brain. Hanging upside down or standing on your head causes inversion flows. A Valsalva maneuver is performed by blowing real hard against maximum resistance. Pilots and scuba divers use Valsalva maneuvers to control pressure in the brain and ears respectively. The famous trumpet player “Satchmo” Louis Armstrong performed Valsalva maneuvers when he played long powerful high sustained notes. His neck and facial veins would buldge and his eyes would literally pop out. Technically speaking, he should have blown his cork before middle age if inversion flows were a problem. Instead he lived a good and long life. Additionally, Olympic style competition weight lifters do Valsalva maneuvers when they lift heavy weights. In this regard, Valsalva maneuvers are beneficial in that they help shore up, stabilize and strengthen the spine.
 In light of inversion flows and Valsalva maneuvers, I decided decades ago to study bats, whales and giraffes because of the extreme inversion flows they face during head inversion and deep dives. It turned out to be a great idea. As I expected, these mammals appear to have developed compensatory mechanisms. Based on my studies, it is my opinion that giraffes use the extra large spaces inside their skull called diploe as a drip pan to catch blood that has been rerouted during head inversion. I discussed the diploe in humans and their role in brain cooling in previous posts.
In light of inversion flows and Valsalva maneuvers, I decided decades ago to study bats, whales and giraffes because of the extreme inversion flows they face during head inversion and deep dives. It turned out to be a great idea. As I expected, these mammals appear to have developed compensatory mechanisms. Based on my studies, it is my opinion that giraffes use the extra large spaces inside their skull called diploe as a drip pan to catch blood that has been rerouted during head inversion. I discussed the diploe in humans and their role in brain cooling in previous posts.This extra large rather handsome looking giraffe with the beautiful bedroom eyes and full sensous lips, also has a particularly distguished prominent bump over the paranasal bones of the nose. I believe that large giraffes use these extra special, strategically located bumps, called accessory horns, to further increase the capacity of the accessory drainage system of the diploe during head inversion. The challenge for humans is just the opposite. Humans developed compensatory mechanisms to contend with upright posture. Interestingly, the valveless veins of the skull and spine appear to play similar roles in all the mammals mentioned above. What is even more fascinating is that humans and whales use the vertebral veins to stabilize intracranial pressure (ICP) and fluid mechanics in the brain but in completely opposite ways. In brief, moderate inversion flows don’t appear to be the problem. On the other hand, acute venous back jets are an entirely different story.
Unfortunately, back jets don’t explain the full story behind the lesions you find in the cord. Again, that’s where Schelling’s theory makes the most sense. I will discuss cord lesions in MS in my next post. In contrast to massive pressure from venous back jets that stretch nearby myelin in the brain, according to Schelling the myelin in the cord simply snaps due to shear forces acting on attachment points inside the cord itself. Those shear forces are amplified by a Tsunami of CSF waves flowing backwards through the subarchnoid space of the cord.
For additional information on this and related topics visit my website at http://www.upright-health.com.
Posted in ccsvi, demyelination, ms lesions, multiple sclerosis, Uncategorized 9 Comments
The Mystery of MS Lesions
The root of the word sclerosis means scar and multiple sclerosis is associated with multiple scars in the brain. Scars being what they are, it is unlikely that either the best upper cervical chiropractic care or surgical liberation procedure will lead to repair of badly damaged or scarred tissues.
If you read the comments section you will see that many people with MS lesions recall severe trauma from many years earlier. Only in rare cases do the serious symptoms show up immediately or soon after trauma so no one would even think of looking for lesions in the first year or so after the accident. In fact, the interval of time between the traumatic incident and the onset of symptoms and lesions is one of the key issues in the medicolegal debate regarding the relationship between MS and trauma. The other issue is the cause or mechanism of injury. I discuss the medicolegal issue, as well as a pertinent clear cut case or MS related to whiplash in my book.
By the time brain scans are done the scars can be many years old. On the other hand, I had the experience of treating cases where the signs, symptoms and lesions all started to show up in just about a year. Two of those cases were especially severe and resulted in significant disabilities. In any case, most lesions in MS are permanent scars.
Unfortunately, oftentimes the scars are in bad locations as far as signs and symptoms are concerned. For example, the cervical cord contains all of the long myelinated tracts that pass from higher centers in the brain down to the arms and legs to work the muscles. Damage to these long tracts can cause permanent muscle weakness. The goal in these cases should be to restore function and halt further progression and disability as much as possible.
The lesions or scars of multiple sclerosis show up as bright spots called hyperintensity signals on MRI as seen in the brain scan on the right. Hyperintensity signals, however, are not unique to MS. Strokes and migraine headaches can also cause hyperintensity signals on brain scans in the area of impaired arterial blood flow.
called hyperintensity signals on MRI as seen in the brain scan on the right. Hyperintensity signals, however, are not unique to MS. Strokes and migraine headaches can also cause hyperintensity signals on brain scans in the area of impaired arterial blood flow.
MS hyperintensity signals are more characteristically located above the covering over the posterior fossa, which contains the cerebellum as seen in the sketch below. Hence, the covering is called the tentorium cerebelli. MS lesions are typically found in supratentorial areas. Additionally, the hyperintensity signals are often found surrounding the chambers in the core of the brain called ventricles in the periventricular areas. The ventricles are the dark shadows in the brain scan above and chambers in the middle of the brain and brainstem seen in the sketch below.
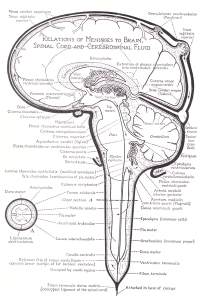 In addition to the supratentorial and periventricular areas, instead of arteries, as in strokes and migraine headaches, the lesions in MS are more typically found in what are called perivenular areas around the larger dural sinuses (veins) of the brain. They also tend to get smaller in number and size as you follow the blood vessels upstream counter-current to blood flow. This is the complete opposite of what you would expect if viruses were the cause because viruses follow blood flow. Consequently, the lesions would tend to show up in areas closer to the source of the stream in the arteries first, not so much further downstream in veins. Considering all the above, it’s hard to picture how stenosis in such distant jugular and thoracic veins could cause lesions to show up predominantly in the higher and core areas of the brain above the tentorium, and not more in the cerebellum, which is down in the basement of the cranial vault called the posterior fossa.
In addition to the supratentorial and periventricular areas, instead of arteries, as in strokes and migraine headaches, the lesions in MS are more typically found in what are called perivenular areas around the larger dural sinuses (veins) of the brain. They also tend to get smaller in number and size as you follow the blood vessels upstream counter-current to blood flow. This is the complete opposite of what you would expect if viruses were the cause because viruses follow blood flow. Consequently, the lesions would tend to show up in areas closer to the source of the stream in the arteries first, not so much further downstream in veins. Considering all the above, it’s hard to picture how stenosis in such distant jugular and thoracic veins could cause lesions to show up predominantly in the higher and core areas of the brain above the tentorium, and not more in the cerebellum, which is down in the basement of the cranial vault called the posterior fossa.
In addition to the brain, MS lesions are sometimes found in the cervical cord as depicted in the old sketch above. In contrast to the core of the brain, lesions in the cord tend to show up on the outside along its flanks which contain the myelinated tracts mentioned above. Rarely ever do MS lesions show up below the shoulders. While MS lesions stop at the shoulders, however, other similar conditions associated with scarring similar to demyelination seen in the cervical cord in MS, are seen in the lower cord, such as amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s disease and primary lateral sclerosis (PLS). A variant of ALS, PLS can reach up into the brain as well. It’s called bulbar ALS. There is also a variant of MS, called Devic’s disease, that is associated with demyelination in the lower cord but optic neuritis in the brain. In addition to MS, I also treated patients with demyelinating diseases of the lower cord. At this time there is nothing anyone can do to stop the devastation in these conditions, but I believe we are getting closer, and a flood of cranked-up highly motivated MS patients are leading the way. When Parkinson’s patients join the fray the pressure will increase three fold, so will the money for further research into venous drainage problems.
Interestingly, while Asians have a lower incidence of MS they do get demyelinating diseases of the cord such as Devic’s disease. I believe it has to do with design differences between Caucasian and Asian skull designs. I will be covering demyelinating diseases of the lower cord on my new website, which is not quite ready for public viewing yet. Suffice it to say that demyelinating diseases of the cord are probably due to similar design problems and circulatory causes found in MS.
As far as the cause and location of the lesions of MS are concerned, Dr. Schelling’s theory makes the most sense. I will be discussing Schelling’s theory as to why the lesions show up where they do in my next post. I will also throw in some of my own two cents to add to the mix and maybe fill in some of the gaps. In brief, I believe that in certain cases of MS the hyperintensity signals and lesions are more likely due to decreased arterial blood flow similar to migraines and mini strokes, not venous drainage problems.
While curing the scars may be difficult or impossible, the location of the scars are often in areas that have nothing to do with many of the unusual signs and symptoms associated with MS, such as optic neuritis, ringing in the ears, trigeminal neuralgia, speech problems, balance problems, fatigue etc. Even more interesting is that, except for the eyes, most of the nerves that would cause such symptoms are found below the tentorium in the posterior fossa. Most of the signs and symptoms associated with Parkinson’s disease likewise come from the posterior fossa. Slowly but surely, trauma is being recognized as a possible causative factor of Parkinson’s just like MS. Furthermore, since the lesions don’t come and go in MS they can’t be the cause of remissions and exacerbations of signs and symptoms. This is a promising fact!
Halting the progression of MS and improving signs and symptoms unrelated to the lesions is definitely possible by restoring fluid mechanics in the brain. Upper cervical correction is one way to do it. The liberation procedure is another. We are on a completely new path but we have only taken the first step. Things can only get better as we learn more and continue to unravel the mystery of MS and the unique design of the incredible human brain due to upright posture. I believe upright MR and angiograms will shed much more light.
If you read the comments section you will see that many people with MS lesions recall severe trauma from many years earlier. Only in rare cases do the serious symptoms show up immediately or soon after trauma so no one would even think of looking for lesions in the first year or so after the accident. In fact, the interval of time between the traumatic incident and the onset of symptoms and lesions is one of the key issues in the medicolegal debate regarding the relationship between MS and trauma. The other issue is the cause or mechanism of injury. I discuss the medicolegal issue, as well as a pertinent clear cut case or MS related to whiplash in my book.
By the time brain scans are done the scars can be many years old. On the other hand, I had the experience of treating cases where the signs, symptoms and lesions all started to show up in just about a year. Two of those cases were especially severe and resulted in significant disabilities. In any case, most lesions in MS are permanent scars.
Unfortunately, oftentimes the scars are in bad locations as far as signs and symptoms are concerned. For example, the cervical cord contains all of the long myelinated tracts that pass from higher centers in the brain down to the arms and legs to work the muscles. Damage to these long tracts can cause permanent muscle weakness. The goal in these cases should be to restore function and halt further progression and disability as much as possible.
The lesions or scars of multiple sclerosis show up as bright spots
 called hyperintensity signals on MRI as seen in the brain scan on the right. Hyperintensity signals, however, are not unique to MS. Strokes and migraine headaches can also cause hyperintensity signals on brain scans in the area of impaired arterial blood flow.
called hyperintensity signals on MRI as seen in the brain scan on the right. Hyperintensity signals, however, are not unique to MS. Strokes and migraine headaches can also cause hyperintensity signals on brain scans in the area of impaired arterial blood flow.MS hyperintensity signals are more characteristically located above the covering over the posterior fossa, which contains the cerebellum as seen in the sketch below. Hence, the covering is called the tentorium cerebelli. MS lesions are typically found in supratentorial areas. Additionally, the hyperintensity signals are often found surrounding the chambers in the core of the brain called ventricles in the periventricular areas. The ventricles are the dark shadows in the brain scan above and chambers in the middle of the brain and brainstem seen in the sketch below.
