 KCUMB Students
KCUMB Students
"Big Robbins" -- Infectious
Lectures follow TextbookQUIZBANK -- Infectious disease (all)
Microbe Library -- American Society for Microbiology teaching resourcesTHE 17 NEGLECTED TROPICAL DISEASES (NTD's): Only lack of money / interest prevents the 1 billion people affected with one of more of these from being treated effectively.
- Chagas disease
- African trypanosomiasis (sleeping sickness)
- Leishmaniasis
- Buruli ulcer
- Leprosy
- Trachoma
- Yaws
- Cysticercosis
- Dracunculiasis (guinea worm)
- Echinococcosis
- The foodborne trematodiases (clonorchiasis, fascioliasis, opisthorchiasis, paragonimiasis)
- Lymphatic filariasis
- Onchocerciasis
- Schistosomiasis
- Soil-transmitted helminths (Ascaris, whipworm, the hookworms, I'd have added strongyloides)
- Dengue and Chikungunya
- Rabies
CDC'S RECOMMENDATIONS FOR ADULT IMMUNIZATION: JAMA
288: 2258, 2002. Health advice and immunization (hepatitis A, hepatitis B, typhoid, cholera, rabies

, meningococcus, Japanese encephalitis, BCG, Lyme disease

, tick encephalitis) for those planning to go overseas: NEJM
342: 1716, 2000. Infectious diseases for the team doctor: JAMA
271: 862, 1994; Ann. Int. Med.
122: 283, 1995. The main ones to worry about are the viruses, but AIDS transmission in sports seems most unlikely. Future physicians: Before you start practice in the community, be sure you know how to recognize, and have a fair index of suspicion for, each of the following infections, which might be introduced by bioterrorists:
- anthrax
 **
**
- botulism
 **
**
- brucellosis
 **
**
- plague

- Q-fever
 **
**
- smallpox

- staph enterotoxin B

- tularemia
 **
**
- viral encephalitis **
- viral hemorrhagic fever
** Right or wrong, each of these was weaponized by the US at recently at 1969 (JAMA 278: 412, 1997). In the U.S., we are seldom reminded that the Japanese probably used germ warfare (anthrax , plague
, plague , others) on at least 11 cities during WWII. It is well-established that they conducted atrocious germ-warfare experiments on thousands of human beings at Unit 731 (Lancet 360: 628, 2002). And the Aum Shinri Kyo cult in Japan, which released sarin gas into the subway, had anthrax
, others) on at least 11 cities during WWII. It is well-established that they conducted atrocious germ-warfare experiments on thousands of human beings at Unit 731 (Lancet 360: 628, 2002). And the Aum Shinri Kyo cult in Japan, which released sarin gas into the subway, had anthrax and Q-fever
and Q-fever weapons as well. * The current Category A agents (lethal and easily deployed as weapons) are anthrax
weapons as well. * The current Category A agents (lethal and easily deployed as weapons) are anthrax , plague
, plague , tularemia
, tularemia , smallpox
, smallpox , viral hemorrhagic fever, and botulinum
, viral hemorrhagic fever, and botulinum toxin.
toxin.
Learning Objectives: Viruses
NOTE: This unit begins with a focus on the common, whole-body virus infections. We will study hepatitis viruses, skin viruses, brain viruses, and retroviruses in systemic pathology. Define, and correctly use, the following terms:
commensal
endemic
epidemic
epizootic
fomites
hyperinfection
inclusion
infection
infestation
lower respiratory infection
lytic infection
nosocomial infection
pandemic
parasite
provirus
saprophyte
superinfection
symbiont
Tzanck smear
upper respiratory infection
vector
viremia
zoonosis
Explain why it is simplistic to think of a particular microbe as the single, sufficient "cause" of a particular clinical problem. Give some examples, and some exceptions. Mention the essential features, and give the names and sizes of the largest and smallest pathogenic human viruses. Mention the four phases of the virus cycle. Explain how viruses do us harm at the cellular level, and give examples. Given the name of a virus, recall its family and nucleic acid type, and whether (and where) it produces inclusion bodies

. (* This is a reasonable objective, Doctor; people will be asking you to do this for the rest of your life.) Describe the essential features and important complications of the following viral illnesses:
cytomegalic inclusion disease
Epstein-Barr virus infection
herpes simplex 1 & 2
& 2
mumps
measles
rubella
smallpox
varicella-zoster
Describe the essential pathology of the common cold, and mention the viruses that produce it. Mention the other viruses that produce respiratory infections, the distinctive features of each, and other clinical syndromes they can produce. Name the non-virus that is a very important cause of "chest colds". List the three important agents of true viral gastroenteritis. Describe the common features of arbovirus infections, the nature of "hemorrhagic fevers", and the distinctive features of yellow fever, dengue, and Lassa fever. Recall the numbered strain of human papillomavirus that causes most simple warts, and the two strains most strongly linked to cancer of the cervix. Explain current thinking about chronic fatigue syndrome, and tell when you might make this diagnosis. Discuss the basic biology of chlamydia

, rickettsia, and mycoplasma. Tell how they are like familiar bacteria, and how they differ from them and from one another. Recognize those viral diseases that could theoretically be eradicated, and mention impediments to this. Recognize and distinguish the various chlamydial

diseases, mentioning their distinctive features. Explain why it is difficult to eradicate chlamydial infections. Name the agents, vectors, and pathologic and clinical features of typhus