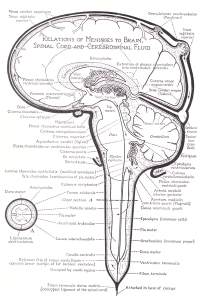 In addition to the supratentorial and periventricular areas, instead of arteries, as in strokes and migraine headaches, the lesions in MS are more typically found in what are called perivenular areas around the larger dural sinuses (veins) of the brain. They also tend to get smaller in number and size as you follow the blood vessels upstream counter-current to blood flow. This is the complete opposite of what you would expect if viruses were the cause because viruses follow blood flow. Consequently, the lesions would tend to show up in areas closer to the source of the stream in the arteries first, not so much further downstream in veins. Considering all the above, it’s hard to picture how stenosis in such distant jugular and thoracic veins could cause lesions to show up predominantly in the higher and core areas of the brain above the tentorium, and not more in the cerebellum, which is down in the basement of the cranial vault called the posterior fossa.
In addition to the supratentorial and periventricular areas, instead of arteries, as in strokes and migraine headaches, the lesions in MS are more typically found in what are called perivenular areas around the larger dural sinuses (veins) of the brain. They also tend to get smaller in number and size as you follow the blood vessels upstream counter-current to blood flow. This is the complete opposite of what you would expect if viruses were the cause because viruses follow blood flow. Consequently, the lesions would tend to show up in areas closer to the source of the stream in the arteries first, not so much further downstream in veins. Considering all the above, it’s hard to picture how stenosis in such distant jugular and thoracic veins could cause lesions to show up predominantly in the higher and core areas of the brain above the tentorium, and not more in the cerebellum, which is down in the basement of the cranial vault called the posterior fossa.In addition to the brain, MS lesions are sometimes found in the cervical cord as depicted in the old sketch above. In contrast to the core of the brain, lesions in the cord tend to show up on the outside along its flanks which contain the myelinated tracts mentioned above. Rarely ever do MS lesions show up below the shoulders. While MS lesions stop at the shoulders, however, other similar conditions associated with scarring similar to demyelination seen in the cervical cord in MS, are seen in the lower cord, such as amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s disease and primary lateral sclerosis (PLS). A variant of ALS, PLS can reach up into the brain as well. It’s called bulbar ALS. There is also a variant of MS, called Devic’s disease, that is associated with demyelination in the lower cord but optic neuritis in the brain. In addition to MS, I also treated patients with demyelinating diseases of the lower cord. At this time there is nothing anyone can do to stop the devastation in these conditions, but I believe we are getting closer, and a flood of cranked-up highly motivated MS patients are leading the way. When Parkinson’s patients join the fray the pressure will increase three fold, so will the money for further research into venous drainage problems.
Interestingly, while Asians have a lower incidence of MS they do get demyelinating diseases of the cord such as Devic’s disease. I believe it has to do with design differences between Caucasian and Asian skull designs. I will be covering demyelinating diseases of the lower cord on my new website, which is not quite ready for public viewing yet. Suffice it to say that demyelinating diseases of the cord are probably due to similar design problems and circulatory causes found in MS.
As far as the cause and location of the lesions of MS are concerned, Dr. Schelling’s theory makes the most sense. I will be discussing Schelling’s theory as to why the lesions show up where they do in my next post. I will also throw in some of my own two cents to add to the mix and maybe fill in some of the gaps. In brief, I believe that in certain cases of MS the hyperintensity signals and lesions are more likely due to decreased arterial blood flow similar to migraines and mini strokes, not venous drainage problems.
While curing the scars may be difficult or impossible, the location of the scars are often in areas that have nothing to do with many of the unusual signs and symptoms associated with MS, such as optic neuritis, ringing in the ears, trigeminal neuralgia, speech problems, balance problems, fatigue etc. Even more interesting is that, except for the eyes, most of the nerves that would cause such symptoms are found below the tentorium in the posterior fossa. Most of the signs and symptoms associated with Parkinson’s disease likewise come from the posterior fossa. Slowly but surely, trauma is being recognized as a possible causative factor of Parkinson’s just like MS. Furthermore, since the lesions don’t come and go in MS they can’t be the cause of remissions and exacerbations of signs and symptoms. This is a promising fact!
Halting the progression of MS and improving signs and symptoms unrelated to the lesions is definitely possible by restoring fluid mechanics in the brain. Upper cervical correction is one way to do it. The liberation procedure is another. We are on a completely new path but we have only taken the first step. Things can only get better as we learn more and continue to unravel the mystery of MS and the unique design of the incredible human brain due to upright posture. I believe upright MR and angiograms will shed much more light.
CCSVI or CCVBP
The term CCSVI (chronic cerebrospinal venous insufficiency) implies there is insufficient capacity in the venous drainage system to sufficiently drain the brain. The source of CCSVI is currently attributed to stenosis in distant jugular and thoracic veins that cause backups in the brain. While I believe that many cases are, in fact, caused by an insufficiency in drainage capacity, I don’t believe the vast majority of these cases are due to stenosis in jugular and thoracic veins.

Instead, I believe the insufficiency in most cases lies in less than perfect drainage designs of the brain inside the skull. The case on the left is supposedly caused by stenosis of the left internal jugular vein in front of the first and second cervical vertebral of the upper cervical spine. The problem is that many people are simply born with variations in design such as significantly smaller size in one of the transverse sinus to sigmoid sinus to internal jugular vein routes inside the skull. You can see the major drainage routes of the brain in the previous post. As an aside, the white you see in the scan are the spaces and chambers of the brain filled with water for cushioning and protection. The large chambers in the middle of the brain are where the water is produced.
It doesn’t matter though whether it is due to stenosis in the jugular and thoracic veins or a case of inherent insufficiency due to design problems. The good news is that in either case, regardless of where the insufficiency is found, the liberation procedure most likely works by acting like a siphon to assist in draining the backup in the brain. But knowing the precise location of the insufficiency could influence the decision as to where to do the angioplasty or to place the stents to be the most effective in future operations.
In this regard, I believe that the vast majority of cases of venous drainage problems in the brain, however, are not caused by insufficient drainage capacity. In contrast to insufficiency, I believe, most cases of venous drainage problems in the brain are due to chronic craniocervical venous back pressure or CCVBP, which is acquired through trauma, aging and degenerative conditions of the cervical spine. There is plenty of physical anthropological forensic evidence to support my theory which can be seen in normal, pathological and artificially deformed skulls. Further anthropological studies should be done. I discuss the topic thoroughly in my book in the chapter called “Acute Versus Chronic Back Pressure.” There are several scenarios that can cause CCVBP.
The brainstem passes through the foramen magnum in the base of the skull. The base of the skull in humans is bent, which puts the foramen magnum directy beneath a large portion of the mass of the brain and brainstem. This puts the brainstem in a precarious position in humans, perched above the foramen magnum below it, and beneath a large portion of the mass of the brain above which bears down on it. In this regard, a significant portion of the drainage system of the brain is found on the base of the skull near and in the foramen magnum making it especially susceptible to compression.

The Cisterns, Brain Flotation and Chiari
To keep it in its proper position the brainstem floats in a water jacket. The water around the brainstem and cerebellum near the base of the brain is contained in several large collapsible wells called cisterns. Because of the way this particular brain scan was done, in contrast to the preceding image, the cisterns are the shadows surrounding the brainstem and cerebellum and are filled with water. It’s the complete opposite of the other image where the water is white. As in the preceding image, the shadows in the middle of the brain and in the cerebellum are the chambers of the brain called ventricles. The ventricles are connected to the cisterns, but that’s another topic.
The cisterns are large dilations in the middle space of the protective coverings of the brain called the meninges. The space inside the protective coverings is called the subarachnoid space. The cisterns are part of the subarachnoid spaces that contain cerebrospinal fluid (CSF) and surround and protect the brainstem and cerebellum from banging into the hard bones of the base of the skull. More importantly, they protect the brainstem and cerebellum from sinking into the foramen magnum. This sinking is referred to as a pressure conus or Chiari malformation.
The shadow you see beneath the frontal lobe is the notch in the base of the skull for the pituitary gland. The crossing of the optic nerves lies just above the notch. Additionally, there is another important cistern that lies beneath the frontal lobe of the brain. It’s job is to protect the optic nerves from compression by the forebrain against the front of the base of the skull. Compression of the optic nerve is most likely one of the primary causes of optic neurtitis, which I will discuss further in future posts.
Getting back to the brainstem, a Chiari malformation can cause catastrophic consequences. Among other things, besides compressing the cord and potentially depressing all vital functions in the body, it can also block both venous blood and cerebrospinal fluid pathways that pass through the foramen magnum and into the spinal cord at this point.
The Occiput and Drainage Routes
Let’s forget about CSF for now and just focus on the venous outlets as they pertain to CCSVI. The sketches below are of the occipital bone which forms a large portion of the rear part of the base of the skull. It is also contains the attachment points for the upper cervical spine to the skull.
The sketch below is of the inside of the occipital bone. The view is from above looking down into the base of the skull. The transverse sinus, the internal occipital protuberance and occipital sinus inside the occipital bone are like dry river beds. The dural sinus veins of the brain channeled these courses into the bone just like a river cuts through earth and rock. The transverse sinus drainage routes head for the jugular veins. You can see the jugular notch which forms part of the jugular foramen.
Lower down, the occipital sinus system in the middle flows into the lowest drainage veins in the brain, which I call the basement veins. The best basement veins used by humans tend to be located in or near the foramen magnum. Two important outlets often used are the hypoglossal and condyloid canals. You can see the condyloid canal on the left. Notice how close it is to the jugular outlet.
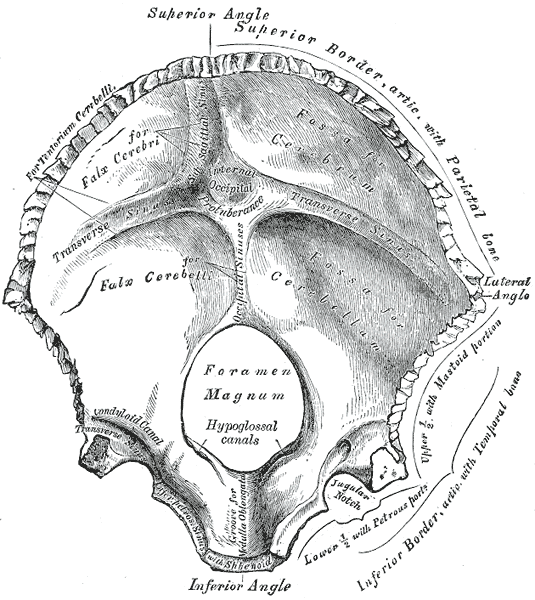
In addition to the vertebral vein connections, these outlets also contain important cranial nerves. One particular cranial nerve is called the hypoglossal nerve that goes to the tongue. Another cranial nerve is called the vagus nerve. Vagus means a wanderer like a vagabond. It called the wanderer because it wanders out from the brainstem to every organ in the chest and abdominal cavities and plays an important role in their function and regulation. Rubbing the carotid sinuses on either side of the Adam’s apple for example will cause a vasovagal response that lowers blood pressure.