, ehrlichiosis

, Rocky Mountain spotted fever

, scrub typhus, and Q-fever

. Mention the major mycoplasmal diseases, and the distinctive features of a mycoplasmal respiratory infection. Give the classical synonyms for each disease in this unit. Recognize the following under the microscope:
cytomegalic inclusion disease cell
herpes cell
measles giant cell (epithelial, Warthin-Finkeldey)
giant cell (epithelial, Warthin-Finkeldey)
Negri bodies
Parvo B19 cells
adenovirus smudge cells (obvious case)
smudge cells (obvious case)
atypical lymphocytes of infectious mononucleosis
NOTE: In spite of what anybody else might tell you, prions (the agents of kuru, scrapie, Creutzfeldt-Jakob, and so forth) are
not viruses ("slow" or otherwise). There's no longer any reasonable doubt. More about prions under "CNS".
INTRODUCING THE INFECTIOUS DISEASES
Since ancient times, physicians have known that many diseases are transmissible, but because of the subtle and idiosyncratic ways in which infections seem to travel, the early-modern physicians thought the responsible particles must be much smaller than our cells (correct) and closer in size to atoms (not correct). Virchow wondered whether the bacteria that he often saw in infections were the cause or a side-effect, but eventually came to accept Pasteur's demonstration of their infectious nature. If you have not had "Med Micro", don't worry. We are concerned with what these organisms do to people, rather than details of their biology. Everyone in the class will probably want to skim the section of a good pathology book to review basic microbiology and tissue reactions. The study of infectious disease is especially interesting because the etiologies of most of these diseases is clear -- damage by an invader. And if the invaders can be killed, the disease can be arrested. Today, only a few fools and crooks deny that micro-organisms cause disease. Yet the microbe is seldom the whole story or the "single" cause. Most infectious agents are, in some sense, opportunists ("secondary invaders"). Often, the chink in the host's armor is some personal characteristic. M. tuberculosis thrives on malnutrition and alcoholism. Staph aureus
thrives on malnutrition and alcoholism. Staph aureus takes advantage of dirt and body hair. Propionibacterium acnes flourishes in a milieu of chocolate and testosterone. Folk wisdom relates the common cold to body chilling. Athlete's foot fungus likes if when we don't dry between our toes. Etc., etc., etc. Often, known immune deficiency (congenital, acquired, iatrogenic) provides the portal. We all know the dread infections seen in patients on chemotherapy, by organisms once considered "non-pathogens". The Epstein-Barr virus
takes advantage of dirt and body hair. Propionibacterium acnes flourishes in a milieu of chocolate and testosterone. Folk wisdom relates the common cold to body chilling. Athlete's foot fungus likes if when we don't dry between our toes. Etc., etc., etc. Often, known immune deficiency (congenital, acquired, iatrogenic) provides the portal. We all know the dread infections seen in patients on chemotherapy, by organisms once considered "non-pathogens". The Epstein-Barr virus causes infectious mono (if that) in healthy people, but causes cancer in AIDS victims and boys with X-linked immunodeficiency. Patients given glucocorticoids often have major problems with superficial fungi (ringworm), and worse. Diabetics have ineffective neutrophils and high glucose, facts that make them vulnerable to Candida
causes infectious mono (if that) in healthy people, but causes cancer in AIDS victims and boys with X-linked immunodeficiency. Patients given glucocorticoids often have major problems with superficial fungi (ringworm), and worse. Diabetics have ineffective neutrophils and high glucose, facts that make them vulnerable to Candida infections. Etc., etc. Often, therapy itself provides the gateway for the infectious agent. Candida
infections. Etc., etc. Often, therapy itself provides the gateway for the infectious agent. Candida and C. difficile, normally commensal organisms, thrive when antibiotics kill off their microbiological competitors. Candida flourishes in intravenous hyperalimentation catheters, E. coli predictably infects bladders with indwelling catheters. Staph epidermidis
and C. difficile, normally commensal organisms, thrive when antibiotics kill off their microbiological competitors. Candida flourishes in intravenous hyperalimentation catheters, E. coli predictably infects bladders with indwelling catheters. Staph epidermidis from a blood culture is no joke if it's growing on a prosthetic heart valve. Etc. And for many (if not most) organisms, it is often unclear why one person who meets the microbe becomes very sick, and the next person is spared. A Bergey's of potentially deadly bacteria can be found in most people's normal flora. The polio
from a blood culture is no joke if it's growing on a prosthetic heart valve. Etc. And for many (if not most) organisms, it is often unclear why one person who meets the microbe becomes very sick, and the next person is spared. A Bergey's of potentially deadly bacteria can be found in most people's normal flora. The polio virus usually causes only a GI upset (if that), and only a few people go on to become paralyzed. Histoplasmosis
virus usually causes only a GI upset (if that), and only a few people go on to become paralyzed. Histoplasmosis is usually trivial, but sometimes overwhelms a person who was in robust good health. . AIDS only gets transmitted during the most intimate body-fluid sharing. During Ebola
is usually trivial, but sometimes overwhelms a person who was in robust good health. . AIDS only gets transmitted during the most intimate body-fluid sharing. During Ebola outbreaks, mortality is very high but some people's illness is only subclinical. The manifestations of Lyme disease
outbreaks, mortality is very high but some people's illness is only subclinical. The manifestations of Lyme disease are protean and unpredictable. And so forth. However, a few organisms, when found, always indicate disease. If you get plague bacillus
are protean and unpredictable. And so forth. However, a few organisms, when found, always indicate disease. If you get plague bacillus or rabies
or rabies virus into your system, and don't take prophylactic treatment, you're going to get plague / rabies, period. So far as we know, there are no false-positive PCR's for AIDS. If you drink a milk-shake laced with staphylococcal enterotoxin B
virus into your system, and don't take prophylactic treatment, you're going to get plague / rabies, period. So far as we know, there are no false-positive PCR's for AIDS. If you drink a milk-shake laced with staphylococcal enterotoxin B , you're going to get food poisoning.
, you're going to get food poisoning.
Bug terminology: Symbiont: The organism and its host have a mutually advantageous arrangement (mitochondria producing ATP, E. coli producing vitamin K, in exchange for room & board) Commensal: The organism does the host no good and no harm (worthless bugs in the gut, hepatitis B carrier) Parasite: The organism thrives by actually doing harm to the host (i.e., the pathogenic micro-organisms) Saprophyte: The organism lives off dead stuff (i.e., fungi that thrive only in the hair, nails, or dead keratin layer of the skin) Infection: The parasite or saprophyte is making somebody sick. Infestation: A commensal, parasite, or saprophyte has been detected, other than what most people carry, whether or not somebody is sick. Superinfection: An infection that results because tissues are made vulnerable by another infection. Hyperinfection: Orders of magnitude more infectious agents than you "should" have, because of a fundamental change in your relationship with your parasite. (The prime example is strongyloidiasis, where the worm changes its life cycle in the immunosuppressed). Vector: A multicellular animal (usually an arthropod) that transmits an infectious micro-organism. Fomites: Inanimate objects that carry infectious organisms. (This is why we care whether our silverware looks clean....) Carrier: A clinically healthy person who is shedding an infectious organism, and can make others sick. Nosocomial infection: A hospital-acquired infection. Uh-oh. Hospital pathogens are the result of decades of selection for antibiotic-resistance and the ability to infect the very-sick.... Epidemic: An outbreak of infectious disease. The origin of epidemics in Darwin's world: Science 257: 1073, 1992. Endemic: A never-ending epidemic Pandemic: An epidemic involving the whole world Zoonosis: A disease contracted from animals (ZOE-uh-NO-sis) Epizootic: An epidemic among animals (EP-uh-zoe-OTT-ick)
* You will learn from the clinicians how to test for the infections disease, and how to interpret their results. Sometimes you can diagnose disease based on the finding of a particular organism (for example, F. tularensis on any culture, or N. fowleri visualized in spinal fluid) or antibody pattern (for example, a positive Western blot for HIV-1). On other occasions, a positive result may be misleading (for example, Staph epidermidis from a blood culture contaminated by skin flora, a single high antistreptolysin-O titer), or a negative result may not rule out infection (i.e., negative blood cultures in a patient with suspected endocarditis previously treated "empirically" with antibiotics).
from a blood culture contaminated by skin flora, a single high antistreptolysin-O titer), or a negative result may not rule out infection (i.e., negative blood cultures in a patient with suspected endocarditis previously treated "empirically" with antibiotics).
You already know Koch's postulates. Today, the final "fifth postulate", which establishes the micro-organism as agent of the disease, is the demonstration of a virulence gene. * We suggest you ignore R&F's "Pathologist's Criteria for Establishing a Micro-Organism as the Cause of a Disease or Lesion". If followed to the letter, Russell bodies would be the cause of syphilis . Obviously, pathologist and microbiologist must work together.
. Obviously, pathologist and microbiologist must work together.
INTRODUCING THE VIRUSES
* I kissed the pretty brown-eyed cow
Who gives me milk and cheese;
I'm lying in my nursery now
With hoof-and-mouth disease. -- Sol Weinstein c. 1966
Viruses are probably escaped eukaryotic genes, with protein coats and able to commandeer eukaryotic cells to make copies of themselves. Viruses are the most frequent causes of human illnesses. The largest virus worth remembering is the smallpox virus (0.2-0.3 microns). The smallest human pathogen is probably the poliovirus
virus (0.2-0.3 microns). The smallest human pathogen is probably the poliovirus (0.028 microns). The infectious particle itself is called a virion. The protein-based coat is the capsid, which surrounds nucleic acid (DNA or RNA, never both). Each virus must (1) attach to the cell, (2) penetrate it, (3) un-coat, and (4) replicate. These stages together constitute the virus cycle. An "eclipse phase" almost always occurs between un-coating and replication; a virus integrated into the host genome, able to replicate with the dividing cell, is a provirus. Viremia means viruses in the bloodstream. Except for some respiratory viruses, all viruses probably travel via the blood. As with any infection, it is a mistake to think of a single virus causing a single clinical syndrome.
(0.028 microns). The infectious particle itself is called a virion. The protein-based coat is the capsid, which surrounds nucleic acid (DNA or RNA, never both). Each virus must (1) attach to the cell, (2) penetrate it, (3) un-coat, and (4) replicate. These stages together constitute the virus cycle. An "eclipse phase" almost always occurs between un-coating and replication; a virus integrated into the host genome, able to replicate with the dividing cell, is a provirus. Viremia means viruses in the bloodstream. Except for some respiratory viruses, all viruses probably travel via the blood. As with any infection, it is a mistake to think of a single virus causing a single clinical syndrome.
Here is a simplified taxonomy of the viruses mentioned in this unit (and a few others): Double-stranded DNA viruses Adenovirus family Hepadnavirus family
Herpes viruses
Cytomegalovirus
Epstein-Barr
Herpes simplex I
Herpes simplex II
Human herpes virus 6
Human herpes virus 8
Herpes zoster / chickenpox
Papovavirus family
Human papillomavirus
JC virus (PML, brain disease)
Poxvirus family Molluscum contagiosum
Smallpox
Smallpox vaccine ("vaccinia")
RNA viruses Reovirus family Rotavirus (sporadic viral gastroenteritis)
Coronavirus family
Orthomyxovirus family
Picornavirus family * Calicivirus subfamily Hepatitis E (discovery Science 247: 1335, 1990; epidemic Lancet 338: 783, 1991)
Winter vomiting viruses (Norwalk / norovirus, others; Norovirus NEJM 361: 1776, 2009)
Enterovirus subfamily Coxsackie A and B
and B
Echovirus
Poliovirus
Many others
Hepatitis A
* Hoof & mouth disease (animals, see above) Rhinovirus subfamily
Paramyxovirus family Measles
Mumps
Parainfluenza
Respiratory syncytial virus
* Metapneumovirus (another common children's chest cold virus: Nat. Med. 7: 719, 2001); now the most common NEJM 350: 431 & 443, 2004; most kids who need to go into the hospital are previously healthy NEJM 368: 633, 2013.
Retrovirus family HIV-1 & 2 and their kin
HTLV I & II (see NEJM 326: 374, 1992)
Animal tumor viruses (many)
Togavirus family Rubella
Hepatitis C (a flavivirus; discovery Science 244: 359, 1989)
Hepatitis G (Science 271: 505, 1996) and GC (three of these, discovered 1995; Lancet 345: 1453, 1995)
"Arboviruses" (toga-, flavi-, arena-, bunya-, reo-, filo-) Arbovirus encephalitis viruses
Colorado tick fever
Dengue family
Regional hemorrhagic fevers
Yellow fever