Chiari Conditions, CCSVI and Nerve Compression
Chiari conditions can compress these and other cranial nerves just like the optic nerve mentioned above. Among other things, compression of the hypoglossal nerve can cause slurred speach. Compression of the vagus nerve can cause nausea, vomiting and feelings of fainting. Higher up in the cranial vault, compression of the optic nerve causes pain and blindness. Among other things, nerves do not like compression. Picture hitting your not so “funny” elbow bone and recall what that feels like. It’s like pressing on your eyeball or pinching your skin. It hurts. Nerves are meant to be highly sensitive. It’s there job to be sensitive. That’s why the brain is surrounded by water to protect it from compression against the hard walls of the cranial vault, as well as from itself.
The hypoglossal and condyloid canals exit the skull near the condyles on the bottom of the base of the skull. The condyles are large kidney shaped knuckle type joints that link the skull to the first cervical vertebra called atlas or C1.
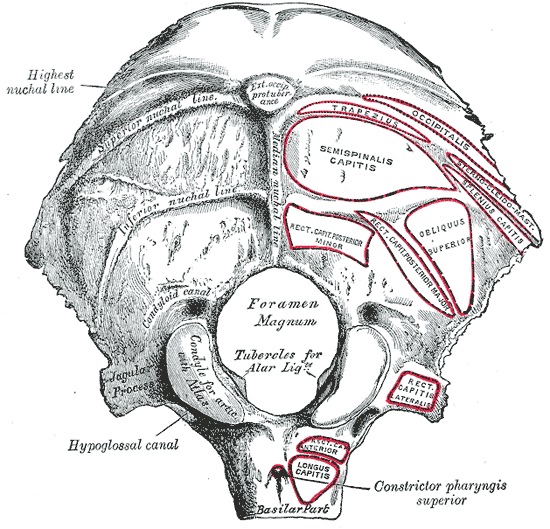
The Upper Cervial Connection to Chiari and CCSVI
The ridges and circles you see on the sketch are for the attachment of the neck and special upper cervical muscles. I will be discussing misalignments of the upper cervical spine so it is important to understand the relationship of the atlas vertebra in the upper cervical spine to the jugular foramen and the hypoglossal and condyloid canal outlets. As you can see in the sketches above, they are all located close to the atlas vertebra. The transverse processes of atlas extends out toward the jugular notch. Because of this close arrangement it only takes microplastic, miniscule misalignment type strains to cause compression of the soft tissues surrounding the openings in the base of the skull and subsequent back pressure against their veins that can have a major impact on fluid mechanics in the brain.
Back pressure against the veins of the brain near the base of the skull can cause venous congestion called edema inside the brain. It can also decrease the passive CSF production pressure gradient used during upright posture for brain support. This would cause a decrease in CSF volume in the cisterns thus raising the risk of a pressure conus or Chiari type conditon. Chiari conditions in turn further plug the foramen magnum and consequently the hypoglossal and condyloid canals further complicating problems with back pressure and venous backups. They also trap CSF in the cisterns and ventricles, but again, that’s another story.
I will be discussing the arterial arrangement of the posterior blood supply to the brain in future posts. I will also be covering misalignments in the upper cervical spine. After you understand the arrangement of these arteries and veins it will be easy to see how small misalignments in the upper cervical spine can have a major impact on the health of the brain. They can also affect the spinal cord, but we aren’t even close to covering issues related to the cord at this juncture. The brain is complicated enough for now.

Instead, I believe the insufficiency in most cases lies in less than perfect drainage designs of the brain inside the skull. The case on the left is supposedly caused by stenosis of the left internal jugular vein in front of the first and second cervical vertebral of the upper cervical spine. The problem is that many people are simply born with variations in design such as significantly smaller size in one of the transverse sinus to sigmoid sinus to internal jugular vein routes inside the skull. You can see the major drainage routes of the brain in the previous post. As an aside, the white you see in the scan are the spaces and chambers of the brain filled with water for cushioning and protection. The large chambers in the middle of the brain are where the water is produced.
It doesn’t matter though whether it is due to stenosis in the jugular and thoracic veins or a case of inherent insufficiency due to design problems. The good news is that in either case, regardless of where the insufficiency is found, the liberation procedure most likely works by acting like a siphon to assist in draining the backup in the brain. But knowing the precise location of the insufficiency could influence the decision as to where to do the angioplasty or to place the stents to be the most effective in future operations.
In this regard, I believe that the vast majority of cases of venous drainage problems in the brain, however, are not caused by insufficient drainage capacity. In contrast to insufficiency, I believe, most cases of venous drainage problems in the brain are due to chronic craniocervical venous back pressure or CCVBP, which is acquired through trauma, aging and degenerative conditions of the cervical spine. There is plenty of physical anthropological forensic evidence to support my theory which can be seen in normal, pathological and artificially deformed skulls. Further anthropological studies should be done. I discuss the topic thoroughly in my book in the chapter called “Acute Versus Chronic Back Pressure.” There are several scenarios that can cause CCVBP.
The brainstem passes through the foramen magnum in the base of the skull. The base of the skull in humans is bent, which puts the foramen magnum directy beneath a large portion of the mass of the brain and brainstem. This puts the brainstem in a precarious position in humans, perched above the foramen magnum below it, and beneath a large portion of the mass of the brain above which bears down on it. In this regard, a significant portion of the drainage system of the brain is found on the base of the skull near and in the foramen magnum making it especially susceptible to compression.

The Cisterns, Brain Flotation and Chiari
To keep it in its proper position the brainstem floats in a water jacket. The water around the brainstem and cerebellum near the base of the brain is contained in several large collapsible wells called cisterns. Because of the way this particular brain scan was done, in contrast to the preceding image, the cisterns are the shadows surrounding the brainstem and cerebellum and are filled with water. It’s the complete opposite of the other image where the water is white. As in the preceding image, the shadows in the middle of the brain and in the cerebellum are the chambers of the brain called ventricles. The ventricles are connected to the cisterns, but that’s another topic.
The cisterns are large dilations in the middle space of the protective coverings of the brain called the meninges. The space inside the protective coverings is called the subarachnoid space. The cisterns are part of the subarachnoid spaces that contain cerebrospinal fluid (CSF) and surround and protect the brainstem and cerebellum from banging into the hard bones of the base of the skull. More importantly, they protect the brainstem and cerebellum from sinking into the foramen magnum. This sinking is referred to as a pressure conus or Chiari malformation.
The shadow you see beneath the frontal lobe is the notch in the base of the skull for the pituitary gland. The crossing of the optic nerves lies just above the notch. Additionally, there is another important cistern that lies beneath the frontal lobe of the brain. It’s job is to protect the optic nerves from compression by the forebrain against the front of the base of the skull. Compression of the optic nerve is most likely one of the primary causes of optic neurtitis, which I will discuss further in future posts.
Getting back to the brainstem, a Chiari malformation can cause catastrophic consequences. Among other things, besides compressing the cord and potentially depressing all vital functions in the body, it can also block both venous blood and cerebrospinal fluid pathways that pass through the foramen magnum and into the spinal cord at this point.
The Occiput and Drainage Routes
Let’s forget about CSF for now and just focus on the venous outlets as they pertain to CCSVI. The sketches below are of the occipital bone which forms a large portion of the rear part of the base of the skull. It is also contains the attachment points for the upper cervical spine to the skull.
The sketch below is of the inside of the occipital bone. The view is from above looking down into the base of the skull. The transverse sinus, the internal occipital protuberance and occipital sinus inside the occipital bone are like dry river beds. The dural sinus veins of the brain channeled these courses into the bone just like a river cuts through earth and rock. The transverse sinus drainage routes head for the jugular veins. You can see the jugular notch which forms part of the jugular foramen.
Lower down, the occipital sinus system in the middle flows into the lowest drainage veins in the brain, which I call the basement veins. The best basement veins used by humans tend to be located in or near the foramen magnum. Two important outlets often used are the hypoglossal and condyloid canals. You can see the condyloid canal on the left. Notice how close it is to the jugular outlet.
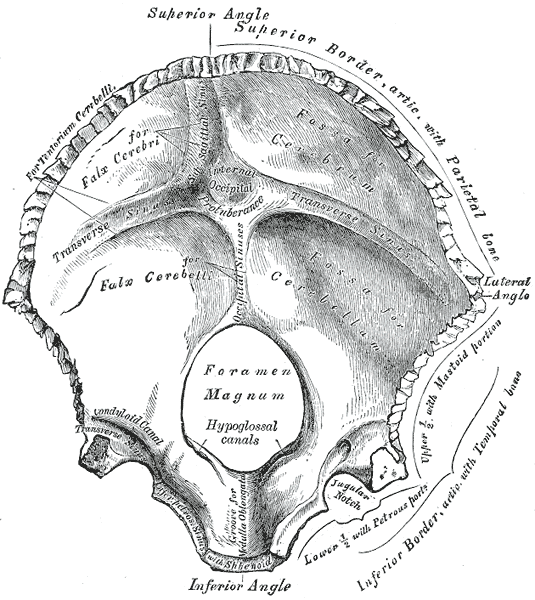
In addition to the vertebral vein connections, these outlets also contain important cranial nerves. One particular cranial nerve is called the hypoglossal nerve that goes to the tongue. Another cranial nerve is called the vagus nerve. Vagus means a wanderer like a vagabond. It called the wanderer because it wanders out from the brainstem to every organ in the chest and abdominal cavities and plays an important role in their function and regulation. Rubbing the carotid sinuses on either side of the Adam’s apple for example will cause a vasovagal response that lowers blood pressure.
Chiari Conditions, CCSVI and Nerve Compression
Chiari conditions can compress these and other cranial nerves just like the optic nerve mentioned above. Among other things, compression of the hypoglossal nerve can cause slurred speach. Compression of the vagus nerve can cause nausea, vomiting and feelings of fainting. Higher up in the cranial vault, compression of the optic nerve causes pain and blindness. Among other things, nerves do not like compression. Picture hitting your not so “funny” elbow bone and recall what that feels like. It’s like pressing on your eyeball or pinching your skin. It hurts. Nerves are meant to be highly sensitive. It’s there job to be sensitive. That’s why the brain is surrounded by water to protect it from compression against the hard walls of the cranial vault, as well as from itself.
The hypoglossal and condyloid canals exit the skull near the condyles on the bottom of the base of the skull. The condyles are large kidney shaped knuckle type joints that link the skull to the first cervical vertebra called atlas or C1.
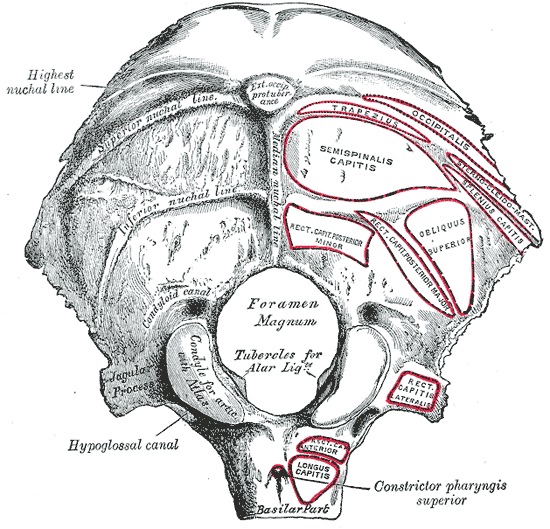
The Upper Cervial Connection to Chiari and CCSVI
The ridges and circles you see on the sketch are for the attachment of the neck and special upper cervical muscles. I will be discussing misalignments of the upper cervical spine so it is important to understand the relationship of the atlas vertebra in the upper cervical spine to the jugular foramen and the hypoglossal and condyloid canal outlets. As you can see in the sketches above, they are all located close to the atlas vertebra. The transverse processes of atlas extends out toward the jugular notch. Because of this close arrangement it only takes microplastic, miniscule misalignment type strains to cause compression of the soft tissues surrounding the openings in the base of the skull and subsequent back pressure against their veins that can have a major impact on fluid mechanics in the brain.
Back pressure against the veins of the brain near the base of the skull can cause venous congestion called edema inside the brain. It can also decrease the passive CSF production pressure gradient used during upright posture for brain support. This would cause a decrease in CSF volume in the cisterns thus raising the risk of a pressure conus or Chiari type conditon. Chiari conditions in turn further plug the foramen magnum and consequently the hypoglossal and condyloid canals further complicating problems with back pressure and venous backups. They also trap CSF in the cisterns and ventricles, but again, that’s another story.
I will be discussing the arterial arrangement of the posterior blood supply to the brain in future posts. I will also be covering misalignments in the upper cervical spine. After you understand the arrangement of these arteries and veins it will be easy to see how small misalignments in the upper cervical spine can have a major impact on the health of the brain. They can also affect the spinal cord, but we aren’t even close to covering issues related to the cord at this juncture. The brain is complicated enough for now.
Posted in Alzheimer's, ccsvi, multiple sclerosis, Parkinson's, physical anthropology 8 Comments
Upper Cervical Strain and CCSVI
The image on the right is an excellent MR venogram of the brain. If you are interested in the names of the veins, just click on the image and you will see the annotations. The largest veins you see are the superior sagittal sinus at the top, the transverse to sigmoid sinuses located along the bottom running somewhat horizontally and then downward from the back toward the front of the skull and finally the internal jugular veins descending straight down the neck.
There is another interesting vein called the straight sinus which takes off at approximately a 45 degree angle forward and upward from the transverse sinus. The straight sinus is pertinent to Dr. Schelling’s research involving the location of the lesions in MS. According to Schelling, one of the key areas that reverse flows, called back jets, vent into is the straight sinus. This explains why lesions tend to show up in areas surrounding tributary veins of the straight sinus. I will discuss more on Schelling’s research about the location of the lesions in future posts.
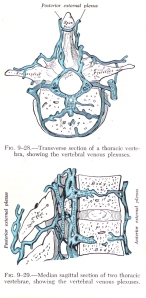 The network of much smaller veins below the transverse sinus and behind the internal jugulars, is the vertebral veins, more commonly called the vertebral venous plexus (VVP). A plexus is a network, which is exactly what the VVP is. Although the individual veins may be small, the drainage capacity of the vast network of veins of the VVP located inside the spinal canal and surrounding spine is huge.
The network of much smaller veins below the transverse sinus and behind the internal jugulars, is the vertebral veins, more commonly called the vertebral venous plexus (VVP). A plexus is a network, which is exactly what the VVP is. Although the individual veins may be small, the drainage capacity of the vast network of veins of the VVP located inside the spinal canal and surrounding spine is huge.
Some of the most important extra venous outlets in humans that drain into the cervical VVP are located around the foramen magnum. Some actually pass through it. Another frequently used route is located behind the mastoid bone of the ear. There are many different design variations in the extra venous outlets used by humans for upright posture. Some designs simply work better than others and some are predisposed to drainage issues due to reduced capacity by design.
The image below is of a female with migraine headaches which, interestingly, is sometimes associated with MS. The image on the left taken before a chiropractic upper cervical correction shows significantly more blood flow through the left and right internal jugular veins. Following upper cervical correction flow through the internal jugular veins is considerably reduced and blood flow through the vertebral veins seen in the middle in the area of the foramen magnum is increased.

What’s particularly fascinating about this MR venogram image is that it was done with the patient lying down, when the demands on the VVP are significantly lower. The primary role of the VVP is to drain the brain during upright posture. Even so, it nonetheless appears to play a prominent role in the recumbent position as well.
In this case the sigmoid sinus to internal jugular vein routes were being overburdened due to a venous shift in their direction as a consequence of reduced drainage capacity in the cervical portion of the VVP drainage routes. The reduced drainage capacity of the brain to cervical VVP routes was the result of a chronic upper cervical strain chiropractors call a subluxation. In this case the burden on the jugulars would have further increased significantly during upright posture due to failure of the VVP.
In other words, the cause of the CCSVI in this case was due to back pressure and sluggish circulation in the VVP as a result of an upper cervical subluxation, not faults, such as stenosis in the jugular routes.
There is another interesting vein called the straight sinus which takes off at approximately a 45 degree angle forward and upward from the transverse sinus. The straight sinus is pertinent to Dr. Schelling’s research involving the location of the lesions in MS. According to Schelling, one of the key areas that reverse flows, called back jets, vent into is the straight sinus. This explains why lesions tend to show up in areas surrounding tributary veins of the straight sinus. I will discuss more on Schelling’s research about the location of the lesions in future posts.
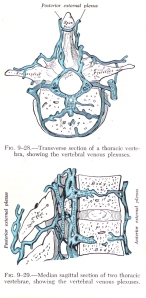 The network of much smaller veins below the transverse sinus and behind the internal jugulars, is the vertebral veins, more commonly called the vertebral venous plexus (VVP). A plexus is a network, which is exactly what the VVP is. Although the individual veins may be small, the drainage capacity of the vast network of veins of the VVP located inside the spinal canal and surrounding spine is huge.
The network of much smaller veins below the transverse sinus and behind the internal jugulars, is the vertebral veins, more commonly called the vertebral venous plexus (VVP). A plexus is a network, which is exactly what the VVP is. Although the individual veins may be small, the drainage capacity of the vast network of veins of the VVP located inside the spinal canal and surrounding spine is huge.Some of the most important extra venous outlets in humans that drain into the cervical VVP are located around the foramen magnum. Some actually pass through it. Another frequently used route is located behind the mastoid bone of the ear. There are many different design variations in the extra venous outlets used by humans for upright posture. Some designs simply work better than others and some are predisposed to drainage issues due to reduced capacity by design.
The image below is of a female with migraine headaches which, interestingly, is sometimes associated with MS. The image on the left taken before a chiropractic upper cervical correction shows significantly more blood flow through the left and right internal jugular veins. Following upper cervical correction flow through the internal jugular veins is considerably reduced and blood flow through the vertebral veins seen in the middle in the area of the foramen magnum is increased.

What’s particularly fascinating about this MR venogram image is that it was done with the patient lying down, when the demands on the VVP are significantly lower. The primary role of the VVP is to drain the brain during upright posture. Even so, it nonetheless appears to play a prominent role in the recumbent position as well.
In this case the sigmoid sinus to internal jugular vein routes were being overburdened due to a venous shift in their direction as a consequence of reduced drainage capacity in the cervical portion of the VVP drainage routes. The reduced drainage capacity of the brain to cervical VVP routes was the result of a chronic upper cervical strain chiropractors call a subluxation. In this case the burden on the jugulars would have further increased significantly during upright posture due to failure of the VVP.
In other words, the cause of the CCSVI in this case was due to back pressure and sluggish circulation in the VVP as a result of an upper cervical subluxation, not faults, such as stenosis in the jugular routes.
CCSVI, Brain Cooling and Blood Flow
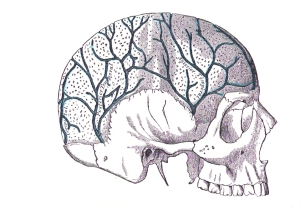
The upper cervical spine plays an important role in the venous drainage system of the brain, brain blood flow and brain cooling. Back pressure against the vertebral venous outlets in the upper cervical spine can thus be a cause of CCSVI, decreased blood flow and decreased cooling capacity of the brain. An overview of the cranial veins will make the connection clear.
The cranial veins include the veins of the face and scalp, the diploic veins, the emmisary veins and the dural sinues. The diploic veins, seen in the picture above, and mentioned in the previous post, sit between the inner and outer plates of the membranous bones of the skull that cover the cranial vault.
The dural sinuses seen in the pictures below are the main drainage routes of the brain inside the cranial vault. They are called dural sinues because they are not true veins. Instead they are tunnels formed by the outer coat of the brain itself, the dura mater. The inside walls of the dural sinuses are lined with the inner walls of veins. The dura mater, which means tough mother or material, makes the dural sinus drainage system much stronger than typical veins. As a result, they are better able to withstand stress and resist deformation from the pressure and movement of the brain, which sits on top of and presses down against them.
The cranial veins of the face and scalp, diploe and dural sinuses are all interconnected by the emissary veins. In contrast to the rest of the body, none of the cranial veins have valves to check or prevent reverse flows. That’s an important fact when it comes to discussing MS lesions, which I won’t go into here.
 If you click on the picture to the left and look closely, you will see that the dural sinuses are depicted by stripes inside the skull. You will also see little black semicircles on the top and the bottom of the skull. The semicircles represent emissary veins, which link the face and scalp veins to the diploic veins and to the dural sinues.
If you click on the picture to the left and look closely, you will see that the dural sinuses are depicted by stripes inside the skull. You will also see little black semicircles on the top and the bottom of the skull. The semicircles represent emissary veins, which link the face and scalp veins to the diploic veins and to the dural sinues.The emissary veins play an important role in draining the head and brain. The ones located toward the back and bottom of the skull seen behind the outline of the ear, drain into the vertebral veins of the spine. In addition to drainage, the emissary veins also play a critical role in cooling the brain. They do so by delivering blood, that has been cooled by conduction and sweat evaporation at the surface of the face and scalp, to the diploe and to the dural sinues.
Besides cooling the diploe and dural sinuses, the brain also uses two counter current heat exchanger tunnel systems in the dural sinuses to cool incoming arterial blood before it enters the brain.
 The two cavernous (dural) sinuses are located inside the cranial vault. If you click on the picture to the right you will see the internal carotid depicted passing through the cavernous sinus before it enters the brain.
The two cavernous (dural) sinuses are located inside the cranial vault. If you click on the picture to the right you will see the internal carotid depicted passing through the cavernous sinus before it enters the brain.The other tunnel is called the suboccipital cavernous sinus, which is also known as the atlantooccipital membrane as depicted in the picture below. The suboccipital cavernous sinus is located just outside the skull between the first cervical vertebra and the occipital bone at base of the skull.

Even though it is outside the skull, studies have shown that the suboccipital cavernous sinus is constructed of nearly identical materials, in the same way and serves the same function as the cavernous sinus. For this reason, some scientists now consider it to be part of the dural sinuses of the brain. The suboccipital cavernous sinus contains and cools the two vertebral arteries before they enter the brain.
Thus, the brain is surrounded by cooled venous blood in the cranium and incoming arterial blood keeping the brain about two to three degrees cooler than the rest of the body. Some physical anthropologists attribute the extra large size of the human brain more to its exceptional cooling capacity than to the increase in arterial blood flow that comes with upright posture. Anthroplogists refer to human encephalization due to enhanced cooling capacity as the “radiator theory.”
Both the cavernous and suboccipital cavernous sinuses also play a role in maintaining blood flow and pressure in the brain. Their inner walls contain pressure sensors called baroreceptors that detect pressure in the tunnels. When pressure goes up they send signals that cause the muscles in the incoming arteries to constrict and decrease blood flow. When pressure drops they signal the blood vessels to open up and increase blood flow. Technically it is called the “neurovascular myogenic autoregulatory reflex mechanism.” As an aside, similar important pressure receptors and blood flow regulators are located in the carotid sinuses near the Adams apple of the throat.