Hantavirus (once "Navajo pneumonia", others; see Science 260: 1579, 1993; Science 261: 680, 1993; NEJM 330: 751, 1994)
West Nile Virus (pathology Am. J. Clin. Path. 119: 749, 2003)
Other Parvovirus
Rabies virus
virus
* A rule that works most of the time: DNA viruses replicate in the nucleus, and RNA viruses replicate in the cytoplasm.
Depending on their type, viruses do us harm by: (1) destroying our cells as their progeny are released ("lytic infection", typical of herpes viruses , smallpox
, smallpox ); (2) rendering infected cells non-functional (HIV, others); (3) exciting cell-mediated immunity, which destroys otherwise-healthy cells that happen to be infected by the virus (hepatitis B, infectious mononucleosis). (4) causing cell overgrowth, which may be unsightly (warts, molluscum), a fertile ground of carcinogenesis (Epstein-Barr virus
); (2) rendering infected cells non-functional (HIV, others); (3) exciting cell-mediated immunity, which destroys otherwise-healthy cells that happen to be infected by the virus (hepatitis B, infectious mononucleosis). (4) causing cell overgrowth, which may be unsightly (warts, molluscum), a fertile ground of carcinogenesis (Epstein-Barr virus in Africa), or full-blown malignancy (some human papillomavirus infections).
in Africa), or full-blown malignancy (some human papillomavirus infections). NOTE: Some viruses promote also cell fusion; we don't know if this is bad for us. Measles and herpes (simplex
and herpes (simplex & zoster
& zoster ) produce picturesque giant cell formation; the nuclei, loaded with visible virus aggregates, will tell you these are not granulomas. Multinucleated brain microglial cells are a marker for AIDS.
) produce picturesque giant cell formation; the nuclei, loaded with visible virus aggregates, will tell you these are not granulomas. Multinucleated brain microglial cells are a marker for AIDS.
Like their attacks, our defenses against viruses are varied. Neutralizing antibodies (i.e., the kind induced by vaccines) prevent or eliminate viral infection by binding to the viruses themselves. Cell-mediated immunity and interferon are also important. Immunity to most viruses is quite durable, and apart from latent infections, it's unusual to get infected twice by the same virus. Viral inclusions are aggregates of virus proteins, visible by light microscopy. These assist greatly with the histologic diagnosis of viral disease. The viral inclusions that are most worth remembering: Intranuclear ("Cowdry A" and "Cowdry B"; don't worry about the distinction) Adenovirus ("smudge cells") * BK virus ("decoy cells", one huge bluish inclusion) Cytomegalovirus
* BK virus ("decoy cells", one huge bluish inclusion) Cytomegalovirus (one large, clearly-defined) Herpes simplex I
(one large, clearly-defined) Herpes simplex I & II
& II (one large, clear, + multinucleate) Herpes zoster
(one large, clear, + multinucleate) Herpes zoster (same as simplex) Measles
(same as simplex) Measles (in measles giant cells, and SSPE) Molluscum contagiosum (cells are replaced by masses of poxvirus called "molluscum bodies") JC papovavirus ("progressive multifocal leukodystrophy" of the brain) Parvo B19
(in measles giant cells, and SSPE) Molluscum contagiosum (cells are replaced by masses of poxvirus called "molluscum bodies") JC papovavirus ("progressive multifocal leukodystrophy" of the brain) Parvo B19 (one huge reddish inclusion)
(one huge reddish inclusion)
Intracytoplasmic Cytomegalovirus (many small) Rabies
(many small) Rabies ("Negri bodies" in neurons) Molluscum contagiosum ("molluscum bodies" in skin) Smallpox
("Negri bodies" in neurons) Molluscum contagiosum ("molluscum bodies" in skin) Smallpox (* "Guarnieri bodies" in skin) Chlamydia
(* "Guarnieri bodies" in skin) Chlamydia (not really viruses....)
(not really viruses....)
Remember that the typical inflammatory infiltrate evoked by viruses is composed of lymphocytes and macrophages.
 Viral inclusions
Viral inclusions
Lung pathology series
Dr. Warnock's Collection VIRUS RESPIRATORY DISORDERS
These contagious diseases, typically spread by droplets, range from "the common cold" to deadly viral pneumonitis. By convention, upper respiratory infections involve the nose, sinuses, throat, tonsils, and/or middle ear. The anatomy is variable, and sinuses are often occluded. * CT scanners see NEJM 330: 25, 1994.
* Dost thou pray to thy god that thy nose may not run? Nay, foolish one! Thou blowest thy nose on the sleeve of thy toga!
Lower respiratory infections involve the larynx, trachea, bronchi, alveoli ("viral pneumonitis", "chest cold"), and/or pleura.
The anatomic pathology of a cold is what you'd expect. If you were to biopsy the nasal mucosa in a common cold, you'd see abundant mucus production and edema (hence, watery snot), and a preponderance of lymphocytes and plasma cells. Neutrophils appear (and the snot turns yellow) when necrotic tissue sloughs. (The "pop" wisdom is that the yellow mucus that occurs late in a cold represents "bacterial superinfection"; do your own gram stain and find out for yourself.) In a typical viral interstitial pneumonitis, inflammatory cells fill the alveolar septa, but without entering the alveolar spaces. (Absence of inflammatory exudate in the alveolar spaces distinguishes "pneumonitis" from "pneumonia"; the distinction often blurs in practice.) In fatal chest colds, we see similar changes, but with more florid cell damage. Death results when the airways are sufficiently damaged to allow fibrin to escape and block air flow and exchange. Failure of the airway to clear its secretions invites bacterial superinfection, with a neutrophilic response.
A host of different viruses can be involved. Rhinoviruses (>100 species), the usual agents of "the common cold" ("coryza", etc.), attack the upper respiratory tract directly. They supposedly do not cause lower respiratory infections. * "Stress & the common cold": NEJM 325: 606, 1991. Steam inhalation, Mom's favorite aid for the common cold, is worthless (JAMA 271: 1112, 1994). * Pleconaril, the novel anti-viral agent that seems to be effective against picornaviruses (J. Inf. Dis. 181: 20, 2000) including the common cold (Med. J. Aust. 175: 112, 2001). Safety concerns have prevented its widespread use. Echinacea fails to help the common cold -- the conclusion of a very elaborate, very expensive study (NEJM 353: 337 & 341, 2005) which left the reviewers asking, "How much longer will we continue funding studies of folk remedies when there is no plausable mechanism and no demonstrable active substance?"
Coronaviruses (many species) are the second most common cause of the common cold. The classic coronaviruses supposedly do not cause lower respiratory infections, either. SARS is of course a novel coronavirus infection (NEJM 348: 1977 & 1995, 2003). Adenovirus (many species) can produce common colds, chest colds, red eyes ("epidemic keratoconjunctivitis"), and/or GI upsets. Necrosis is typical of the most severe adenovirus pneumonitis, which can be fatal (Arch. Path. Lab. Med. 113: 1349, 1989; a bad case in an immunocompetent adult, which I suspect actually happens fairly often Am. J. Med. Sci. 285: 285, 2003; the military must think so also since it vaccinated against adenovirus from 1971 to 1999 and after cessation, the disease re-emerged especially in recruits: J. Inf. Dis. 196: 67, 2007). Nowadays it doesn't seem any rougher than other chest colds for healthy folks (J. Inf. Dis. 203: 1388, 2012). Pathologists notice enlarged, basophilic nuclei without any texture; these denote "smudge cells", typical of adenovirus infection. * Adenovirus hepatitis after bone marrow transplant: Arch. Path. Lab. Med. 127: 246, 2003.* The other type of nuclear change seen in adenovirus infections is a realtively small central eosinophilic inclusion surrounded by a clear zone.Disseminated adenovirus as cause of death in immune compromise: Am. J. Clin. Path. 120: 575, 2003. * Procalcitonin, a marker for bacterial infection (!), to guide antibiotic administration / cessation in folks with chest colds: JAMA 309: 717, 2013.
{24371} adenovirus lung infection; low power shot just shows thickening of the alveolar septa
{24374} adenovirus lung infection; hyaline membranes; no visible smudge cells but lots of lymphocytes
{01743} smudge cell, schematic diagram
Influenza (A, B, C; name is Spanish for "bad influence") is primarily an infection of any and all parts of the respiratory tree. Update Nat. Med. 9: S-83, 2004 Systemic complaints begin 1-2 days after exposure, with fever, headache, myalgias, and fatigue. In severe cases, necrotizing lesions of the airway appear. Staphylococcal superinfection is common and deadly. The anatomic pathology in fatal cases is diffuse alveolar damage with widespread hemorrhage (Am. J. Path. 172: 1155, 2008). Mutants vary their hemagglutinin (H) and neuraminidase (N) antigens, producing a new strain every few years. Influenza A: Pandemic influenza Influenza B: Epidemics; children badly affected Influenza C: Sporadic, upper respiratory infections Tens of thousands of people die of influenza during every epidemic. The "flu shot" works great for kids but only produces a 30% or so reduction in cases when used in nursing homes (abstract 92357998, from Italy). You already know about the 1918 epidemic of "Spanish flu", which caused the greatest number of deaths of any acute infectious disease outbreak. Forty million dead is a conservative estimate (Nat. Med. 10: S-83, 2004). The mutation that triggered it: Science 293: 1842, 2001. * The dread chicken flu in Hong Kong: Lancet 351: 467 & 472, 1998. Evolution of new flu strains is blamed on agricultural practices in which chickens and pigs are raised together. * Recovering the virus and its genes from bodies frozen in the Alaskan permafrost: Proc. Nat. Acad. Sci. 96: 1651, 1999. This is from the Armed Forces Institute of Pathology team that succeeded in recovering the virus, which was also able simply to make the recovery from old glass autopsy slides. The leader of the rival group, which sought unsuccessfully to recover the virus from a Norwegian burial, wrote the science-adventure book "Hunting the 1918 Flu" (review NEJM 250: 352, 2004).
superinfection is common and deadly. The anatomic pathology in fatal cases is diffuse alveolar damage with widespread hemorrhage (Am. J. Path. 172: 1155, 2008). Mutants vary their hemagglutinin (H) and neuraminidase (N) antigens, producing a new strain every few years. Influenza A: Pandemic influenza Influenza B: Epidemics; children badly affected Influenza C: Sporadic, upper respiratory infections Tens of thousands of people die of influenza during every epidemic. The "flu shot" works great for kids but only produces a 30% or so reduction in cases when used in nursing homes (abstract 92357998, from Italy). You already know about the 1918 epidemic of "Spanish flu", which caused the greatest number of deaths of any acute infectious disease outbreak. Forty million dead is a conservative estimate (Nat. Med. 10: S-83, 2004). The mutation that triggered it: Science 293: 1842, 2001. * The dread chicken flu in Hong Kong: Lancet 351: 467 & 472, 1998. Evolution of new flu strains is blamed on agricultural practices in which chickens and pigs are raised together. * Recovering the virus and its genes from bodies frozen in the Alaskan permafrost: Proc. Nat. Acad. Sci. 96: 1651, 1999. This is from the Armed Forces Institute of Pathology team that succeeded in recovering the virus, which was also able simply to make the recovery from old glass autopsy slides. The leader of the rival group, which sought unsuccessfully to recover the virus from a Norwegian burial, wrote the science-adventure book "Hunting the 1918 Flu" (review NEJM 250: 352, 2004).
Parainfluenza viruses cause symptoms similar to influenza. Remember them as causes of laryngotracheobronchitis ("croup"). Echovirus (* "enteric, cytopathic, human orphans"), an oral-fecal route pathogen that reaches the other tissues via the bloodstream, produces sore throat and perhaps a rash ("exanthem"). It's also linked to myocarditis.
Coxsackie virus A (* named for Coxsackie, N'Yawk) produces an annoying, blistering infection of the throat, confusingly mislabelled "herpangina". It also produces the curious, usually-mild "hand, foot, and mouth" disease (strains A15 and A16 and others including enterovirus 71; blisters on hands, feet, and mouth; * Not to be confused with the dread foreign zoonosis, "hoof/foot and mouth disease"; see above. Acyclovir therapy for coxsackie A: Cutis 57: 232, 1996.
Coxsackie virus B can involve the pleura (producing pleural pain, or "pleurisy"). It is also implicated in both acute myocarditis and (as we have seen) in chronic immune-mediated myocarditis ("Barney Clark's disease").
Enterovirus 71 is one to watch. It caused a 1998 epidemic in Taiwan with a devastating rhombencephalitis (NEJM 341: 929, 936, & 984, 1999). Vaccine Lancet 381: 1037 & 2024, 2013. Respiratory syncytial virus ("RSV"; NEJM 325: 57, 1991) causes epidemics of potentially-lethal bronchiolitis and pneumonia in children (well-known, and rampant in hospitals Clin. Inf. Dis. 31: 590, 2000) and debilitated adults (stay tuned). In fatal cases, we see epithelial syncytia (i.e., fused, multinucleated cells) in the terminal bronchiolar mucosa. * Monoclonal antibody administered straight into the lungs to fight RSV: Proc. Nat. Acad. Sci. 91: 1386, 1994 (if we get a cure for the common cold it could be down these lines, but it's a long way off). * You already know that the old-time RSV vaccine produced antibodies that protected the virus from the rest of the immune system, making the real infection worse. By age 2, pretty much everybody has met RSV. Children at extreme risk may get partial protection by monthly injections of palivizumab, a monoclonal antibody.
 RSV
RSV
WebPath Photo Note that certain other viruses (measles

, mumps

, rubella

, chickenpox, etc.) enter the body by way of the lungs. They may produce lung involvement during the clinical phase, but this follows spread of the virus through the bloodstream. NOTE:
Mycoplasma pneumoniae, a little bacterium, is another very notable cause of chest colds, probably more common than these viruses. More about this later.
GI TRACT VIRUSES
Mumps A childhood illness featuring inflammation of the major salivary glands. (Not all glands may be involved; still, you can't get mumps twice.) Adults may also suffer from orchitis, oophoritis, and/or pancreatitis. High-pressure in the testis is uncomfortable and is likely to cause ischemia and permanent loss of spermatogenesis. Fortunately, it is usually unilateral.
Encephalitis and/or meningitis are usually mild; researchers notice that lab findings of viral meningitis are present in about half these kids. Most kids are immunized against mumps, but the virus is still very much with us, producing a few hundred cases per year in the US. * The "Rubini strain" of mumps virus, promoted as safer for use in vaccines, conferred no immunity, and a mumps epidemic followed in Singapore (Lancet 354: 1355, 1999).
Mumps resurgent in the USA among college students -- no one knows why, since most of those infected did have two doses of the vaccine (NEJM 358: 1580, 2008; NEJM 367: 1704, 2012).
Viral enteritis / diarrhea (NEJM 325: 252, 1991; JAMA 269: 627, 1993; poor nations Proc. Nat. Acad. Sci. 91: 91, 2390, 1994.) Rotavirus is an important cause of mild winter vomiting and diarrhea in children; most adults are immune. Vaccine JAMA 273: 1191, 1995; approved by FDA late 1998, banned after a few kids got intussusceptions from hyperplastic lymph nodes after taking the vaccine. The tort lawyers got involved and claimed causality. So the vaccine wasn't distributed anywhere else. This got reaction from the parents of the 600,000 kids who died each year of rotavirus in the poor nations (Science 287: 491, 2000; Lancet 358: 1224, 2001). In the followup, everybody realized that banning the vaccine was a terrible mistake (Science 293: 1576, 2001; JAMA 287: 1455, 2002). Thankfully, "safer vaccines" are now available, oral formulations were being used around much of the world by 2005 (Lancet 368: 323, 2006), and a pentavalent oral vaccine was licensed in the US in 2006 (NEJM 354: 11, 2006, Pediatrics 119: 11 & 171, 2007; update NEJM 360: 1063, 2009).
Norovirus ("Norwalk agent") causes outbreaks of vomiting and/or diarrhea at any time, in children or adults. Both are transmitted by the fecal-oral route, by a variety of intermediates including fomites. Damage to epithelial cells allows fluid into the gut, resulting in diarrhea. Epidemiologists look for both of these using electron microscopy. The remaining cases are probably caused by adenoviruses . Despite the frequent diagnosis of "GI virus", food poisoning is probably more common.
. Despite the frequent diagnosis of "GI virus", food poisoning is probably more common. * New epidemic gastroenteritis: Mexico virus (from England, naturally... J. Inf. Dis. 175: 951, 1997)
RASH VIRUSES
We'll cover warts, etc., under "Skin". For now, remember: Human papillomavirus type 2... the most common cause of common warts Human papillomavirus types 16 & 18 the most common cause of cancer of the cervix.
Today, clinicians base treatment decisions on the strain number. 
Measles ("Rubeola"; update on measles NEJM 366: 1755, 2012) Still a major infectious disease worldwide. Indiginous measles was eliminated from the Americas in the early 2000's. There are still outbreaks in Europe (3909 cases in 2007 -- Lancet 373: 356 & 383, 2009) -- the data reflects the poor herd immunity (immigrants, anti-immunization activism being much more influential in Europe, government programs not reaching children). During the early 2000's, measles rates in Africa dropped by about 90% thanks to immunization (Lancet 373: 984, 2009). Before the vaccine, measles was part of everyone's childhood. Many of the ultra-orthodox in Israel oppose immunization; in 2007, they had 250 cases of measles. As it affects only humans, it could be eliminated through immunization, which works for about 90% of people; the rest are protected by herd immunity. * DNA measles vaccine: Nat. Med. 6: 776, 2000.
Transmission is by droplets. The incubation period is two weeks. Measles begins as a cold and eye discomfort, followed by Koplik's spots (blister-ulcers next to Stensen's ducts), generalized lymphoid hyperplasia, and then by a typical rash.
{12292} measles
{24924} Koplik's spots
Complications include significant pneumonitis (1 out of 30 cases in the US prior to immunization), hemorrhagic rash ("black measles"), and (1/1000 cases) an severe, autoimmune post-measles encephalitis that often causes permanent brain damage. If you ever see measles tissue under a microscope, look for multinucleate epithelial giant cells (often with each nucleus bearing an intranuclear inclusion), and "Warthin-Finkeldey" multinucleated T-cell derived giant cells in lymphoid tissue (less likely to have spectacular intranuclear inclusions).
{24925} measles giant cell
The acute encephalitis is distinct from subacute sclerosing panencephalitis (SSPE), in which measles virus acts as a slow virus. More about this under CNS pathology.
Vulnerable hosts (the elderly, babies, the poorly-nourished, the immunosuppressed) are prone to measles ("giant cell") pneumonia and/or secondary bacterial infection and death. Measles kills about 800,000 people yearly, mostly in the poor nations (JAMA 287: 1172, 2002). We believe measles does not damage the fetus. In today's developed countries, immunization to measles is supposedly available to anyone who wants it. In the U.S., poor kids often are not immunized, thanks mostly to our Byzantine system of health care (Hastings Center Reports 21(4): 3, 1991). In the 1980's, many Europeans refused immunization of their children following the media campaign against whooping cough, and a measles epidemic wrecked havoc (Arch. Dis. Child. 64: 1442, 1989). Today's measles outbreaks typically occur in poor communities where the preschool children are unimmunized; the disease rips through them, they take it home to their baby brothers and sisters, lots of kids are hospitalized, and a few get brain damage or die. Outbreaks started becoming common in Britain in 2001, when the percentage of parents opting-out of immunization became sufficient to cause this to happen: Science 301: 804, 2003; Lancet 363: 569, 2004. In the US, measles is thankfully rare, associated mostly with foreign travel (foreigners bringing it to the US, or US tourists catching it overseas); the vast majority of cases are in people who are not immunized because of "religious or personal beliefs" (JAMA 299: 2621, 2008). * Think about the math. The average number of people who will catch the illness from an infected person (R0) is a function of population density, infectiousness of the disease (ultra-high for measles to the unimmunized), and percentage of unimmunized people. As soon as this exceeds 1.0, expect an outbreak. In 2000 alone, 454,000 human beings in Africa died of measles (Lancet 366: 832, 2005) and 873,000 people died worldwide of measles in 1999 (Lancet 369: 191, 2007). Every one of these deaths could have been prevented by immunization, which is inexpensive and easily supplied. And it is now happening... there were only 345,000 deaths worldwide in 2005 (Lancet 2007, above).
* The measles virus is a morbillivirus. The other, new Australian morbillivirus ("Equine morbillivirus") that kills horses (and a horse-trainer) is described in Science 268: 94, 1995 and reviewed in Lancet 349: 93, 1997. Another man died of the virus a year after assisting with the autopsy.
German measles ("Rubella", "three day measles"; Lancet 385: 2279, 2015;) This mild droplet-borne illness, with a rash and arthritis, causes fetal damage (cataracts, blindness, deafness, heart defects, skeletal deformities, high IgM in cord blood, thrombocytopenia, big spleen and liver, and so forth; "* Gregg's syndrome"). Serious rubella ought to be a thing of the past, but it's still with us, thanks to incomplete immunization. This is scandalous.For decades, many countries (even oh-so-modern Taiwan) didn't immunize: J. Micro 31: 217, 1998; MMWR Jul, 13, 2001. In Morocco, around one newborn in 10,000 is crippled (Lancet 365: 29, 2005; something about how countries decide not to immunize.) The Fort Bragg outbreak in which unimmunized German soldiers got sick: Mil. Med. 164: 616, 1999. The impact of anti-immunization activism, especially the pop claim that MMR causes autism due to its containing thimerosal (ethylmercury), has been tremendous: Br. J. Gen. Pract. 50: 969, 2000; thankfully, only a handful of kids die in the US each year because of this business. And it's clearly not true -- there's no dose-response association, and no relationship between reported autism and whether the batch of vaccine actually contained thimerosal (JAMA 290: 1763, 2003). Congenital rubella continues to be a major cause of devastating birth defects in the developing nations. India, Pakistan, Indonesia and most of Africa have no plans to immunize (as of 2015.)
{53732} congenital rubella after-effects
Smallpox ("Variola") This ancient disease is the first one to be controlled, then conquered, by science. It is transmitted by droplet infection, multiplies in the throat, enters the bloodstream, and multiplies further in the lymphoid tissue. Two weeks after infection, the rash appear synchronously over the body. The spots become vesicles (i.e., sites of necrosis of the lower skin layers) and then pustules (i.e., vesicles that have been invaded by neutrophils). Systemic involvement caused death; survivors were scarred. Viral cytoplasmic incisions are called * Guarnieri bodies.
Medical historians: Dr. Ed Jenner noted that milkmaids did not get smallpox (and were therefore famous for their beauty) because cowpox (a febrile illness with a rash on the hands, caught from milking cows) conferred immunity. He began inoculating people artificially with this virus, and the rest is history; * the population explosion of the 1800's must have been partly due to this discovery. * "Vaccine" < vache, French for "cow".
No one knows the real origin of today's smallpox vaccine virus ("vaccinia"). It is so immunogenic that vaccination during actual smallpox can be life-saving. In rare cases, inoculation with this virus produces a spreading, gangrenous infection; patients have underlying immunodeficiency or bad eczema ("atopic dermatitis"). Watch for new vaccines based on recombinant vaccinia, which can be made to express most antigens. They should be one-dose vaccines, perhaps even oral (Proc. Nat. Acad. Sci. 91: 11187, 1994).
* People are still making massive political capital off the 1763 Fort Pitt episode, in which British Captain Simeon Ecuyer supposedly sent blankets bearing smallpox to the Indians under Chief Pontiac in an unsuccessful attempt to start an epidemic. Be this as it may, other European-Americans went to great lengths to prevent the transmission of smallpox to the Indians (Bull. Hist. Med. 78: 575, 2004), discovering in the process that quarantining doesn't work and immunization does. * The "big pox" (great pox, etc.) was syphilis . Shakespeare: "A pox on you!", etc. * Smallpox inspired English laureate John Dryden's best bad poem, with such verses as: "Each little pimple had a tear in it/ To lament the fault its rising did commit."
. Shakespeare: "A pox on you!", etc. * Smallpox inspired English laureate John Dryden's best bad poem, with such verses as: "Each little pimple had a tear in it/ To lament the fault its rising did commit."
 * Monkeypox is a rare poxvirus disease similar to smallpox, but not nearly so severe. The pet prairie dog business: MMWR 52: 561, 2003; NEJM 350: 342, 2004; it was hyped (wrongly, of course) as a deadly, untreatable scourge. Orf is contracted from sheep, and milker's nodules represent yet another poxvirus infection. Tanapox is a mild local illness that is common in Africa: NEJM 350: 351, 2004. We'll study the other semi-important pox virus disease (molluscum contagiosum) when we talk about skin.
* Monkeypox is a rare poxvirus disease similar to smallpox, but not nearly so severe. The pet prairie dog business: MMWR 52: 561, 2003; NEJM 350: 342, 2004; it was hyped (wrongly, of course) as a deadly, untreatable scourge. Orf is contracted from sheep, and milker's nodules represent yet another poxvirus infection. Tanapox is a mild local illness that is common in Africa: NEJM 350: 351, 2004. We'll study the other semi-important pox virus disease (molluscum contagiosum) when we talk about skin.
 Erythema infectiosum ("fifth disease", "parvo", "slapped cheek disease" with a reticulated red rash on the trunk and extremities; parvovirus B19) and roseola infantum ("exanthem subitem"; fever and ephemeral pink rash at the end, sparing the face and feet; herpesvirus 6 and the little-known herpes 7, maybe others; see below); are trivial childhood diseases.
Erythema infectiosum ("fifth disease", "parvo", "slapped cheek disease" with a reticulated red rash on the trunk and extremities; parvovirus B19) and roseola infantum ("exanthem subitem"; fever and ephemeral pink rash at the end, sparing the face and feet; herpesvirus 6 and the little-known herpes 7, maybe others; see below); are trivial childhood diseases.
*
{08157} fifth disease (parvovirus 19; "slapped cheek disease")
*
{08158} fifth disease
These viruses hang around for life and can cause troubles later. Parvovirus B19 ("erythrovirus" if you prefer) is infamous as the cause of marrow wipeout in the unborn child (nonimmune hydrops fetalis; look for red intranuclear inclusions), and aplastic crises in hereditary hemolytic diseases (sickle cell, spherocytosis). Herpes 6 is newly-recognized as an opportunist in AIDS and others.
 Herpes 6
Herpes 6
Peripheral smear
Wikimedia Commons Keep an eye on "parvo". It's one of the "usual suspects" in a host of illnesses, including a rheumatoid arthritis variant (PNAS 95: 8227, 1998) and polyarteritis nodosa. Infections in adults can be vicious (weeks or months with arthritis) and hard-to-cure; consider giving a shot of gamma globulin if you're in doubt.
 Parvo
Parvo
WebPath Photo * Parvovirus B19 binds to your P blood group; if you're pp, you can't get it (NEJM
330: 1192, 1994).
HERPES VIRUSES
These are at least eight (at last count) important DNA viruses. Each usually produces a mild (often unnoticed) illness upon entering the body. The virus then lies latent within the host genome, awaiting reactivation, for the rest of the person's life. Millions of people in the U.S. harbor each one; HSV-2 is much less common than 1,3,4,5, or 6. And from time to time, herpes infections kill people.  Herpes simplex 1
Herpes simplex 1 This is usually contracted by getting kissed, typically as a baby. (Some people get a gingivostomatitis following infection.) A majority of adults have the virus, though most never become sick or suffer only fever blisters.
{21245} primary herpes infection (trust me)
{21247} primary herpes infection (trust me)
 Herpes
Herpes
Patient photos
Health Awareness Connection
The virus climbs sensory nerves and hides in nervous tissue (especially trigeminal ganglion). When it emerges from hiding, it causes disease. Recurrences are often, but not always, triggered by hyperthermia or sun exposure. * Interleukin 6 as possible reactivator: J. Inf. Dis. 175: 821, 1997. In normal folks, recurrences usually produce discomfort and small vesicles in the epithelium innervated by these nerves. This is typically a necrotic area on the lower lip, also called a "cold sore", "fever blister", "sun blister" (use a sun-screen: Lancet 338: 1419, 1991), "stress blister". NOTE: These lesions are totally unrelated to aphthae, the familiar, painful, transient white ulcers in the mouth itself.
{14122} herpes on the lip
{14124} herpes on the eyelids
{14128} herpes on the thumb
{12009} herpes on the lip
{12010} herpes on the wrist
More troubling, the virus can produce generalized, severe vesicular eruptions of the skin ("varicelliform herpes" and "eczema herpeticum"; this is especially likely in people who already have atopic dermatitis, or "eczema"). There are also herpes ulcers of the cornea (ouch!), or even necrosis of the temporal lobes of the brain ("herpes encephalitis", a mysterious process).
{15473} herpes encephalitis, residual
In the immunocompromised, look for really bad fever blisters, herpes eruptions of the esophagus, or herpes pneumonitis. The former is painful, the latter is deadly. In the very immunocompromised or in babies, many of the viscera may undergo necrosis at once. (Future pediatric pathologists: Look at the brain, lungs, adrenals and liver.)
{20038} herpes of a baby's liver, gross
Pathologists recognize typical herpes cells in sections or touch preparations ("Tzanck preparations"). The nucleus loses its texture and becomes pale and swollen. In its center, there is typically a large eosinophilic inclusion, surrounded by a clear zone (* "Cowdry A inclusion"). Often giant cell formation (cell fusion) occurs, revealing large cells packed with herpes nuclei.
{13338} herpes of skin, histology (swollen pale nuclei, no inclusions today)
{13341} herpes of skin, histology (swollen pale nuclei, no inclusions today)
{13342} herpes of skin, high magnification (swollen pale nuclei, no inclusions today)
{14136} positive Tzanck prep
Whether mild or severe, pathologists expect to see necrotic areas with herpes-type cells at their peripheries.
The virus is a clear risk for cancer of the mouth and throat, and seems to act synergistically with alcohol and tobacco. * There is currently much interest in using herpes simplex 1 to infect cancer cells in organs with non-dividing cell populations (liver, brain, others). The virus produces an enzyme that makes gancyclovir kill a dividing cell. Stay tuned.