The cranial veins drain into two extracranial venous drainage routes. One route is the jugular veins. The other is the vertebral veins. Interestingly, in contrast to the jugular veins, the vertebral veins have no valves making them similar to the cranial veins. Thus, back pressure against the vertebral veins can affect both the drainage and cooling capacity of the brain. This is interesting in light of the fact that in addition to evidence of CCSVI, MS patients often experience symptoms of heat intolerance.
An increase in pressure in the suboccipital cavernous sinus can also decrease blood flow through the vertebral arteries that pass through it before supplying the inner rear and lower most parts of the brain. It can do so by either direct compression of the vertebral arteries, or by stimulating the pressure sensors in the sinus walls thereby causing the arteries to constrict.
Decreased blood flow through the vertebral arteries can cause a wide variety of symptoms such as fatigue, dizziness, loss of balance and coordination to name a few. The complete list of symptoms is too long to discuss here so I will save it for future posts.
Posted in ccsvi, multiple sclerosis, physical anthropology 19 Comments
Cranial Sutures and CCSVI
 The skull is made up of cartilagenous and membranous bones. The cartilagenous bones make up the base of the skull and are more related to the musculoskeletal system of the spine. In contrast, the membranous bones form the cover over the cranial vault of the brain. They are called membranous bones because in childhood they grow within the outer membrane of the brain and typically, but not always, follow the brain’s growth.
The skull is made up of cartilagenous and membranous bones. The cartilagenous bones make up the base of the skull and are more related to the musculoskeletal system of the spine. In contrast, the membranous bones form the cover over the cranial vault of the brain. They are called membranous bones because in childhood they grow within the outer membrane of the brain and typically, but not always, follow the brain’s growth.The membranous bones of the skull are separated by large spaces in infants that later start to close as a child matures. The special joints that join the membranous bones together are called sutures because their unusual shapes looked like stitches to early anatomists. All bones are a reflection of the stresses that strain them. In this case the stress that strains the sutures comes from veins within the membranous bones called diploe. The sutures thus provide forensic evidence of drainage issues in the brain.
My investigation into the role of venous drainage issues in neurodegenerative diseases began sometime around 1984 while I was studying artificially deformed skulls from former indigenous people of Peru and Bolivia. The wide open state of some of the skull’s sutures that should have been closed caused me to look into hydrocephalus. Hydrocephalus in turn led to a condition called normal pressure hydrocephlaus or NPH, which is sometimes associated with Alzheimer’s disease. AD next led to Parkinson’s disease because they sometimes share a suspicious and strange relationship in that one condition can progress into the other. AD also affects the periventricular areas of the brain, which is where the lesions in MS are often found. Consequently, MS kept turning up in my searches and so it got included in my research from the start. The biggest problem for me, however, was explaining the peculiar characteristics of the locations of the lesions seen in MS. One of those unusual characteristics is that the lesions tend to be located around the largest veins in the brain.
 Schelling similarly began his research into the peculiar lesions of MS sometime around 1974 while studying skulls. In contrast to the sutures of the skull, however, Schelling got started after he noticed large differences in the jugular and other venous outlets of the skull in MS patients. The jugular foramen are the large holes you see in the picture, on the left and right side of the foramen magnum which is located in the middle. Schelling’s research provided many of the answers I was looking for when it came to the lesions of MS. I will do my best to summarize his findings in future posts. For now, I believe that what Schelling saw was skulls with design issues associated with reduced venous drainage capacity of the brain. In other words, what Schelling saw in the skulls way back in 1974 was forensic evidence of the role of CCSVI in causing MS.
Schelling similarly began his research into the peculiar lesions of MS sometime around 1974 while studying skulls. In contrast to the sutures of the skull, however, Schelling got started after he noticed large differences in the jugular and other venous outlets of the skull in MS patients. The jugular foramen are the large holes you see in the picture, on the left and right side of the foramen magnum which is located in the middle. Schelling’s research provided many of the answers I was looking for when it came to the lesions of MS. I will do my best to summarize his findings in future posts. For now, I believe that what Schelling saw was skulls with design issues associated with reduced venous drainage capacity of the brain. In other words, what Schelling saw in the skulls way back in 1974 was forensic evidence of the role of CCSVI in causing MS.Drainage issues such as those I saw in the artificially deformed skulls, hydrocehalus, and many other pathological skulls, including those with drainage design issues such as undersized jugular foramen, exaggerate the affects of hydraulic stress within the sutures of the membranous bones and cause them to stay open. These open sutures were exactly what I saw during my research. Just think, if venous pressure can carve bones and cause the sutures to stay open, imagine what water pressure within the skull, due to poor drainage issues, can do to the much softer tissues of the brain. I will discuss MS signs, symptoms and lesions due to drainage issues in future posts.
Dr. Zamboni only recently started looking into the role of venous drainage issues in neurodegenerative diseases after his wife became afflicted with MS. Consequently, he may be unaware of the full ramifications of CCSVI, and his surgical procedure which, is in terms of its development, in its infancy. There is far more to CCSVI than simply MS, and his liberation procedure may have far greater justification for its use in many more patients than Dr. Zamboni ever imagined when he first began his research.
MS is just the tip of the iceberg. It is my opinion that humans are predisposed to neurodegenerative diseases due to the design of the skull, spine and circulatory system of the brain as a result of upright posture. Some designs are less than perfect. In contrast to stenosis of distant jugular and thoracic veins causing CCSVI, I believe more people are affected by reduced drainage capacity issues in the skull and brain. Time will tell. In either case, the liberation procedure is probably the best answer for many cases of reduced drainage capacity due to design issues and it will most likely continue to evolve and improve. There is much more to this story.
Posted in ccsvi, multiple sclerosis, physical anthropology 4 Comments
Brainstem and Venous Liberation

Among other things, trauma has been associated with what is called Chiari conditions, also know as cerebellum tonsillar ectopia or CTE. Chairi conditions are classified according to the severity of the depth of penentration of the cerebellum into the foramen magnum. One of the areas often involved are the tonsils of the cerebellum.
I won’t go into all the ramifications of deformation of the relationship between the brain and cord within the foramen magnum and spinal canal here. Suffice it to say, however, that they most likely don’t deform together. Instead the head and neck and the rest of the spine twist and deform around the brainstem and cord.
The brainstem liberation procedure requires reduction of the strain in the structure that surrounds it. By realigning the foramen magnum in base of the skull with the spinal canal the strain and deformation of the brainstem and cord is reduced and their position within thier respective canals, likewise, returns to normal thus liberating the brainstem and vertebral veins.
The upper cervical spine provides the greatest leverage and contact point for attempting to reduce the strain. The upper cervical spine in this case is carefully assessed and realigned to the base of the skull with a thrust from various types of forces in use by different methodologies in chiropractic. Some use their hands. Some use little hammers and some use sound waves. Some use short snappy little thrusts. Others use longer slow sustained pressure. None are uncomfortable to the patient. No anesthesia is required.
 This is an old picture of a knee chest toggle recoil type of upper cervical adjustment, which is the original method developed by BJ Palmer and what I was taught in school. In this case, the force is delivered through a small point of the the pisaform (wrist bone) of the doctor’s contact hand. A quick snap of the arms delivers a precise shallow force, which was followed by an instant recoil of the arms along with a body release by the doctor. Before working on other students we trained our muscles to snap appropriately and worked on mechanical speeders. Chiropractors would have contests at symposiums to see who could work on a speeder, with an egg placed on top, without breaking the egg. It was a tough challenge indeed but the purpose behind it was to demonstrate how shallow a force is needed with the addition of speed to produce a desired result. The desired result being to put the vertebra in motion in the desired direction. The original procedure has gone through many modifications and improvements.
This is an old picture of a knee chest toggle recoil type of upper cervical adjustment, which is the original method developed by BJ Palmer and what I was taught in school. In this case, the force is delivered through a small point of the the pisaform (wrist bone) of the doctor’s contact hand. A quick snap of the arms delivers a precise shallow force, which was followed by an instant recoil of the arms along with a body release by the doctor. Before working on other students we trained our muscles to snap appropriately and worked on mechanical speeders. Chiropractors would have contests at symposiums to see who could work on a speeder, with an egg placed on top, without breaking the egg. It was a tough challenge indeed but the purpose behind it was to demonstrate how shallow a force is needed with the addition of speed to produce a desired result. The desired result being to put the vertebra in motion in the desired direction. The original procedure has gone through many modifications and improvements.There may be other equally valid ways of liberating the brainstem and vertebral veins, but for now, only upper cervical chiropractic has the research behind it and is the least invasive. This is just as important and just as significant to MS research as the venous stenosis theory. Nobody has all the answers yet. We are simply scratching at the surface of a whole new direction in research far different than the immunological or inflammatory theory paths we have been following for decades without much in the way of results. I am sure that there is going to be much more to this unfolding story. Upright brain scans and MR angiorgrams will provide more clues.
Posted in ccsvi, liberation procedure, multiple sclerosis, Uncategorized 2 Comments
CCSVI, US and MR Angiograms
The diagnosis of CCSVI is currently based on ultrasound scans of the jugular and thoracic veins This is problematic because for one not everyone is getting the same results using US scans to find venous stenosis due to operator errors/differences. For another, stenosis is a relative term since all vessels are capable of compliance to meet loads and demands. Still another most important fact is that scanning extracranial vessels is an indirect assesment of the intracranial venous circulation in the brain.
In contrast to US scans, MR angiograms are a direct assesment of venous drainage issues of the brain inside the cranial vault. Most MR scans, however, are done in the supine position, with the patient lying down with their face up. This is the least informative way to study faulty fluid mechanics in the brain because humans get into trouble as a result of faulty fluid mechanics due to upright posture.
I have been a fan of upright MR since they first came out. Dr. Noam Alperin of the Department of Radiology of the University of Miami is a big advocate and one of the leading experts in the world on Phase Contrast Upright MR scans and angiograms. The reason why is that upright posture significantly changes blood flow and fluid mechanics in the brain. As an aside Dr. Alperin had this to say about my book, “You did an outstanding job. Like you we believe that venous drainage plays an important role in ICP (intracranial pressure).”
Interestingly, recent upright MR angiograms by Alperin support anthropological evidence that extra venous outlets evolved in humans and hominids to offset the increase in blood flow that comes from upright posture. Those extra venous outlets drain into the vertebral veins of the spine, not the jugular veins. That is, upright posture causes venous outflow to shift in favor of the vertebral veins. If the vertebral veins become blocked the burden then falls on the jugular veins, which sit slightly higher in the bottom of the sink of the cranial vault. Because of their location and the design of the bent base of the skull, the jugular routes are less efficient for the bottom of the vault, which is why humans specifically developed extra accessory outlets that drain into nearby vertebral veins in and around the spine and spinal canal.
While the liberation procedure by all accounts so far has worked well for many MS patients, it may be working for other reasons. Dr. Zamboni may have it backwards. The vertebral veins are not used for back up to the jugular veins. Instead, the jugular veins are used when the vertebral veins become backed up during upright posture. Using jugular routes to offload back ups in the vertebral veins is not the most efficienct way. The most efficient way is through the vertebral veins as nature intended. The liberation procedure may be the the best way for now of relieving venous congestion in the brain. But it is probably not the best or most efficient way of improving flow through the vertebral veins. The best way of improving flow through the vertebral veins would be to remove the source of back pressure in the upper cervical spine. On the other hand, some patients may need stents and upper cervical correction. Time will tell, but unlike all the research over the past few decades, the issue of CCSVI won’t take as long to figure out because of the technology of upright brain scans.
In contrast to US scans, MR angiograms are a direct assesment of venous drainage issues of the brain inside the cranial vault. Most MR scans, however, are done in the supine position, with the patient lying down with their face up. This is the least informative way to study faulty fluid mechanics in the brain because humans get into trouble as a result of faulty fluid mechanics due to upright posture.
I have been a fan of upright MR since they first came out. Dr. Noam Alperin of the Department of Radiology of the University of Miami is a big advocate and one of the leading experts in the world on Phase Contrast Upright MR scans and angiograms. The reason why is that upright posture significantly changes blood flow and fluid mechanics in the brain. As an aside Dr. Alperin had this to say about my book, “You did an outstanding job. Like you we believe that venous drainage plays an important role in ICP (intracranial pressure).”
Interestingly, recent upright MR angiograms by Alperin support anthropological evidence that extra venous outlets evolved in humans and hominids to offset the increase in blood flow that comes from upright posture. Those extra venous outlets drain into the vertebral veins of the spine, not the jugular veins. That is, upright posture causes venous outflow to shift in favor of the vertebral veins. If the vertebral veins become blocked the burden then falls on the jugular veins, which sit slightly higher in the bottom of the sink of the cranial vault. Because of their location and the design of the bent base of the skull, the jugular routes are less efficient for the bottom of the vault, which is why humans specifically developed extra accessory outlets that drain into nearby vertebral veins in and around the spine and spinal canal.
While the liberation procedure by all accounts so far has worked well for many MS patients, it may be working for other reasons. Dr. Zamboni may have it backwards. The vertebral veins are not used for back up to the jugular veins. Instead, the jugular veins are used when the vertebral veins become backed up during upright posture. Using jugular routes to offload back ups in the vertebral veins is not the most efficienct way. The most efficient way is through the vertebral veins as nature intended. The liberation procedure may be the the best way for now of relieving venous congestion in the brain. But it is probably not the best or most efficient way of improving flow through the vertebral veins. The best way of improving flow through the vertebral veins would be to remove the source of back pressure in the upper cervical spine. On the other hand, some patients may need stents and upper cervical correction. Time will tell, but unlike all the research over the past few decades, the issue of CCSVI won’t take as long to figure out because of the technology of upright brain scans.
Posted in ccsvi, liberation procedure, multiple sclerosis Tagged ccsvi, multiple sclerosis 1 Comment
Physical Anthropology and CCSVI
Of all the research I have read on neurodegenerative diseases, brain scans are perhaps the most cumbersome because it relates so much to physics and mathmatical medicine. As unbelievable as it may seem, physical anthropology papers can be far worse, almost as if they are speaking in a different language, which is unfortunate because, physical anthropology is loaded with practical information when it comes to health issues related to upright posture. It is extremely important to the current hot topic of neurodegenerative diseases.
According to physical anthropologist Dr. Dean Falk (who incidently majored in math before undertaking physical anthropology) of the University of Florida, humans and hominids developed extra venous drainage outlets in the base of the skull to offset the increase in blood flow that comes from upright posture. Those extra outlets drain into the vertebral veins of the spine, not the jugular veins. Furthermore, the lowest outlets lie below the level of the jugular foramen in the floor of the basement of the cranial vault.
In her paper Evolution of Cranial Blood Drainage in Hominids: Enlarged Occipital/Marginal Sinuses and Emissary Foramina published in 1986, Falk describes numerous design variations, some of which led to the design variations currently found in humans, which are great in number. Many people as Schelling noted, have large discrepancies, for example, in the size of the jugular and other outlets. I have personally seen skulls with a large jugular foramen on one side and a small one on the other. In other cases, openings that were normally found were absent. This is important because design issues, as well as certain diseases, can affect the drainage capacity and efficiency of the system. Consequently, they may predispose certain cases to venous drainage issues. What’s particulary interesting about Schelling’s findings of discrepancies in designs of drainage outlets in crania is that they were associated with known cases of MS.
In addition to research into the drainage system of the human brain, physical anthropology contains a great deal of practical forensic physical evidence in the form of normal and pathological skulls, as well as the artificially deformed skulls I studied. The science of physcial anthropology needs to get involved in this research.
I sent complimentary copies of my book to Dr. Falk, as well as Dr. Dan Lieberman of Harvard University. Dr. Lieberman is better known as the barefoot doctor. His interests are in health issues related to upright posture. One of his interests is in the bent base of the human skull, the same as mine. It would be great to get both Falk and Lieberman, or other experts of the same caliber, involved in this research. The bent base and design of the drainage system is most important to this research. There are far too many anatomical variations to deal with in physiological studies. Time will tell. Eventually, the subject may hook someone in physcial anthropology.
Posted in ccsvi, multiple sclerosis, physical anthropology Tagged ccsvi, ms, physical anthroplogy Leave a comment
Stenosis Versus Compliance in CCSVI
There are obviously problems in using ultrasound to determine venous stenosis. For one not everyone is coming up with the same results. The other problem, when it comes to stenosis, is that veins and arteries are dynamic, not static. They change according to circumstances and loads. Technically, it’s called compliance.
During inversion for example, there is a great deal of compliance in the vertebral veins in the spinal canal and the dural sinuses of the brain which have no valves to prevent or check reverse flow, such as those found in the jugular and most other veins. In the extremities, veins expand easily, such as seen in varicosities in the legs. Similarly, if you raise your hand overhead the veins on the surface of the hands with shrink in size, but if you let them hang by your sides they will expand as they fill with blood.
Stenosis is also controversial when it comes to arteries. Heart attacks were once blamed on stenosis of the coronary arteries and many patients elected to have angioplasty and stents put in to improve flow. Unfortunately, it has done nothing to reduce the death rate from heart attacks. Many cases resulted in re-stenosis. Some even caused stroke and heart attacks due to thrombus formation on the old metal stents. If anything, stenosis causes angina, not heart attacks. Heart attacks are typically caused by thrombus that break loose from areas that have been shown to have nothing to do with the stenosis. It has been shown that patients with more than seventy percent stenosis often had no problems.
In adddition, the assesment of stenosis is made while the patient is lying down and anesthetized, in this condition there aren’t any demands on the circulatory system. An artery would have to be severely calcified not to comply at all. In other words, stenosis is a relative term and like angioplasty and stents in coronary arteries venous angioplasty and stents will most likely be subject to the same problems, including re-stenosis.
Nonetheless, the so called liberation procedure appears to be working quite well, and that’s good news for all the MS patients dealing with serious disabilities. But it may work for different reasons other than improving venous stenosis. It may work by siphoning blood from the clogged drainage system of the brain similar to siphoning gas from the tank of a car. Opening the jugular and thoracic veins creates a void, which probably draws blood out of the brain similar to the effect of upright posture on blood flow in the brain. With this in mind, there may be other options for improving venous drainage issues based on the same premise but due to blockage in the vertebral veins not the jugulars. I will discuss it in future posts.
In the mean time, the role of venous drainage issues in causing MS is just the tip of the iceberg. Aging baby boomers, Alzheimer’s and Parkinson’s are the iceberg. MS patients should join forces with AD and PD patients as their conditions may share similar root causes.
During inversion for example, there is a great deal of compliance in the vertebral veins in the spinal canal and the dural sinuses of the brain which have no valves to prevent or check reverse flow, such as those found in the jugular and most other veins. In the extremities, veins expand easily, such as seen in varicosities in the legs. Similarly, if you raise your hand overhead the veins on the surface of the hands with shrink in size, but if you let them hang by your sides they will expand as they fill with blood.
Stenosis is also controversial when it comes to arteries. Heart attacks were once blamed on stenosis of the coronary arteries and many patients elected to have angioplasty and stents put in to improve flow. Unfortunately, it has done nothing to reduce the death rate from heart attacks. Many cases resulted in re-stenosis. Some even caused stroke and heart attacks due to thrombus formation on the old metal stents. If anything, stenosis causes angina, not heart attacks. Heart attacks are typically caused by thrombus that break loose from areas that have been shown to have nothing to do with the stenosis. It has been shown that patients with more than seventy percent stenosis often had no problems.
In adddition, the assesment of stenosis is made while the patient is lying down and anesthetized, in this condition there aren’t any demands on the circulatory system. An artery would have to be severely calcified not to comply at all. In other words, stenosis is a relative term and like angioplasty and stents in coronary arteries venous angioplasty and stents will most likely be subject to the same problems, including re-stenosis.
Nonetheless, the so called liberation procedure appears to be working quite well, and that’s good news for all the MS patients dealing with serious disabilities. But it may work for different reasons other than improving venous stenosis. It may work by siphoning blood from the clogged drainage system of the brain similar to siphoning gas from the tank of a car. Opening the jugular and thoracic veins creates a void, which probably draws blood out of the brain similar to the effect of upright posture on blood flow in the brain. With this in mind, there may be other options for improving venous drainage issues based on the same premise but due to blockage in the vertebral veins not the jugulars. I will discuss it in future posts.
In the mean time, the role of venous drainage issues in causing MS is just the tip of the iceberg. Aging baby boomers, Alzheimer’s and Parkinson’s are the iceberg. MS patients should join forces with AD and PD patients as their conditions may share similar root causes.
Posted in ccsvi, liberation procedure, multiple sclerosis 2 Comments
CCSVI, Iron Deposits, MS and Alzheimer’s
 Recent research using brain scans showed iron deposition in patients with CCSVI and MS. But the iron deposits weren’t found in areas typically associated with hyperintensity signals. Instead, they were found in different but very interesting locations that I won’t go into here. Suffice it to say that sluggish brain circulation can lead to cytotoxic edema, which is a topic I cover thoroughly in my book. Sluggish blood flow causes all types of waste products to accumulate and iron is just one of several well known suspects that can initiate neurodegenerative processes. Other strong suspects include calcium and glutamate. Nonetheless, knowing all this, still doesn’t tell us what the cause of CCSVI and sluggish blood flow is. Furthermore, except for research, it serves no clinical purpose to use brain scans to check for iron deposits as a marker for MS considering the cost and the fact that it does nothing to alter the course of the condition.
Recent research using brain scans showed iron deposition in patients with CCSVI and MS. But the iron deposits weren’t found in areas typically associated with hyperintensity signals. Instead, they were found in different but very interesting locations that I won’t go into here. Suffice it to say that sluggish brain circulation can lead to cytotoxic edema, which is a topic I cover thoroughly in my book. Sluggish blood flow causes all types of waste products to accumulate and iron is just one of several well known suspects that can initiate neurodegenerative processes. Other strong suspects include calcium and glutamate. Nonetheless, knowing all this, still doesn’t tell us what the cause of CCSVI and sluggish blood flow is. Furthermore, except for research, it serves no clinical purpose to use brain scans to check for iron deposits as a marker for MS considering the cost and the fact that it does nothing to alter the course of the condition.What’s more interesting about this recent study on iron depositon is that it cites two other particular studies of interest. The first one from Brain Research, done in 1997, showed similar iron deposition in Alzheimer’s disease, which I cover in my book. The other study is from Functional Neurology, by Dr. Zamboni where it was found that the severity of CCSVI, that is venous drainage issues in the brain, is related to altered CSF hydrodynamics. All three studies corroborate my theory that, in addition to MS, CCSVI similarly causes Alzheimer’s and Parkinson’s diseases. I will be covering cranial hydrodynamics in future posts. I cover the topic thoroughly in my book. Among other things, I believe that CCSVI alters cranial hydrodynamics resulting in either hydrocephalus or Chiari type conditions, but it starts with drainage issues.