Herpes simplex 2 ("herpes genitalis") This virus is usually contracted through sexual contact, and produces painful, recurrent blisters on the genitals. The pathology is identical to HSV-I. This was a social handicap for the "free-love" generation. In the immunocompromised, HSV-2 is not a pretty sight.
{14133} herpes on a man
{14134} herpes on a woman
{24936} herpes on a pap smear, good inclusions
{05272} herpes in a man with AIDS
If active herpes simplex is present in the birth canal, the newborn will probably contract the infection during vaginal delivery. This is often a fulminant, deadly infection. When in doubt, Caesarean section is indicated. * Herpes very seldom crosses the placenta (J. Med. Virol. 51: 210, 1997).
{15609} baby died of herpes 2
Herpes necrotizing encephalitis is almost always due to type 1 herpes, but many patients experience a viral meningitis ("stiff neck") during the first episode of herpes 2. "Serologic testing" for genital herpes is still notoriously inaccurate: Am. J. Clin. Path. 120: 839, 2003.* Herpes 2 vaccine: J. Inf. Dis. 175: 16, 1997.
Human herpes six (Mayo Clin. Proc. 74: 163, 1999) Keep your eye on this one. It can cause disease by itself (Lancet 338: 147, 1991), and is blamed for accelerating the course of HIV infection. The virus invades B-lymphocytes and stays latent in the body following infection. Primary herpes six in children: NEJM 326: 1445, 1992 (exanthem subitem, also known as roseola). Around 90% of us harbor the little creature. Update NEJM 352: 768, 2005.
Herpes 8: The Kaposi's sarcoma virus, KSHV/herpes 8. Fulfilling Koch's postulates: Nature 373: 667, 1995; Am. J. Path. 150: 147, 1997 (the virus in the semen of most men with Kaposi's); J. Inf. Dis. 175: 947, 1997.Unlike most other viruses, KSHV has hijacked a handful of activated human oncogenes, including a cyclin that inhibits Rb-protein and two apoptosis inhibitors. Review NEJM 342(14), 2000.
Future pathologists! Recognize Kaposi's by...
- Spindle cells with slits instead of vessels;
- Extravasated red cells
- Usually but not always, some hyperchromatic nuclei
- "Hyaline globules" (i.e., phagocytized red cells) inside the spindle cells
- Early, just sprouts of vessels around a larger vessel
- Late, likely to be hemosiderin
- Immunostain foor KSHV (Am. J. Clin. Path. 121: 330 & 335, 2004)
Chickenpox ("varicella") / herpes zoster ("Herpes 3") On first meeting this virus, a person (usually a child) develops "chickenpox", a highly contagious disease spread by droplets. The rash consists of vesicles that arise in successive crops over the body. (* Future clinicians: Starts on the trunk and spreads outward.) Only about 15 kids die in the US each year from chickenpox. After recovery, the virus hides out in the dorsal root and/or sensory trigeminal ganglia. Herpes zoster ("zoster", "shingles") is recurrence of the chickenpox rash, typically along the distribution of a sensory nerve root.
{14146} zoster
{14149} zoster, trig-1
{14152} zoster, trig-2
{14154} zoster, trig-3
{14155} zoster, face ("facial nerve")
{12116} varicella
{14137} varicella
The lesion is always uncomfortable, and eye involvement (V1) is very serious. It is preceded by paresthesias, and pain after herpes zoster is notorious ("post-herpetic neuralgia"). The blisters can infect a child with chickenpox. Its appearance may represent immunosuppression (around 30% of Hodgkin's disease patients are troubled by it), or just bad luck.
The immunosuppressed can get pneumonia, or total body recurrence. Older patients, or unlucky children, can get an encephalitis, which is probably immune-mediated. Regardless of site or severity, the histopathology of chickenpox / zoster is almost identical to herpes simplex. A varicella virus vaccine is available, and implementing its use would save money (not to mention lives and suffering: JAMA 271: 35, 1994). It is now in general use (NEJM 344: 955, 2001). Even us older folks who had chickenpox as kids are now taking it so that we never get shingles (immunity wanes with time, and is restored by a shingles attack, which is supposed to be vaccine-preventable: NEJM 356: 1338, 2007). In 1996, after a year in which there was no successful U.S. lawsuit against a physician for following immunization protocols, a campaign began to immunize teens who had not yet gotten chickenpox (JAMA 276: 766, 1996).
We now know that chickenpox during the first 20 weeks of pregnancy can damage the unborn child (NEJM 330: 901, 1994). Immunizers take note. * "Chickenpox" in the immunosuppressed caused by herpes simplex is "Kaposi's varicelliform eruption".
 Cytomegalic inclusion disease ("CMV"; "cytomegalovirus", "herpes 5")
Cytomegalic inclusion disease ("CMV"; "cytomegalovirus", "herpes 5") A very common viral infection. It can be contracted in utero, during birth, or from Mom's saliva or milk during infancy. If avoided in childhood, it is easily transmitted during sex (and probably from kissing or maybe even being coughed upon), or from blood transfusions (after he was shot, Pope John Paul II got sick from transfusion-acquired CMV), or bone marrow transplantation. Usually, the person meeting the virus sheds it only for a few days. Teens and adults may note an infectious mononucleosis-like infection that lasts up to a few weeks (* bad? get out the gancyclovir: J. Ok. State Med. A. 90: 367, 1997). However, if acquired during pregnancy, the virus is shed through pregnancy and lactation. With all these possibilities, around 80% of people eventually turn positive for this ubiquitous virus. It stays latent, until you are immunosuppressed.
The most disturbing feature of CMV is its ability to damage the unborn child. While most fetuses meeting CMV show no signs of damage, a child with congenital CMV syndrome is small for gestational age, jaundiced, afflicted with hemolytic anemia, afflicted with thrombocytopenia and purpura, blind, deaf, retarded, and/or epileptic. Widespread brain necrosis is common, typically occurring around the ventricles and calcifying.
{15805} CMV "blueberry muffin rash"
The hallmark of any CMV infection is very large cells (hence the name), with large nuclei with large intranuclear inclusions. The inclusion is huge and is surrounded by a clear halo. There are also small basophilic inclusions in the cytoplasm. Future pathologists: Sometimes "CMV-cells" are all over; sometimes really good cells are hard to find. The best single place to look is salivary glands. Next is kidney. You may get lucky and see them in urine. Even more sensitive is the gene probe for the virus. * "Stealth viruses", much-discussed in "alternative medicine" and "anti-vaccine" circles, supposedly carry genes between eukaryotic species. One independent researcher finds them everywhere; no one else writes about them at all. Draw your own conclusions.
{16626} CMV in the kidney
{18807} CMV in the kidney
{20035} CMV in salivary gland
{20036} CMV in salivary gland
{22232} CMV in the retina (you need only recognize that there is lots wrong)
{01741} CMV schematic diagram
CMV in the immunosuppressed patient involves the lungs (deadly pneumonia) or GI tract (necrosis, even perforation). AIDS patients are prone to develop CMV chorioretinitis, which results in blindness.
Infectious mononucleosis / Epstein-Barr virus ("human herpesvirus 4") Epstein-Barr virus ("EBV") is the most notable cause of infectious mononucleosis, and some people define "infectious mononucleosis" to be the EBV-related disease. Most people meet the Epstein-Barr virus in childhood and never become symptomatic. Teens and adults are prone to get the familiar "infectious mono" syndrome. The virus is transmitted by saliva (i.e., kissing). The incubation period for "infectious mono" is about 6 weeks.
The virus has a special trophism for B-cells, in which it multiplies. The EBV receptor is the C3d receptor (* CD21). Infected B-cells will keep virus into their genome, and are immortalized (* gene EBNA2 from EBV turns on several B-cell genes and seems to be responsible for immortalization: Proc. Nat. Acad. Sci. 90: 5893, 1993; Science 265: 92, 1994; Science 268: 560, 1995; more Proc. Nat. Acad. Sci. 94: 1761, 1997); there's ongoing work to find exactly how it immortalizes. Eventually, B-cells that bear viral antigens are eliminated by cell-mediated and humoral immunity. * EBV packs slightly-altered versions of our own bcl-2 and interleukin-10 anti-apoptosis genes, just to prevent killing of its host B-cells by T-cells (Proc. Nat. Acad. Sci. 94: 5860, 1997). * Epstein-Barr type 2 is most common among gay men. No one knows why, or exactly how it is transmitted (J. Inf. Dis. 18: 2045, 2000).
Proliferation of B-cells bearing EBV antigens on their surfaces is upsetting to T-suppressor cells and T-killer cells. These T-cells proliferate throughout the body, and are seen in the bloodstream. (Before we knew they were T-cells, we assumed they were "monocytes", hence "mononucleosis"; we'll report these as "atypical lymphocytes" or "virocytes" today.) Recognize these by their large size, abundant vacuolated cytoplasm, and large, reticulated nuclei. (* Other types of "atypical lymphocytes" exist; we'll teach you about these in "Clinical Pathology".)
The patient with "infectious mononucleosis" has fever, malaise, fatigue (interleukin effect), and generalized lymphadenopathy (check behind the ears). Usually, the throat is sore. If you biopsy a lymph node, you'll see hypercellular paracortical (T-cell) areas, and large germinal follicles (B-cell activation). The spleen is packed with activated cells and may rupture (they infiltrate the capsule; be gentle palpating these spleens.)
{13706} circulating upset T-cell in infectious mononucleosis
{21243} posterior auricular lymph nodes
{23434} immunoblasts in infectious mono node (don't worry about how to tell this from CMV)
{46188} immunoblasts in infectious mono node
There may be mild liver damage (elevated transaminases, jaundice). In rare fatal cases, the CNS is heavily infiltrated by lymphocytes. "Petechiae on the palate", once considered diagnostic, wasn't (chuckle, Oral Surg. 52: 417, 1981).
Several things make infectious mononucleosis a mysterious illness:
- Around half of patients get cold agglutinins and autoimmune hemolytic anemia
- There is mild thrombocytopenia
- There may be a rash, especially if someone gives the patient "ampicillin for that strep throat."
- If you have X-linked recessive lymphoproliferative immunodeficiency, you'll probably die of infectious mono.
- * In fatal infectious mono, you'll find extensive phagocytosis of red cells by macrophages ("hemophagocytic syndrome", review with animal model Am. J. Path. 158: 1533, 2001)
Here's more than you probably want to know about mono testing: Strictly speaking, heterophile antibodies, which occur in many inflammatory diseases, are IgM antibodies that agglutinate sheep red cells. Forsmann antibodies, which occur in many inflammatory diseases, are heterophile antibodies that are absorbed by guinea pig kidney but not by beef RBC's. Mono test ("Mono-spot") antibodies are induced by EB-virus infectious mono. These are heterophile antibodies that are absorbed by beef RBC's, but not by guinea pig kidney (* "Paul-Bunnell reaction"). The "Mono-spot" is cheap, reasonably sensitive and very specific, but often remains negative for many weeks, and often never turns positive in children. The antibody goes away in about 6 months. More expensive, more definitive tests are available. Serum IgG anti-EBV capsid indicates past or present EBV infection. High titers suggest current infection. This is the test to order if the "Mono-spot" is still negative but you still suspect EBV mono. Serum IgM anti-EBV capsid indicates current EBV infection. It is sensitive and specific, and very useful in children. EBV "early antigens" indicate early or chronic EBV disease. Ask your infectious disease expert whether these tests are useful.
The large majority of patients recover, and the virus remains latent for the rest of the patient's life. Chronic infectious mononucleosis exists; its existence is documented by persistent acute-phase antibodies. The link between EBV and Burkitt's lymphoma is well-known; it promotes (as a mitogen), and causes the 8:14 translocation. Also well-established are the links to lymphocyte-rich squamous cell carcinoma of the throat ("lymphoepithelioma", a Chinese disease), and Eskimo salivary gland cancer (Cancer 57: 2097, 1986), as well as lymphomas of the brain (always) and elsewhere (usually) in AIDS and other immunosuppressed people. EBV causes leiomyosarcoma in the immunosuppressed: NEJM 332: 12 & 19, 1995. Mechanisms of transformation: NEJM 333: 724, 1995. * There is presently some interesting circumstantial evidence pointing to Epstein-Barr virus, acquired after infancy, is the cause of multiple sclerosis. Apparently all MS patients have the virus on board, and a viral protein closely mimics myelin basic protein. Stay tuned. * The link to Hodgkin's disease and some other cancers remains dubious. In evaluating a claim that "Epstein-Barr virus is often found in the cells of thus-and-such a tumor", remember that it's commonplace to find it in various normal tissues of people without any disease (Am. J. Clin. Path. 100: 502, 1993).
 * Herpesvirus simiae (cercopithecine herpes 1, simian herpes B virus) is a dread infection caught from being bitten by a monkey. It causes a severe encephalomyelitis. What to do if you are exposed: Clin. Inf. Dis. 35: 1191, 2002.
* Herpesvirus simiae (cercopithecine herpes 1, simian herpes B virus) is a dread infection caught from being bitten by a monkey. It causes a severe encephalomyelitis. What to do if you are exposed: Clin. Inf. Dis. 35: 1191, 2002.
ARBOVIRUSES (
arthropod-
borne)
Yellow fever monkey reservoir. This is the prototype of the "viral hemorrhagic fevers", a family of disturbing diseases, mostly (but not all) transmitted by biting insects. Yellow fever primarily affects monkeys, with humans becoming infected when bitten by an Aedes mosquito. The incubation period is a few days. The patient develops a flu-like syndrome, during which liver failure (jaundice, bleeding tendency, hypotension) becomes apparent. Future liver pathologists: As you would expect, there is hepatic steatosis and Councilman bodies (i.e., apoptotic hepatocytes). Mid-zonal necrosis of hepatocytes is the rule, but the liver architecture is not damaged. Unlike other forms of hepatitis, there is essentially no inflammation.
Most patients recover uneventfully, without scarring of the liver. In severe cases, death results from brain or heart damage.
Dengue (say it DENG-gee or DENG-gay, not DENG-yoo; travellers Lancet 370: 1644, 2007; JAMA 299: 214, 2008; Lancet 371: 1216, 2008; NEJM 366: 1432, 2012) The terrible outbreak in Brazil in 2008 was due to mosquito-breeding debris-puddles in the urban slums: Lancet 372: 205, 2008. A major world disease caused by any of four flaviviruses (dengue-1, dengue-2, dengue-3, dengue-4), which are trophic for macrophage-monocytes. Infection by the virus produces a self-limited, Aedes mosquito-borne, flu-like illness with a rash. The worst feature is severe arthralgias and myalgias ("breakbone fever"), which will tip the physician off that this is dengue. I predicted in 2002 that it would reach the continental US due to global warming, and this has happened (Pub. Health Rep. 127: 259, 2012). * Neutropenia and thrombocytopenia is probably due to infection of the marrow stromal cells by the virus: Am. J. Trop. Med. 54: 503, 1996)
The most severe forms are "hemorrhagic dengue" and "dengue shock syndrome" (diffuse vascular leakage). Both are life-threatening. They are probably due, at least in part, to widespread T-cell activation (Nat. Med. 9: 820, 2003). And there may be CNS damage in dengue as well, with the virus attacking the neurons (Lancet 355: 1053, 2000). It's now clear that "hemorrhagic dengue" and "dengue shock syndrome" result from infection by a second dengue virus in someone who has recovered from a previous infection and mounts too brisk an immune response (J. Inf. Dis. 185: 1697, 2002); this can happen during a single epidemic since the virus mutates rapidly (Lancet 355: 1902, 2000). There are maybe half a million cases of these severe illnesses worldwide each year (NEJM 313: 484, 2010). * Why this probably happens, at the immune-system level: Nat. Med. 9: 999, 2003. Preformed antibody is abundant but non-neutralizing; sensitized T-helper cells are tremendously overactivated.
Dengue is the world's most common arthropod-borne viral infection, with up to many millions of cases each year and thousands of deaths, resurgent with the resurgence of Ae. Aegypti in the Americas (Am. J. Trop. Med. Hyg. 87: 584, 2012). It is inviting to think that dengue, which mutates very rapidly and can probably change its tropism, is the origin of the other pathogenic filiviruses (yellow fever, hepatitis C, hepatitis G family). A live attenuated tetravalent dengue vaccine exists and may become widely available soon -- one concern is a striking elevation of liver enzymes on challenge with dengue virus 3 (J. Inf. Dis. 207: 700, 2013). Vaccine update NEJM 372: 113 & 172, 2015.
West Nile Virus (NEJM 310: 308, 2013), carried by mosquitoes, reached the US in the late 20th century. Usually it produces headache, severe muscle pain, and a rash, but without encephalitis or meningitis. In 1999, a cluster of patients in New York City suffered confusion and profound weakness after becoming infected (Clin. Inf. Dis. 30: 413, 2000). The autopsy series: Emerg. Infect. Dis. 6(4): 370, 2000 (brain necrosis, with microglia and neutrophils). Chikungunya, the mosquito-borne epidemic disease that spread very rapidly especially around the Indian Ocean in 2005-2006: NEJM 356: 769, 2007; Lancet 379: 662, 2012; update NEJM 372: 1231, 2015. Regional hemorrhagic fevers (Argentine, Bolivian, Crimea, Korean, Lassa, Omsk, others)
The "Red Death" had long devastated the country. No pestilence had ever been so fatal, or so hideous. Blood was its Avatar and its seal--the redness and the horror of blood. There were sharp pains, and sudden dizziness, and then profuse bleeding at the pores, with dissolution. The scarlet stains upon the body and especially upon the face of the victim, were the pest ban which shut him out from the aid and from the sympathy of his fellow-men. And the whole seizure, progress and termination of the disease, were the incidents of half an hour. -- Edgar Allan Poe, "The Masque of the Red Death"
These illnesses, mostly tick-borne zoonoses, produce flu-like syndromes with bleeding tendencies. They range from mild to severe. The most virulent in the group is Lassa fever. Its reservoir is an East African mouse that sheds the virus copiously. It is usually contracted from the animal's droppings, but is contagious from person to person if common-sense precautions are neglected (Br. Med. J. 297: 584, 1988). Lab diagnosis J. Clin. Micro. 38: 2670, 2000. Why most of these fevers cause hemorrhage has long been a mystery. Coagulation factors are unaffected, and platelet counts are often normal or only mildly reduced. Probably most of them do what Ebola does (see below), destroying endothelium.
does (see below), destroying endothelium.
Colorado tick fever ("coltivirus") resembles Rocky Mountain Spotted Fever , epidemiologically and clinically. Marburg virus, a filovirus, has caused deadly epidemics of hemorrhagic fever in people exposed to monkey tissues (the 1967 German outbreak) and perhaps other sources.
, epidemiologically and clinically. Marburg virus, a filovirus, has caused deadly epidemics of hemorrhagic fever in people exposed to monkey tissues (the 1967 German outbreak) and perhaps other sources.How outbreaks begin remains mysterious (J. Infect. Dis. 179 S-1: S127, 1999). Once they begin, hospital workers are at tremendous risk.* The story of the Kitum cave on Mt. Elgon is famous -- two patients with no other source of infection, seven years apart, had just visited it. However, the cave is much-visited, is a famous ceremonial site for the indigenous Masai people, and Marburg virus outbreaks are rare. The Angola outbreak, with over 200 cases and almost as many deaths: NEJM 352: 2155, 2005. It causes bleeding by reproducing in, and popping, endothelial cells (J. Cli. Inv. 91: 1301, 1993).
Ebola virus, another filovirus from Africa, causes a dreaded hemorrhagic fever. To date, we can offer only supportive treatment. How outbreaks begin reflects its nature; it's a zoonosis -- primarily chimps and gorillas (Science 317: 1484, 2007) -- which crosses to humans who handle animal carcasses (Science 303: 387, 2004). The Filipino virus got into the U.S. in 1990 among some research monkeys, but didn't become established (Lancet 335: 502, 1994) -- thankfully this is not virulent for people. The worst virulence factor is a glycoprotein which destroys endothelium (Nat. Med. 6: 886, 2000) and other cells. Death may be due to massive hemorrhage, massive immune system overactivation, and/or disseminated intravascular coagulation.Ebola is transmitted by direct contact with patients or their body fluids or in dirty needles (J. Inf. Dis. 179 S-1: S-87, 1999). Hospital workers have shown tremendous heroism in caring for these patients, with several dozen lives lost during the 1990s. The 2014 outbreak in West Africa went unrecognized for three months (NEJM April 16, 2014). Although the virus is highly lethal, many people who meet the same strains that kill their neighbors get no symptoms and recover completely (Lancet 355: 2210, 2000). Naturally-occurring antibodies in survivor convalescent serum failed to prevent the illness in others. Vaccine for primates: Nature 408: 605, 2000. Regrettably, the classic ebola vaccines don't provide immunity for several months. A "fast" vaccine gave immunity in four weeks and may be the way to contain epidemics: Nature 424: 681, 2003. I shared this information with the medical students at the time of publication and expressed the hope that it would be prepared and stored for when (not "if") it would be needed.New work with the filoviruses has showcased the complexity of the infectious process. All are similar. See Lancet Inf. Dis. 4: 487, 2004; NEJM 352: 2645, 2005
- The viruses first enter, and are carried around the body by, dendritic macrophages. Early antibodies assist entry into macrophages and endothelium.
- The virsues cause monocytes to express tissue factor on the surfaces, causing disseminated intravascular coagulation.
- The viruses destroy infected cells in large numbers, including endothelium, liver, and adrenals.
- Lymphocytes are not infected, but undergo mass apoptosis.
In 2005, your lecturer predicted the present (2014) outbreak of Ebola in the poorest areas of West Africa and expressed the hope that a vaccine would be readily available when it erupted. The fact that there were about a dozen likely candidates (before-the-crisis update Lancet 378: 389, 2011), including the chimp adenovirus vaccine that had ALREADY passed a phase I trial (Virology 383: 348, 2009; I am not making this up), and that none was mass-produced in preparation for an epidemic that anyone who understands disease could have foreseen, will be a topic of discussion for historians. It was even proposed to release the virus into the wild to protect Africa's chimps (Proc. Nat. Acad. Sci. 111: 8873, 2014 -- work done before anyone knew of the human outbreak). In August 2014, in the wake of a terrible crisis, the WHO published a statement that it would be ethical to offer unproven remedies that were likely to work, provided it was done scientifically and that there be "ongoing discussion" of "fairness" and other issues (i.e., who gets what). See also the prophetic "Wake me up when there's a crisis": Am. J. Pub. Health 101: 2080, 2011. An ebola vaccine based on vesicular stomatitis: JAMA 313: 1249, 2015. The reality was that no one was interested in rushing an ebola vaccine to the area when the outbreak began because it would not be 100% effective, and regardless there would be a public perception that wicked outsiders were experimenting on the poorest of the poor (Lancet tells it as it is -- 385: 2350, 2015).
Reston virus is an Ebola-like filovirus that is catching by air, but much less virulent for humans. This one entered the US with some monkeys from the Philippines (J. Inf. Dis. 179(S1): S-108, 1999). * Rift Valley Hemorrhagic Fever was "discovered" during the investigation of Marburg disease. It caused an epidemic in Saudi Arabia in 2000 with a high mortality rate (Clin. Inf. Dis. 36: 245, 2003); it tended to cause meningoencephalitis and/or liver necrosis. * Crimean-Congo Hemorrhagic Fever is another deadly illness that is widely distributed in East Africa and central Asia. Ribavirin seems to improve survival somewhat (Clin. Inf. Dis. 36: 1613, 2003). Hantaviruses, the cause of Korean hemorrhagic fever and the agent now established as the cause of the outbreak of fatal disease in the U.S. southwest in 1993 (inhaled mouse droppings), were once popular candidates for biologic warfare agents (Science 260: 1579, 1993). Hantavirus review Arch. Path. Lab. Med. 127: 30, 2003.
"CHRONIC FATIGUE SYNDROME" ("myalgic encephalomyelitis", philosophical review Ann. Int. Med.
134: 838, 2001; practical approach Am. Fam. Phys.
65: 1083, 2002)
Any viral infection may be followed for up to several weeks by mild malaise and lack of energy. A current medical mystery focuses on chronic fatigue syndrome ("rag doll syndrome", "Yuppie flu", "immune dysfunction", etc., etc.) This is presently defined as 6 or more months of disabling fatigue requiring >50% reduction in daily activities. There must also be some hard findings (lymph nodes, sore throat, elevated interleukin-2 levels, etc. Patients will self-diagnose this disease. During the 1990's, the more we looked at these patients, the more way-out-of-line immune parameters you find (J. Clin. Microb. 28: 1403, 1990). The CDC case definition requires a duration of over 6 months, a full workup to rule out everything else, and 8 of 10 common features including sore throat, muscle pain and weakness, fever, and sleep disturbance (Arch. Int. Med. 152: 1569, 1992; Ann. Int. Med. 117: 325, 1992.) This is for research purposes; probably not all CFS patients meet these criteria, but they do sort out the people with fibromyalgia, postconcussion syndrome, functional headache, Briquet's somatization disorder, Gulf War syndrome (if this is a specific entity), parvo B19 , "multiple chemical sensitivities" (if there is any such thing), etc. One measurable marker is probably increased orthostatic blood pressure drop (Am. J. Med. Sci. 320: 1, 2000, others). Not surprisingly, many of these patients are depressed (psychotherapy doesn't help: Am J. Med. 94: 197, 1993, suicides are common). We used to assume that this was the etiology (much as old-time physicians claimed that coughing caused tuberculosis) rather than the result of being disabled. One of the new antidepressants may help anyway. The epidemiology suggests a viral etiology (Lake Tahoe 1984, etc.), and this is strongly supported by finding of widespread immune activation in these people (Lancet 338: 707, 1991), but so far, no known agent has been implicated in the majority of cases (Science 249: 1249, 1991; herpes 6 may be one player Ann. Int. Med. 116: 103, 1992). Epidemiology: Pediatrics 89: 802, 1992; Arch. Int. Med. 152: 1611, 1992. There are a host of contradictory reports of various disturbances in the responsiveness of the CRF-ACTH-cortisol axis (J. Clin. Endo. Metab. 86: 3545, 2001) and of the disease improving on low-dose cortisol administration (Lancet 353: 455, 1999). By contrast, if a physician gets very interested in the possibility of your having "postviral fatigue syndrome", you are far more likely to "get it" (Lancet 344: 864, 1994). The good news is that the disease often remits over a few years, though in the most severe cases this is less likely (Arch. Phys. Med. Rehab. 80: 1090,1999). Graded exercise seems to help (Br. Med. J. 322: 387, 2001). Since the disease effects are quantified by subjective reports and behavior, it is hard to know what really causes "cognitive behavior therapy" to work when support groups do not: Lancet 357: 841, 2001; also JAMA 286: 1360, 2001 (CFS is hard to study). Today, it's acknowledged that this is real but poorly-understood. A combination of individual therapy, cognitive-behavioral therapy, graded exercise, and work on the internet seems to get teens back on their feet (Lancet 379: 1412, 2012). Most interesting to me as a pathologist is a study finding entervirus protein in the stomachs of most chronic fatigue patients, very few controls (J. Clin. Path. 61: 43, 2008). * XMRV (xenotropic murine leukemia virus), claimed to be the cause of chronic fatigue / fibromyalgia (Science 326: 585, 2009), isn't found by the Dutch in an established cohort: BMJ 340: c1018, 2010.
, "multiple chemical sensitivities" (if there is any such thing), etc. One measurable marker is probably increased orthostatic blood pressure drop (Am. J. Med. Sci. 320: 1, 2000, others). Not surprisingly, many of these patients are depressed (psychotherapy doesn't help: Am J. Med. 94: 197, 1993, suicides are common). We used to assume that this was the etiology (much as old-time physicians claimed that coughing caused tuberculosis) rather than the result of being disabled. One of the new antidepressants may help anyway. The epidemiology suggests a viral etiology (Lake Tahoe 1984, etc.), and this is strongly supported by finding of widespread immune activation in these people (Lancet 338: 707, 1991), but so far, no known agent has been implicated in the majority of cases (Science 249: 1249, 1991; herpes 6 may be one player Ann. Int. Med. 116: 103, 1992). Epidemiology: Pediatrics 89: 802, 1992; Arch. Int. Med. 152: 1611, 1992. There are a host of contradictory reports of various disturbances in the responsiveness of the CRF-ACTH-cortisol axis (J. Clin. Endo. Metab. 86: 3545, 2001) and of the disease improving on low-dose cortisol administration (Lancet 353: 455, 1999). By contrast, if a physician gets very interested in the possibility of your having "postviral fatigue syndrome", you are far more likely to "get it" (Lancet 344: 864, 1994). The good news is that the disease often remits over a few years, though in the most severe cases this is less likely (Arch. Phys. Med. Rehab. 80: 1090,1999). Graded exercise seems to help (Br. Med. J. 322: 387, 2001). Since the disease effects are quantified by subjective reports and behavior, it is hard to know what really causes "cognitive behavior therapy" to work when support groups do not: Lancet 357: 841, 2001; also JAMA 286: 1360, 2001 (CFS is hard to study). Today, it's acknowledged that this is real but poorly-understood. A combination of individual therapy, cognitive-behavioral therapy, graded exercise, and work on the internet seems to get teens back on their feet (Lancet 379: 1412, 2012). Most interesting to me as a pathologist is a study finding entervirus protein in the stomachs of most chronic fatigue patients, very few controls (J. Clin. Path. 61: 43, 2008). * XMRV (xenotropic murine leukemia virus), claimed to be the cause of chronic fatigue / fibromyalgia (Science 326: 585, 2009), isn't found by the Dutch in an established cohort: BMJ 340: c1018, 2010.
CHLAMYDIAL DISEASES
Chlamydia are degenerate bacteria that are obligate intracellular parasites. They must get their ATP from their host. The host response is neutrophilic. Chlamydia are readily phagocytized, but prevent lysosomes from fusing with the vacuoles. It is hard to get rid of these infestations, and often an uneasy equilibrium is established between host and parasite. Ornithosis ("Psittacosis", parrot fever) Infections by Chlamydia psittaci from inhaled bird droppings. Most any kind of bird can do it; the classic is parrots. (* Rare psittacosis from ewes causes sepsis in pregnant women: Thorax 46: 600, 1991.) The patients get neutrophilic pneumonitis / pneumonia. This can be fatal. In severe cases there is edema, bacterial superinfection. Giemsa shows inclusion bodies in the cytoplasm. Recovery is the rule after a few weeks. The infection may remain latent, and may recur.
Trachoma: A disease of the poor nations, and the world's most important cause of preventable blindness. Infection of the surface of the eye with an aggressive strain (A-C) of Chlamydia trachomatis, a micro-organism that flourishes in arid countries. Chlamydia reaches the eyes by means of fingers, fomites, or flies. The resulting inflammation produces proliferation of the conjunctival surface tissue ("pannus"). * Lymphoid follicles abound in this material, and help establish the diagnosis.
With enough scarring, the eyelids fail to close properly. Many of these people are also vitamin A deficient. With no access to antibiotics (or any medical care) blindness will result. * Good news: One dose of azithromycin seems to cure trachoma: Lancet 342: 453, 1993.
Inclusion conjunctivitis Not as bad as trachoma, but still not fun. Caught from people with genital chlamydia (fingers, getting born, un-halogenated swimming pools). The latter produces "swimming pool conjunctivitis".
Lymphogranuloma venereum (LGV) Infection of the anogenital region with aggressive Chlamydia trachomatis (* serotypes L-1, -2, or -3). Fortunately rare, this disease is encountered primarily in the tropics; U.S. cases have mostly been in gay men. The disease begins with a small ulcer at the site of inoculation. It spreads to the lymph nodes, which suppurate ("buboes"; there is a granulomatous admixture; "stellate microabscesses" rimmed by granulomas are typical). The disease does not become systemic. The end result is rectal strictures and/or elephantiasis. * You may also hear the term "genital ulcer - inguinal adenopathy disease" / "GUD", especially if chlamydia are not demonstrated to be present; herpes , chancroid, and syphilis
, chancroid, and syphilis can be mimics especially early-on (Sexually Transmitted Diseases 29: 253, 2002).
can be mimics especially early-on (Sexually Transmitted Diseases 29: 253, 2002).
{23386} LGV, histopathology
{23425} LGV, histopathology
* The old "Frei" skin test was made of ground-up tissue from these patients. No thanks.
Chlamydial urethritis / cervicitis Very common sexually transmitted diseases, usually caused by less virulent strains of Chlamydia trachomatis than cause LGV. This organism is our most important cause of "non-gonococcal urethritis" and "non-gonococcal cervicitis" (* not to mention "sterile pyuria"). Not emphasized enough by "Big Robbins" is that this is an important cause of fallopian tube infections ("pelvic inflammatory disease"), and it can be transmitted to the baby during birth. * Look for DNA probes as the future's preferred way of making the diagnosis of chlamydial genital infections. Rapid enzyme immunoassay to screen a man's urine to see if he has chlamydia on board: J. Fam. Pract. 33: 73, 1991. A 1980's claim about high-specificity chlamydial changes on pap smear was a disappointment. All about chlamydial infections in women: Hosp. Pract. 27(2): 175, 1992. Azithromycin for chlamydia was once the miracle-cure (NEJM 327: 921, 1992); now multi-drug resistant strains have emerged (J. Inf. Dis. 181: 1421, 2000).
Chlamydia pneumoniae ("TWAR", etc.) is an important cause of wheezy adult lung infections (JAMA 266: 225, 1991) and very likely a major player in much chronic asthma. More to come.