Posted in Alzheimer's, ccsvi, liberation procedure, multiple sclerosis, Parkinson's 15 Comments
CCSVI versus Venous Back Jets
Austrian physician, Dr. Alfons Schelling has spent most of his career studying MS. In contrast to Dr. Zamboni, Schelling believes that the supratentorial periventricular lesions that have a predilection for areas surrounding the larger veins in the brain, are caused by venous back jets into the brain. As opposed to stenosis, back jets make sense due to CCSVI when it comes to the MS lesions seen on brain scans.
Dr. Schelling currently maintains that one of the possible sources for the back jets comes from normal cardiorespiratory waves that are transmitted to the brain due to faulty valves in the jugular veins. In addition to Dr. Schelling’s theory, another possible source is trauma, such as whiplash injuries that cause violent back jets of venous blood and cerebrospinal fluid from the cord back into the brain in what is called reverse or inversion flows. Unlike the jugular veins, the vertebral veins and the veins of the brain have no valves to check or prevent back flows. Schelling’s theory makes far more sense in explaining MS lesions but fails to explain the ongoing nature of remissions and exacerbations in MS signs and symptoms.
In contrast to Dr. Schelling, it is my opinion that normal cardiorespiratory waves are not likely to be the source of injuries due to inversion flows except in rare cases. With this in mind, my investigative studies included bats, whales and giraffes because of their exposure to extreme inversion flows. It appears that humans and other mammals developed compensatory mechanisms to deal with normal inversion flows. I cover this in depth in my book. Furthermore, the theory of venous back jets into the brain due to incompetant valves in the jugular veins, likewise fails to explain the peculiar demographics associated with MS the same as CCSVI due to stenosis in jugular routes. In other words, if incompentant jugular valves were the cause, then it follows that people living in southern climates, Asians and Eskimos must have a lower incidence of incompetant valves to explain the lower incidence of MS. This is highly unlikely.
CCSVI due to stenosis, and venous back jets into the brain causing MS lesions are two important new theories regarding neurodegenerative diseases that need further research. Additionally, I would like to offer a third theory similar to CCSVI but not due to venous stenosis. Rather than questionable ultrasound studies, it is based on solid anthropological, pathological and comparative anatomical forensic evidence etched into the bones of the skull, as well as solid physiological evidence from upright Phase Contrast MR scans, and many anecdotal case studies. In addition, I would like to see epidemiological studies done.
I will be discussing the above and more in future posts. For now, my theory has to do with micromechanical plastic strains and deformation of the upper cervical spine and base of the skull causing back pressure against the basement veins and sluggish outflow from the brain.
Dr. Schelling currently maintains that one of the possible sources for the back jets comes from normal cardiorespiratory waves that are transmitted to the brain due to faulty valves in the jugular veins. In addition to Dr. Schelling’s theory, another possible source is trauma, such as whiplash injuries that cause violent back jets of venous blood and cerebrospinal fluid from the cord back into the brain in what is called reverse or inversion flows. Unlike the jugular veins, the vertebral veins and the veins of the brain have no valves to check or prevent back flows. Schelling’s theory makes far more sense in explaining MS lesions but fails to explain the ongoing nature of remissions and exacerbations in MS signs and symptoms.
In contrast to Dr. Schelling, it is my opinion that normal cardiorespiratory waves are not likely to be the source of injuries due to inversion flows except in rare cases. With this in mind, my investigative studies included bats, whales and giraffes because of their exposure to extreme inversion flows. It appears that humans and other mammals developed compensatory mechanisms to deal with normal inversion flows. I cover this in depth in my book. Furthermore, the theory of venous back jets into the brain due to incompetant valves in the jugular veins, likewise fails to explain the peculiar demographics associated with MS the same as CCSVI due to stenosis in jugular routes. In other words, if incompentant jugular valves were the cause, then it follows that people living in southern climates, Asians and Eskimos must have a lower incidence of incompetant valves to explain the lower incidence of MS. This is highly unlikely.
CCSVI due to stenosis, and venous back jets into the brain causing MS lesions are two important new theories regarding neurodegenerative diseases that need further research. Additionally, I would like to offer a third theory similar to CCSVI but not due to venous stenosis. Rather than questionable ultrasound studies, it is based on solid anthropological, pathological and comparative anatomical forensic evidence etched into the bones of the skull, as well as solid physiological evidence from upright Phase Contrast MR scans, and many anecdotal case studies. In addition, I would like to see epidemiological studies done.
I will be discussing the above and more in future posts. For now, my theory has to do with micromechanical plastic strains and deformation of the upper cervical spine and base of the skull causing back pressure against the basement veins and sluggish outflow from the brain.
Posted in ccsvi, liberation procedure, multiple sclerosis 5 Comments
CCSVI due to Stenosis Conflicts with Pathology
Clinically speaking, the types of cases in MS fall into definite, probable and possible categories. The definite cases are defined by areas of demyelination in the brain and cervical cord that show up as hyperintensity signals on scans. In the brain they are usually found in the supratentorial area above the covering over the cerebellum, which is in the bottom compartment of the cranial vault. Furthermore, they are more frequently found in the periventricular areas surrounding the upper chambers of the brain called ventricles. In other words, MS lesions are typically found in the upper compartments of the brain. In contrast to the brain, the lesions can also show up along the flanks of the outside of the cervical cord as opposed to its core. Barring hyperintensity signals, the diagnosis in all other cases of MS remains suspect until all other possibilities are ruled out.
Aside from supratentorial hyperintensity signals the only other significant clinical finding in MS is oligoclonal bands in cerebrospinal fluid taken from the cord. The bands come from gamma globulin breakdown, which is part of the immune system. This is why MS is oftentimes erroneously described as an immunological disease even though there is no solid evidence to substantiate this.
Dr. Zamboni attributes the source of CCSVI to stenosis of veins that the internal jugular veins drain into. Regarding the issue of stenosis, the first point of contention I have, is it that it is hard to imagine how stenosis in much lower cervical and thoracic veins can cause back pressure significant enough to cause the supratentorial periventricular lesions seen in the upper most compartments of the brain in cases with definite MS. If anything, you would expect to find the lesions around the veins in the bottom of the cranial vault. Secondly, it is also hard to explain how stenosis of cervical and thoracic veins cause the oligoclonal bands found in CSF. If it is due to blockage of cervical and thoracic veins causing back pressure against the cord, then there should be more demyelination in the cervical and thoracic cord, which drain into the cervical and thoracic veins as well. Lastly, considering the huge drainage capacity of the vertebral venous system, it is hard to imagine how stenosis of more distant cervical and thoracic veins can cause lesions of MS to show up along the flanks of the cervical cord.
This is just the tip of the iceberg. The role of venous drainage issues in neurodegenerative diseases is much larger than simply MS. I discuss it all in my book The Downside of Upright Posture – The Anatomical Causes of Alzheimer’s, Parkinson’s and Multiple Sclerosis. You can read more about the book on my website uprightdoc.com. Moreover, I think I have a better explanation as to the source of CCSVI, which I will discuss in future posts.
Aside from supratentorial hyperintensity signals the only other significant clinical finding in MS is oligoclonal bands in cerebrospinal fluid taken from the cord. The bands come from gamma globulin breakdown, which is part of the immune system. This is why MS is oftentimes erroneously described as an immunological disease even though there is no solid evidence to substantiate this.
Dr. Zamboni attributes the source of CCSVI to stenosis of veins that the internal jugular veins drain into. Regarding the issue of stenosis, the first point of contention I have, is it that it is hard to imagine how stenosis in much lower cervical and thoracic veins can cause back pressure significant enough to cause the supratentorial periventricular lesions seen in the upper most compartments of the brain in cases with definite MS. If anything, you would expect to find the lesions around the veins in the bottom of the cranial vault. Secondly, it is also hard to explain how stenosis of cervical and thoracic veins cause the oligoclonal bands found in CSF. If it is due to blockage of cervical and thoracic veins causing back pressure against the cord, then there should be more demyelination in the cervical and thoracic cord, which drain into the cervical and thoracic veins as well. Lastly, considering the huge drainage capacity of the vertebral venous system, it is hard to imagine how stenosis of more distant cervical and thoracic veins can cause lesions of MS to show up along the flanks of the cervical cord.
This is just the tip of the iceberg. The role of venous drainage issues in neurodegenerative diseases is much larger than simply MS. I discuss it all in my book The Downside of Upright Posture – The Anatomical Causes of Alzheimer’s, Parkinson’s and Multiple Sclerosis. You can read more about the book on my website uprightdoc.com. Moreover, I think I have a better explanation as to the source of CCSVI, which I will discuss in future posts.
Posted in ccsvi, liberation procedure, multiple sclerosis Leave a comment
CCSVI and the VVP
It was upright posture that caused a forward migration of the foramen magnum in the skull to a place beneath the center and the mass of the brain. The foramen magnum contains the spinal cord. Among other things it can also contain extra venous drainage outlets as well. It’s central location makes for near perfect balance of the head on the neck. It’s particular location also makes the foramen magnum the lowest point inside the cranial vault in the base of the skull.
The condyles of the skull are joints shaped like kidney beans that attach the skull to the first cervical certebral call atlas or C1. They are located along the perimeter of the left and right sides of the formen magnum beneath the skull. The condyles are actually the lowest point in the formen magnum. Picture a sink with drain in the bottom. Typically the bottom of the basin contains a slight depression that contains the drain. The ring of the foramen magnum and the condyles are similar to the depression in the bottom of the basin of the sink.
According to a study by Dr. Dean Falk, an expert physical anthropologist with a background in brain evolution, and others, such as the world renowned Andrew Tobias from Australia, humans and hominids developed additional venous drainage routes to handle the increase in brain blood flow that comes from upright posture. Those extra routes drain the bottom of the cranial vault and empty into the veins of the vertebral venous plexus of the spine.
The extra venous drainage routes tend to be located around the foramen magnum, which as was mentioned above, is the lowest point inside the cranial vault. Some veins actually enter the foramen magnum and exit through openings called the condylar and hypoglossal canals. In fact, there are numerous variations in the drainage system used by humans to empty the bottom of the vault. The subject is complex because it has never been studied in humans in detail. But considering the fact that drainage issues in the skull may lead to answers to finding the cause of neurodegenerative diseases which are some of the most critical and costly health care issues of the day this subject should not be overlooked.
The bottom line, however, is that those extra venous routes, which specifically evolved to handle the increase in brain blood flow that comes from upright posture, as well as to drain the lowest point of the cranial vault, drain into the vertebral venous plexus of the spine, not the internal jugular foramen and veins.
Dr. Zamboni is currently using stents and balloons to open up veins that improve drainage through the internal jugular veins, and possibly other alternative venous pathways as well. Nonetheless, to drain the lowest point of the skull his procedure would have to cause a venous shift upwards toward the jugular foramen and away from its normal flow downwards toward the foramen magnum and alternative outlets located lower down in the bottom of the vault.
While this may work, and it may be the best answer in certain cases, it isn’t the best route for completely draining the lowest point of the cranial vault. The most efficienct route is the one nature intended; that route is into the vertebral venous plexus of the spine not the internal jugular veins. Whatever the cause, the best method to drain the lowest point in the cranial vault would be to remove the source of stenosis and back pressure against the vertebral venous plexus. I’ll address that issue in future posts.
The condyles of the skull are joints shaped like kidney beans that attach the skull to the first cervical certebral call atlas or C1. They are located along the perimeter of the left and right sides of the formen magnum beneath the skull. The condyles are actually the lowest point in the formen magnum. Picture a sink with drain in the bottom. Typically the bottom of the basin contains a slight depression that contains the drain. The ring of the foramen magnum and the condyles are similar to the depression in the bottom of the basin of the sink.