RICKETTSIAL DISEASES
Rickettsia are degenerate bacteria that cannot grow except within cells. They are never part of the "normal flora", and always indicate disease. * Ignore anything you may hear about "rickettsia being intermediate between viruses and bacteria". That's like saying whales are intermediate between mammals and fish, or that viruses are intermediate between living and non-living matter. * You can learn the archaic Weil-Felix reactions on your own. This tests cross-reactivity of particular rickettsia with certain Proteus strains.
All the rickettsia prefer to make their homes in the endothelial cells of the host. They are phagocytized and escape from the vacuole and multiply. Symptoms and signs in rickettsial disease are due to endothelial cell injury and release of noxious material into the circulation. In severe cases, there may be DIC, etc. The details are still elusive. The typical pathologic finding in a rickettsial disease is vasculitis, with damaged vessels surrounded by lymphocytes and macrophages. (Neutrophilic response to rickettsiae is very poor; if anything, the patient will be neutropenic.)
Antibody response to rickettsia is excellent (you'll make the diagnosis serologically, since you can't grow the bugs in the lab), and rickettsia can be effectively treated with tetracycline. Typhus fever ("louse-borne typhus", "epidemic typhus") A dread disease caused by Rickettsia prowazekii, transmitted by louse feces (rarely, flying squirrel fleas). Epidemics occur during wartime and famine (Burundi refugees: Lancet 352: 353, 1998). The American southern flying squirrel carries the organism. Patients have rash, headache, fever, mental changes, and even gangrene (from vasculitis). The essential pathology is swelling and necrosis of the endothelial cells in many parts of the body. (* You may read about "typhus nodules" in the brain; they are reactive glia mixed with inflammatory cells.) Death is not uncommon in untreated cases. It results from brain, heart, and lung involvement.
Between epidemics, the typhus rickettsia hides out somewhere in the body (to this day, no one knows where!). The infection may reactivate years later as the milder, but fully infectious Brill-Zinsser disease; a single case can start an epidemic among refugees. Philologists: Louse infestation is called "pediculosis". Typhus is the prototype of the "no eschar" family of rickettsial diseases, which also includes murine typhus, (* R. typhi), a milder illness caught from rat fleas. It is endemic wherever there is poverty. * R. conorii, which causes the milder "Mediterranean spotted fever", recently diverged from typhus rickettsia (Science 293: 2093, 2001).
 "Typhus", a short story
"Typhus", a short story
by Anton Chekhov, MD.
Chilling.  Rocky mountain spotted fever
Rocky mountain spotted fever (Med. Clin. N.A.
86: 351, 2002; NEJM
353: 551 & 587, 2005)
Named for the Rocky Mountains of Idaho where it was discovered, it's actually more common in the eastern US. This is an important zoonosis that still has a high mortality rate, and can leave survivors with deafness, brain damage, and/or gangrene.Rickettsia rickettsi is a tick-borne rickettsia that invades both endothelial and vascular smooth muscle cells. The most treacherous thing about this illness is that the rash doesn't appear for several days after the onset of symptoms. "Spots" may be hemorrhages from necrosis of the skin arterioles. Look for them everywhere, including on the palms and soles, also the scrotum/vulva. Patients are systemically sick, and the vasculitis and hemostatic chaos (hyper- or hypo-; Am. C. Clin. Path. 112: 159, 1999) can be fatal (ARDS) if untreated (tetracycline is best J. Inf. Dis. 184: 1437, 2001). There are about 37 deaths per year in the US (CDC estimate, Am. J. Trop. Med. 67: 349, 2002); often the illness is a surprise at autopsy and proved using molecular methods (J. Inf. Dis. 179: 1469, 1999.)
{05981} Rocky Mountain spotted fever, histology (necrosis and microthrombus in a small vessel)
{08145} Rocky Mountain spotted fever, face
{08146} Rocky Mountain spotted fever, wrist
{14281} Rocky Mountain spotted fever, bleeds from vasculitis
{14283} Rocky Mountain spotted fever, necrosis from vasculitis
Despite the name, Rocky Mountain spotted fever is most prevalent in the Appalachians....
Scrub typhus (tsutsugamushi fever) Caused by Orientia tsutsugamushi, carried by a mite, endemic throughout the Orient, but poorly studied. * Rapid diagnosis by immunostaining of the peripheral white cells: Am. J. Trop. Med. 65: 899, 2001. Past due.
African tick-bite fever, caused by R. africae and featuring an eschar at the inoculation site, is coming to be recognized more often in travellers, especially to Zimbabwe (Arch. Derm. 142: 1312, 2006). Q-fever A pneumonitis caused by Coxiella burnetti. The "Q" comes from Queensland, Australia, but this infection is found worldwide. The disease is common among sheep, and can be transmitted by ticks or by droplets. (Coxiella can tolerate drying, unlike the other rickettsia, and you can catch it from an animal or human sneezing at you.) * Future pathologists: If the disease goes systemic, you'll see little granulomas in various places. These are called "ring" granulomas, since for some reason a blob of lipid sits in their centers. A vaccine is available, recommended for slaughterhouse workers.* Bioweapons containing Q-fever were part of the U.S. arsenal in the 1960's.
Bacillary angiomatosis An opportunistic infections (AIDS patients) caused by either Bartonella henselae (the cat-scratch fever bug) or Bartonella (Rochalimaea) quintana (the trench fever bug; NEJM 323: 1573, 1581 & 1625, 1990). Dilated vessels in the liver, spleen, and elsewhere are typical. As you'd expect, these are collapsible bluish blobs. Bacteria can accumulate in masses dense enough to appear as granular "hyaline". The disease responds to antibiotics. The disease also affects inner-city drunkards (NEJM 332: 424, 1995). You're already familiar with bartonella as causes of Oroya fever and endocarditis. A new species pathogenic for humans: NEJM 356: 2381, 2007.
Ehrlichiosis ("Rocky Mountain spotless fever"; review Med. Clin. N.A. 86: 375, 2002): Recently-discovered rickettsial disease, caused by any of several Ehrlichia organisms, some of which infect granulocytes and others monocytes. This is a tick-borne zoonosis A new, mean strain of ehrlichiosis is becoming common (JAMA 272: 212, 1994; NEJM 333: 420, 1995). Still, most cases go unnoticed (Arch. Ped. 156: 166, 2002); it is an opportunist in the immunocompromised.
MYCOPLASMAL DISEASES
Mycoplasma (PPLO's, Eaton agent) are little (0.3-0.8 ) bacteria without cell walls (i.e. you can't kill them with penicillin or cephalosporin). They are the smallest free-living critters. Mycoplasma genitalium (J. Urol. 167: 1210, 2002; J. Urol. 159: 405, 1998) and Ureaplasma urealyticum are causes of "non-gonococcal urethritis". Mycoplasma pneumoniae is probably the commonest cause of a chest cold ("primary atypical pneumonitis"), generally with an upper respiratory infection. The incubation period is around two weeks. The disease can last for several weeks. Antibiotics speed recovery. For some reason, it causes production of cold agglutinins in half of patients.
Probably, most mycoplasma infections never come to the doctor's attention. Fortunately, mycoplasma infections are seldom fatal. * A new mycoplasma from AIDS patients: Lancet 338: 1415, 1991
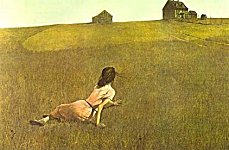
* PRESENT-DAY OPPOSITION TO IMMUNIZATION: "I don't care if
my kid makes the others sick." It affects your patients.
One of the most edifying stories in the history of science is the discovery of immunization. As late as the 1950's, the American public showered Jonas Salk, conqueror of the dread polio epidemic, with gratitude and appreciation. ("Gratitude" and "appreciation" were emotions that people in the past felt for their benefactors, particularly for scientists and physicians who fought and overcame diseases.) Today, few "issues" are more one-sided than the case for childhood immunization against diphtheria, measles
epidemic, with gratitude and appreciation. ("Gratitude" and "appreciation" were emotions that people in the past felt for their benefactors, particularly for scientists and physicians who fought and overcame diseases.) Today, few "issues" are more one-sided than the case for childhood immunization against diphtheria, measles , mumps
, mumps , polio
, polio , rubella
, rubella , tetanus
, tetanus , and whooping cough. However, under U.S. law, there are no penalties for deceiving the public about the safety and effectiveness of immunization. Most of your patients have heard, at one time or another, that they should not have their children immunized. And in the mid-1980's, most of the cost of certain vaccines went for the companies' liability insurance (NEJM 316: 1283, 1987). Active opponents of immunization include certain healing cults and primitivist sects, many traditional chiropractors ("it's cow pus"; court case Hanzel v. Arter, Federal Supplement Dec. 12, 1985), homeopaths (Br. Med. J. 310: 227, 1995), and other "alternative medical practitioners", the animal-rights militants (you'll be told that "polio
, and whooping cough. However, under U.S. law, there are no penalties for deceiving the public about the safety and effectiveness of immunization. Most of your patients have heard, at one time or another, that they should not have their children immunized. And in the mid-1980's, most of the cost of certain vaccines went for the companies' liability insurance (NEJM 316: 1283, 1987). Active opponents of immunization include certain healing cults and primitivist sects, many traditional chiropractors ("it's cow pus"; court case Hanzel v. Arter, Federal Supplement Dec. 12, 1985), homeopaths (Br. Med. J. 310: 227, 1995), and other "alternative medical practitioners", the animal-rights militants (you'll be told that "polio just went away, the vaccine had nothing to do with it"; see NEJM 315: 865, 1986), and certain "liberal green environmental activists" (Science 233: 704, 1986) and "conservative religious leaders". (Leaders within both movements compete with one another, and there is much to be gained by pretending to have something special to offer. Even if it is a complete fabrication, some people will want to believe it.) The best-known anti-immunization organization has (July 1999) no journal reference less than 14 years old on its anti-pertussis site. Thanks to anti-pertussis vaccine activism, the last quarter of the 20th century saw millions of excess cases and hundreds of dead or brain-damaged children throughout the countries that made DPT immunization optional (Lancet 351: 356, 1998; Swedish fiasco Ped. Infect. Dis. J. 6: 364, 1987; ongoing Italian fiasco Ped. Infect. Dis. J. 11: 653, 1992); by contrast, countries that continued to make DPT mandatory were spared. The publications of other anti-immunization organizations usually display the same pattern of obvious, intentional deception that have characterized other "spiritually and philosophically-motivated" pseudoscience campaigns. These include grossly misrepresenting what is contained in their scientific references, and simply making other stuff up. The links to big-money health quackery are obvious, and this is probably what drives these people. From time to time, you'll hear media stories about the supposed dangers of particular vaccines. The mid-1980's hype about pertussis vaccine being a major cause of brain damage and death resulted in tens of thousands of sick, and hundreds of dead, children. When the retrospective studies were done and the dust settled, it became clear kids are just as likely to develop the (mysterious) "brain lesions caused by pertussis vaccine" whether or not they've received the vaccine. There was a hype In early 1998 about "too much stimulation of the immune system too early" causing childhood diabetes, which of course is an autoimmune disorder. The scientific community rallied and examined this claim using retrospective analysis -- and of course it didn't hold up (Lancet 317: 159, 1998). A hype In the late 1990's about MMR vaccine causing autism didn't hold up to scrutiny; lay impressions probably result from the difficult of determining the time of onset of autism: Lancet 353: 2026, 1999. What clinched it for me is that among those claiming a link, there was no peak value for the interval between immunization and the supposed onset of autism (part of a huge Danish study NEJM 347: 1477, 2002). H-flu B vaccine as a cause of diabetes? Didn't hold up (Br. Med. J. 318: 1159, 1999). From 2000-2002, Congress was repeatedly treated to testimony from militants that thimerosal (a mercury-containing preservative that is passing into medical history) in MMR vaccine caused autism; actually the vaccine does not even contain the stuff. Hepatitis B vaccine and multiple sclerosis -- the anti-immunization people don't have the numbers, the vaccine prevents cancer and deaths, but the tort lawyers are already filing lawsuits against the manufacturer (Science 281: 630, 1998; Lancet 355: 549, 2000). It's clearly unethical to do a prospective, controlled study since the benefits are so obvious. "Exemptors" (i.e., kids whose parents got "religious or philosophical examptions" from the requirement that their kids be immunized; 1-2% of kids in many US states are "exemptors") are 35 times more likely to get measles
just went away, the vaccine had nothing to do with it"; see NEJM 315: 865, 1986), and certain "liberal green environmental activists" (Science 233: 704, 1986) and "conservative religious leaders". (Leaders within both movements compete with one another, and there is much to be gained by pretending to have something special to offer. Even if it is a complete fabrication, some people will want to believe it.) The best-known anti-immunization organization has (July 1999) no journal reference less than 14 years old on its anti-pertussis site. Thanks to anti-pertussis vaccine activism, the last quarter of the 20th century saw millions of excess cases and hundreds of dead or brain-damaged children throughout the countries that made DPT immunization optional (Lancet 351: 356, 1998; Swedish fiasco Ped. Infect. Dis. J. 6: 364, 1987; ongoing Italian fiasco Ped. Infect. Dis. J. 11: 653, 1992); by contrast, countries that continued to make DPT mandatory were spared. The publications of other anti-immunization organizations usually display the same pattern of obvious, intentional deception that have characterized other "spiritually and philosophically-motivated" pseudoscience campaigns. These include grossly misrepresenting what is contained in their scientific references, and simply making other stuff up. The links to big-money health quackery are obvious, and this is probably what drives these people. From time to time, you'll hear media stories about the supposed dangers of particular vaccines. The mid-1980's hype about pertussis vaccine being a major cause of brain damage and death resulted in tens of thousands of sick, and hundreds of dead, children. When the retrospective studies were done and the dust settled, it became clear kids are just as likely to develop the (mysterious) "brain lesions caused by pertussis vaccine" whether or not they've received the vaccine. There was a hype In early 1998 about "too much stimulation of the immune system too early" causing childhood diabetes, which of course is an autoimmune disorder. The scientific community rallied and examined this claim using retrospective analysis -- and of course it didn't hold up (Lancet 317: 159, 1998). A hype In the late 1990's about MMR vaccine causing autism didn't hold up to scrutiny; lay impressions probably result from the difficult of determining the time of onset of autism: Lancet 353: 2026, 1999. What clinched it for me is that among those claiming a link, there was no peak value for the interval between immunization and the supposed onset of autism (part of a huge Danish study NEJM 347: 1477, 2002). H-flu B vaccine as a cause of diabetes? Didn't hold up (Br. Med. J. 318: 1159, 1999). From 2000-2002, Congress was repeatedly treated to testimony from militants that thimerosal (a mercury-containing preservative that is passing into medical history) in MMR vaccine caused autism; actually the vaccine does not even contain the stuff. Hepatitis B vaccine and multiple sclerosis -- the anti-immunization people don't have the numbers, the vaccine prevents cancer and deaths, but the tort lawyers are already filing lawsuits against the manufacturer (Science 281: 630, 1998; Lancet 355: 549, 2000). It's clearly unethical to do a prospective, controlled study since the benefits are so obvious. "Exemptors" (i.e., kids whose parents got "religious or philosophical examptions" from the requirement that their kids be immunized; 1-2% of kids in many US states are "exemptors") are 35 times more likely to get measles , so go figure (JAMA 282: 47, 1999; they go on to infect the 10% or so of people in the community who are vaccine non-responders; I look forward to these irresponsible people being sued successfully.) For more on the risks to exemptors (measles and pertussis are still very much with us), see JAMA 284: 3145, 2000. I get quite a bit of E-mail from immunization opponents. One common claim is that "the diseases prevented by immunization are mild and easy to cure." This is a shameless, bald-faced lie. When I was a kid, one child in 1000 had brain damage after measles alone. You can cure congenital rubella