According to a study by Dr. Dean Falk, an expert physical anthropologist with a background in brain evolution, and others, such as the world renowned Andrew Tobias from Australia, humans and hominids developed additional venous drainage routes to handle the increase in brain blood flow that comes from upright posture. Those extra routes drain the bottom of the cranial vault and empty into the veins of the vertebral venous plexus of the spine.
The extra venous drainage routes tend to be located around the foramen magnum, which as was mentioned above, is the lowest point inside the cranial vault. Some veins actually enter the foramen magnum and exit through openings called the condylar and hypoglossal canals. In fact, there are numerous variations in the drainage system used by humans to empty the bottom of the vault. The subject is complex because it has never been studied in humans in detail. But considering the fact that drainage issues in the skull may lead to answers to finding the cause of neurodegenerative diseases which are some of the most critical and costly health care issues of the day this subject should not be overlooked.
The bottom line, however, is that those extra venous routes, which specifically evolved to handle the increase in brain blood flow that comes from upright posture, as well as to drain the lowest point of the cranial vault, drain into the vertebral venous plexus of the spine, not the internal jugular foramen and veins.
Dr. Zamboni is currently using stents and balloons to open up veins that improve drainage through the internal jugular veins, and possibly other alternative venous pathways as well. Nonetheless, to drain the lowest point of the skull his procedure would have to cause a venous shift upwards toward the jugular foramen and away from its normal flow downwards toward the foramen magnum and alternative outlets located lower down in the bottom of the vault.
While this may work, and it may be the best answer in certain cases, it isn’t the best route for completely draining the lowest point of the cranial vault. The most efficienct route is the one nature intended; that route is into the vertebral venous plexus of the spine not the internal jugular veins. Whatever the cause, the best method to drain the lowest point in the cranial vault would be to remove the source of stenosis and back pressure against the vertebral venous plexus. I’ll address that issue in future posts.
Posted in ccsvi, liberation procedure, multiple sclerosis Tagged ccsvi, ms, physcial bioanthropology Leave a comment
CCSVI and MS Demographics
Although I haven’t read the exact studies and what they base their parameters for success on, it appears that Zamboni’s procedure to open up venous drainage in the brain is working fairly well. One of the problems I have with stenosis (which is what Zamboni’s procedure attempts to correct) causing MS is that it fails to explain the peculiar demographics associated with MS. His explanation as to the cause of the lesions is likewise lacking but that’s an entirely different subject.
MS is not an equal opportunity condition. Not only is it selective about the areas of the brain and cord it targets, but it also shows gender, geographical and racial biases. That is, people living in southern climates have a lower incidence of MS than those living in northern climates and the incidence of MS in tropical climates is very low. But if you move a child from a northern to a southern climate their incidence drops to match the level of those of the southern climate. On the other hand, moving adults to southern climates has no impact on incidence.
Oddly enough, many adults with MS claim to feel better at higher altitudes where the weather is colder and more similar to northern latitude climates, but the effects of gravity is less and barometric pressure is lower and more similar to southern latitude climates. It seems that the higher MS patients go, the better they feel. This is interesting because northern latitudes are associated with cold air masses and higher barometric conditions. Conversely, higher altitudes are associated with lower barometric pressure.
The most peculiar aspect about MS, however, is that Asians have a very low incidence of MS regardless of where they live, and Eskimos living in even the most extreme northern climates never get MS. Does this mean that people living in tropical and southern climates, Asians and Eskimos have a lower incidence of venous stenosis? This is highly doubtful.
Rather than venous stenosis per se, it is my opinion that gender and racial differences are probably related to design issues in the skull due to upright posture that can affect venous drainage. The higher incidence of MS in northern climates are associated with a much greater probability of winter related whiplash type trauma that can injure and subsequently impact venous drainage outlets in the base of the skull and upper cervical spine.
In this regard, studies continue to show a highly suspicious connection between MS and trauma, as well as dementia and Parkinson’s in adults. It’s just common sense that young people are more susceptible to whiplash type traumas to the head and neck while the bones, brain and cord are still growing.
In addition to venous drainage issues, I also discuss the bigger picture of cranial hydrodynamics and the likely role of upright posture and the design of the skull, spine and circulatory system of the brain in neurodegenerative diseases in my book The Dowside of Upright Posture – The Anatomical Causes of Alzheimer’s, Parkinson’s and Multiple Sclerosis.
MS is not an equal opportunity condition. Not only is it selective about the areas of the brain and cord it targets, but it also shows gender, geographical and racial biases. That is, people living in southern climates have a lower incidence of MS than those living in northern climates and the incidence of MS in tropical climates is very low. But if you move a child from a northern to a southern climate their incidence drops to match the level of those of the southern climate. On the other hand, moving adults to southern climates has no impact on incidence.
Oddly enough, many adults with MS claim to feel better at higher altitudes where the weather is colder and more similar to northern latitude climates, but the effects of gravity is less and barometric pressure is lower and more similar to southern latitude climates. It seems that the higher MS patients go, the better they feel. This is interesting because northern latitudes are associated with cold air masses and higher barometric conditions. Conversely, higher altitudes are associated with lower barometric pressure.
The most peculiar aspect about MS, however, is that Asians have a very low incidence of MS regardless of where they live, and Eskimos living in even the most extreme northern climates never get MS. Does this mean that people living in tropical and southern climates, Asians and Eskimos have a lower incidence of venous stenosis? This is highly doubtful.
Rather than venous stenosis per se, it is my opinion that gender and racial differences are probably related to design issues in the skull due to upright posture that can affect venous drainage. The higher incidence of MS in northern climates are associated with a much greater probability of winter related whiplash type trauma that can injure and subsequently impact venous drainage outlets in the base of the skull and upper cervical spine.
In this regard, studies continue to show a highly suspicious connection between MS and trauma, as well as dementia and Parkinson’s in adults. It’s just common sense that young people are more susceptible to whiplash type traumas to the head and neck while the bones, brain and cord are still growing.
In addition to venous drainage issues, I also discuss the bigger picture of cranial hydrodynamics and the likely role of upright posture and the design of the skull, spine and circulatory system of the brain in neurodegenerative diseases in my book The Dowside of Upright Posture – The Anatomical Causes of Alzheimer’s, Parkinson’s and Multiple Sclerosis.
Posted in ccsvi, liberation procedure, multiple sclerosis 2 Comments
Chronic Cerebrospinal Venous Insufficiency
There has been a great deal of excitment, and rightly so, over the work of Dr. Zamboni and others using venous stents and balloons to open drainage routes of the brain and improve the symptoms of many multiple sclerosis patients. He attributes the cause of MS to chronic cerebrospinal venous insufficiency. The role of venous drainage issues in neurodegenerative diseases, however, is not new. I first started writing about it in 1987. What’s more, MS is just the tip of the iceberg. Aging baby boomers, Alzheimer’s and Parkinson’s diseases are the iceberg.
While I agree in part with Dr. Zamboni’s theory on the role of venous drainage issues in neurodegenerative diseases, I have some points of contention I would like to discuss. I will discuss the first issue in my next post. It has to do with the unusual demographics associated with MS, which Zamboni’s theory fails to explain. I have several other issues with his theory that I will be discussing in future posts as well. On the other hand, Dr. Zamboni’s procedure may have far greater implications for its use than just MS. Furthermore, it lends credence to chiropractic claims of similar results in treating certain cases of neurodegenerative diseases using far less invasive and costly procedures, but based on a similar theory of venous drainage.
While I agree in part with Dr. Zamboni’s theory on the role of venous drainage issues in neurodegenerative diseases, I have some points of contention I would like to discuss. I will discuss the first issue in my next post. It has to do with the unusual demographics associated with MS, which Zamboni’s theory fails to explain. I have several other issues with his theory that I will be discussing in future posts as well. On the other hand, Dr. Zamboni’s procedure may have far greater implications for its use than just MS. Furthermore, it lends credence to chiropractic claims of similar results in treating certain cases of neurodegenerative diseases using far less invasive and costly procedures, but based on a similar theory of venous drainage.
Upright Posture and Neurodegererative Diseases
Upright posture: It’s what defines us as humans and no other body does it better. Not only do we stand perfectly upright, but we walk about in a most efficient way that required significant evolutionary changes from head to foot.
Anthropologists suggest several different possible scenarios as to what environmental factors might have triggered upright posture and bipedalism in humans and hominids. The truth is, we don’t know. We can only guess, but by all accounts it was a behavioral decision on the part of the brain and that fateful decision led to some amazing anatomical and physiological changes.
For the most part the those changes were beneficial, especially for the brain. In fact, anthropologists attribute the large size of the human brain to the increase in brain blood flow caused by upright posture, as well as an enhanced cooling system. Some even believe that enhanced cooling had a greater impact on the increase in size of the brain than the increase in blood flow. They call it the radiator theory.
This blog will address some critical health care issues that I believe to be associated with upright posture. It will start with neurodegeneraive diseases because conditions, such as Alzheimer’s, Parkinson’s and multiple sclerosis are some of the most critical and costly health care issues we face in the industrialized world today. Yet, despite billions of dollars and decades in research, we still don’t have a clue as to what causes them. This is important because knowing the cause is the key to better treatment and possibly even prevention.
In the final analysis, I am going to present a strong case for doing further research into a brand new theory that has to do with upright posture and the unique design of the human skull, spine and circulatory system of the brain and their role in cranial hydrodynamics. Faulty cranial fluid mechanics may be the root cause of many neurodegenerative diseases.
Anthropologists suggest several different possible scenarios as to what environmental factors might have triggered upright posture and bipedalism in humans and hominids. The truth is, we don’t know. We can only guess, but by all accounts it was a behavioral decision on the part of the brain and that fateful decision led to some amazing anatomical and physiological changes.
For the most part the those changes were beneficial, especially for the brain. In fact, anthropologists attribute the large size of the human brain to the increase in brain blood flow caused by upright posture, as well as an enhanced cooling system. Some even believe that enhanced cooling had a greater impact on the increase in size of the brain than the increase in blood flow. They call it the radiator theory.
This blog will address some critical health care issues that I believe to be associated with upright posture. It will start with neurodegeneraive diseases because conditions, such as Alzheimer’s, Parkinson’s and multiple sclerosis are some of the most critical and costly health care issues we face in the industrialized world today. Yet, despite billions of dollars and decades in research, we still don’t have a clue as to what causes them. This is important because knowing the cause is the key to better treatment and possibly even prevention.
In the final analysis, I am going to present a strong case for doing further research into a brand new theory that has to do with upright posture and the unique design of the human skull, spine and circulatory system of the brain and their role in cranial hydrodynamics. Faulty cranial fluid mechanics may be the root cause of many neurodegenerative diseases.
Posted in Alzheimer's, multiple sclerosis, Parkinson's, physical anthropology Tagged Alzheimer's, multiple sclerosis, Parkinson's 4 Comments










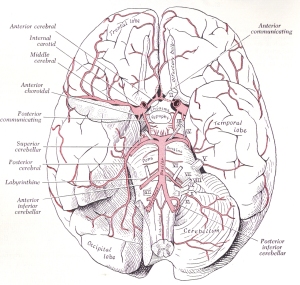




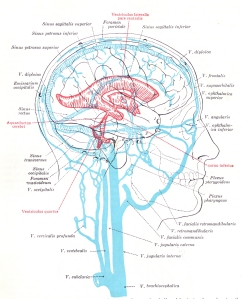
No comments:
Post a Comment