, so go figure (JAMA 282: 47, 1999; they go on to infect the 10% or so of people in the community who are vaccine non-responders; I look forward to these irresponsible people being sued successfully.) For more on the risks to exemptors (measles and pertussis are still very much with us), see JAMA 284: 3145, 2000. I get quite a bit of E-mail from immunization opponents. One common claim is that "the diseases prevented by immunization are mild and easy to cure." This is a shameless, bald-faced lie. When I was a kid, one child in 1000 had brain damage after measles alone. You can cure congenital rubella ? Paralytic polio
? Paralytic polio ? Would you like to have diphtheria (now rampant in the former Soviet Union, where immunization was discontinued)? Would you like your child to get lockjaw? What we don't emphasize (and maybe should) is that nowadays you're being asked to be immunized and have your kids immunized for the sake of your neighbors as much as (or more than) for your own safety. If you don't plan to travel, you're in more (though minimal) danger from the live polio
? Would you like to have diphtheria (now rampant in the former Soviet Union, where immunization was discontinued)? Would you like your child to get lockjaw? What we don't emphasize (and maybe should) is that nowadays you're being asked to be immunized and have your kids immunized for the sake of your neighbors as much as (or more than) for your own safety. If you don't plan to travel, you're in more (though minimal) danger from the live polio vaccine nowadays than from the wild disease. But if people start refusing the vaccine, it'll be epidemic once again. You are unlikely to save your life by taking a pertussis booster, but if you bring pertussis home to a baby too young to be immunized, the baby's life is in grave danger. This sort of thinking seems to be lost on today's activists. "Exercising your choice not to immunize your children" is irresponsible, not the least reason being that overcoming diseases depends on herd immunity. Much of anti-immunization activism boils down to parents saying, "I don't care if MY kid makes your kid sick." Also, see the Arch. Dis. Child. 1986 reference cited below for the article about how the parents of children crippled by pertussis felt about "the liberal media" afterwards.... To be blunt, anti-immunization rhetoric about "the pharmaceutical companies simply trying to make money" is disgusting. In fact, most of them have gotten out of the business because of all the anti-immunization harassment and liability.If you (the caring physician) attempt to argue with committed followers of these people, the discussion will boil down to, "Doctor, I like what they say, and I'll believe them rather than you." (People are all-too-eager to believe lies that makes them feel intellectually and morally superior.) But most people simply want your reassurance that the vaccines are, indeed, safe, valuable, and effective. Stay abreast of the changing vaccines, and give your best answer (I say, "Yes") from a solid knowledge base. Recent big review: JAMA 271: 1602, 1994. Paralytic polio
vaccine nowadays than from the wild disease. But if people start refusing the vaccine, it'll be epidemic once again. You are unlikely to save your life by taking a pertussis booster, but if you bring pertussis home to a baby too young to be immunized, the baby's life is in grave danger. This sort of thinking seems to be lost on today's activists. "Exercising your choice not to immunize your children" is irresponsible, not the least reason being that overcoming diseases depends on herd immunity. Much of anti-immunization activism boils down to parents saying, "I don't care if MY kid makes your kid sick." Also, see the Arch. Dis. Child. 1986 reference cited below for the article about how the parents of children crippled by pertussis felt about "the liberal media" afterwards.... To be blunt, anti-immunization rhetoric about "the pharmaceutical companies simply trying to make money" is disgusting. In fact, most of them have gotten out of the business because of all the anti-immunization harassment and liability.If you (the caring physician) attempt to argue with committed followers of these people, the discussion will boil down to, "Doctor, I like what they say, and I'll believe them rather than you." (People are all-too-eager to believe lies that makes them feel intellectually and morally superior.) But most people simply want your reassurance that the vaccines are, indeed, safe, valuable, and effective. Stay abreast of the changing vaccines, and give your best answer (I say, "Yes") from a solid knowledge base. Recent big review: JAMA 271: 1602, 1994. Paralytic polio among children in a Christian Scientist school: NEJM 288: 1357, 1973. Measles among members of a healing cult: MMWR 34: 718, 1985. Some (not all) Amish object to immunization (J. Inf. Dis. 163: 12, 1991). Dreadful rubella-induced
among children in a Christian Scientist school: NEJM 288: 1357, 1973. Measles among members of a healing cult: MMWR 34: 718, 1985. Some (not all) Amish object to immunization (J. Inf. Dis. 163: 12, 1991). Dreadful rubella-induced birth defects among the anti-immunization-subsect Amish (MMWR 40: 93 & 258, 1991, Ped. Infect. Dis. J. 14: 573, 1995; one Amish kid in 50 was affected.)By now, the case of Andrew Wakefield is history. Was he simply a cynical charlatan, or a decent man who thought he'd discovered something of great importance and fudged his data? I suspect the latter, but you decide.
birth defects among the anti-immunization-subsect Amish (MMWR 40: 93 & 258, 1991, Ped. Infect. Dis. J. 14: 573, 1995; one Amish kid in 50 was affected.)By now, the case of Andrew Wakefield is history. Was he simply a cynical charlatan, or a decent man who thought he'd discovered something of great importance and fudged his data? I suspect the latter, but you decide.
 The Anti-Immunization Activists
The Anti-Immunization Activists
The lying is unbelievable.
Ed's data. * INFECTIOUS DISEASE WORLDWIDE
Here are the World Health Organization's estimates of the leading infectious disease killers worldwide (1990; see Science 256: 1135, 1992). In my opinion, based on my reading of the rest of the literature, at least some these figures are ridiculously low. Acute respiratory infections... 6,900,000 deaths per year
Diarrheal diseases... 4,200,000
Tuberculosis ... 3,300,000
... 3,300,000
Malaria ... 1-2 million
... 1-2 million
Hepatitis... 1-2 million
Typhoid... 600,000
Measles ... 220,000
... 220,000
Bacterial meningitis... 200,000
Schistosomiasis ... 200,000
... 200,000
Pertussis... (almost all of these could be prevented by immunization) 100,000
Amoebiasis... 40,000-60,000
Hookworm... 50,000-60,000
Rabies ... 35,000
... 35,000
Yellow fever... 30,000
African trypanosomiasis... 20,000+
Keep your ears open: HTLV-II is endemic among First Americans ("Native Americans", "American Indians") in New Mexico (1.0-1.6% are positive). So far, there is not the expected increase in case of hairy cell leukemia, CLL, or mycosis fungoides.
Learning Objectives: The Bacteria The bacterial diseases are special. They are ubiquitous( they are deadly, and they are treatable. You should know the stuff on the common bacteria on this handout at the recall level. For "Pathology", do not worry about how to establish each diagnosis clinically, or about the morphology, gram staining properties, or taxonomy of the microbes. Know how they make people sick, and know the diseases well.
 Rhodococcus
Rhodococcus
Pittsburgh Pathology Cases INTRODUCTION TO THE BACTERIA
Until the development of antibiotics, most people died of the classic bacterial infections, which often struck during robust good health. Today, bacterial infections remain a primary focus for most physicians, and they are the final pathway out of life for many (if not most) people who are rendered more susceptible by serious disease (cancer, stroke, emphysema, Alzheimer's). In a way, almost all bacterial infection is "opportunistic", with the opportunities provided by host factors, known and unknown. For example, the presence of a foreign body (i.e., a suture or a piece of dirt) in a wound decreases the number of staphylococci necessary to establish a wound infection by several orders of magnitude. (What's probably happening is that bugs find sanctuary on the inert surface, where the phagocytes cannot devour them. Whatever the details, it works for them. Update on biofilms: JAMA 299: 2683, 2008.)
necessary to establish a wound infection by several orders of magnitude. (What's probably happening is that bugs find sanctuary on the inert surface, where the phagocytes cannot devour them. Whatever the details, it works for them. Update on biofilms: JAMA 299: 2683, 2008.) No one knows for certain why bullets don't work like other foreign bodies in causing infections.
More useful than the concept of "pathogenic" (disease-producing) vs. "non-pathogenic" (harmless) bacteria is the concept of virulence (i.e., the relative ability of the bacterium to cause disease). However, even virulent bacteria have asymptomatic carriers (remember Typhoid Mary). Also remember that most bacterial invasions are probably subclinical, i.e., the patient never recognizes that disease is present. When bacteria infect previously infected tissue (i.e., a viral pneumonia, a non-bacterial skin rash), we talk about superinfection.
All human bacterial pathogens have special ways to avoid being killed by phagocytes. The facultative intracellular bacteria even flourish inside phagosomes. It is not in the bacterium's interest to cause disease, and from an ecological perspective, our saprophytes are "more successful" than the bacteria that cause disease. Various pathogenic bacteria may harm us in any of several ways: Fast-growers deprive the host tissues of nutrients, and lower tissue pH. Despite pop claims, unless the blood supply is very severely impaired, this couldn't pose a serious problem. Many bacteria produce one or more factors, at least in vitro, which would seem potentially harmful. (As "Big Robbins" puts it: "All the leukocidins, hemolysins, hyaluronidases, coagulases, fibrinolysins, and other miscellaneous enzymes extracted from bacterial cultures act on their respective substrates in vitro, but their role in human disease remains presumptive.") However, known exotoxins (i.e., soluble molecules produced by living organisms that clearly do us harm) are relatively few. Broken-down cell walls release endotoxins (lipopolysaccharide protein complexes), which cause high fever, capillary permeability, shock, DIC. They disrupt neutrophils and cause macrophages to release preposterous amounts of IL-1 and α-TNF, which themselves will make you sick. Superantigens, which set off all of your B-cells or all of your T-cells, are obviously going to make you very, very sick. A few strains of Staph aureus uses T-cell superantigens as virulence factors; they include toxic shock syndrome toxin, staph enterotoxin B
uses T-cell superantigens as virulence factors; they include toxic shock syndrome toxin, staph enterotoxin B , and exfoliative toxins A and B (J. Immuno. 162: 4550, 1999.) There are also some strep
, and exfoliative toxins A and B (J. Immuno. 162: 4550, 1999.) There are also some strep superantigens. Of course, whenever phagocytes are activated, the body is likely to harm itself.
superantigens. Of course, whenever phagocytes are activated, the body is likely to harm itself.
TERMS
Bacteremia: Bacteria in the bloodstream, whether or not they are causing disease. Septicemia: Bacteria travelling around the body via the blood. Sepsis: Bacterial infection of the bloodstream, making the patient hypotensive or tachypneic (clinicians) or otherwise producing cardiovascular insufficiency (physiologists), in other words, septic shock.: Nature 420: 885, 2002, in other words, life-threatening systemic "inflammatory response" (?) due to bacteria in the bloodstream. The last three terms are confusing and the internists are just now trying to standardize the terminology (* "systemic inflammatory response syndrome", "sepsis", "severe sepsis", and "septic shock"; for criteria, see JAMA 273: 117, 1995). * "Pyemia" is a seldom-used term that means "pyogenic organisms" (loosely: staph , strep
, strep , gram-negative rods) infecting the blood.
, gram-negative rods) infecting the blood.
Nobody really understands the pathophysiology of septic shock. Current thinking focuses on 1. endotoxin (etc.) from dying bacteria overstimulates production of immune mediators (notably tumor-necrosis factor and interleukin-1-β) that push the body beyond what it can handle (J. Inf. Dis. 171: 393 & 472, 1995), and... 2. nitric oxide from macrophages, stimulated by the cytokine resonse etc. (Nature 372: 504, 1994; update NEJM 345: 588, 2001; NEJM 351: 159, 2004), and... 3. havoc wrought by neutrophil free radicals (which can be suppressed using -- surprise! --ibuprofen; watch for this... Br. J. Surg. 81: 1752, 1994). See also Crit. Care Med. 22(7): S-3, 1994; Ann. Int. Med. 120: 771, 1994. Well... these work in the animal models for sepsis in which huge numbers of bacteria and/or endotoxin are injected. But despite the "pop wisdom" that "sepsis is systemic inflammation", every therapy based on this idea that was tested in the 1990's proved to be a terrible failure (corticosteroids, anti-endotoxin antibodies, TNF-antagonists, interleukin-1 receptor antagonists all flopped). The failure of the much-ballyhooed nonoclonal anti-endotoxin antibody for sepsis: JAMA 283: 1723, 2000. In contrast to these failures is the considerable success of activated protein C against sepsis (other anticoagulants failed). Nobody knows which of the many effects of protein C this resulted from. More on what we know, and don't know, about the pathophysiology of sepsis: Am. J. Path. 170: 1435, 2007.
Lay-folk call sepsis "blood-poisoning". An episode of sepsis costs "somebody" $40,000 (JAMA 271: 1598, 1994).
Gram stain: The stain that stains gram-positive bacteria dark purple and gram-negative bacteria pink
PYOGENIC COCCI (round bacteria; "coccus" is Greek for "berry"; say "COX-eye", please, "cockeye" is ophthalmology)
This is a generic term for the familiar pathogenic gram-positive (staphylococci, streptococci, pneumococci) and gram-negative (neisseria) cocci. There is a striking neutrophilic response to these potent invaders. Spreading infections are called cellulitis (dumb name) or phlegmon (same root as "flame"). Of course, other microorganisms can "evoke pus" (i.e., be pyogenic).
STAPHYLOCOCCAL INFECTIONS
Staphylococci, including pathogenic strains, are normal inhabitants of the nose and skin of most healthy people. (Their favorite habitat is the hair follicles.) Virulence factors include coagulase (which clots blood), hemolysin, and protein A (which ties up Fc portions of antibodies). Although we have antibodies against staphylococci, they are of limited usefulness.
Staphylococci (and certain other microbes) also produce catalase, which breaks down H2O2, rendering phagocytes relatively helpless against them. The coagulase-positive staphylococcus (Staphylococcus pyogenes var. aureus) is a potent pathogen. It tends to produce localized infection ("because it produces coagulase, causing fibrin to wall it off"). It is the chief cause of bacterial skin abscesses. Infection spreads from a single infected hair (folliculitis) or splinter to involve the surrounding skin and subcutaneous tissues. Furuncles are single pimples, while carbuncles are pimple clusters linked by tracks of tissue necrosis which involve the fascia. Even though these usually pop and heal, they are never innocuous. Metastatic infections (most famously, to the heart valves, kidney or the cavernous sinus) and rupture into a body cavity (producing an empyema) are serious hazards. Staphylococcal sepsis is rare but serious. Today's patient with numerous, recurrent furuncles may be carring the PVL (Panton-Valentine leukocidin virulence factor) staph (BMJ 343: d5343, 2011).
{24478} carbuncle
{10985} carbuncle (histology; it's all pus)
{12227} furuncle
{24871} furuncle, skin of wrist
{24661} furuncle (histology; the eosin is strong making the dermis red)
{08979} acute folliculitis, histology of a pimple
Impetigo is a pediatric infection limited to the stratum corneum of the skin -- look for honey-colored crusts. (Often this is a mixed staph and strep infection; dermatologists recognize "impetiginization" when it superinfects another epidermal disease).
infection; dermatologists recognize "impetiginization" when it superinfects another epidermal disease).
{12128} impetigo
{14190} impetigo
{43771} impetigo
Staphylococcal infections of the nail-bed (paronychia) and palmar fingertips (felons) are especially painful and destructive. Don't confuse staph infections with acne, caused by Propionibacterium.  * Karl Marx, a hirsute man who seldom washed, was plagued by staphylococcal skin infections. He blamed capitalism, and proclaimed, "The bourgeoisie shall remember my boils!"
* Karl Marx, a hirsute man who seldom washed, was plagued by staphylococcal skin infections. He blamed capitalism, and proclaimed, "The bourgeoisie shall remember my boils!"
These staph are common causes of wound infections (including surgical wounds) and of a severe, necrotizing pneumonia. Both are serious infections in the hospitalized patient. Because of the extensive tissue destruction, wounds must be re-explored and all abscesses drained, while lung abscesses and bronchopleural fistulas are common in survivors of staphylococcal pneumonia. Staph is the most common cause of synthetic vascular graft infections. Certain sticky strains grow as a biofilm on the grafts (Lancet 359: 2166, 2002). Staph pneumonia is often preceded by a staph wound infection, influenza , or cystic fibrosis. It is less important (though listed in "Big Robbins") in chronic obstructive lung diseases.
, or cystic fibrosis. It is less important (though listed in "Big Robbins") in chronic obstructive lung diseases. * A vicious new strain of staph carrying the Panton-Valentine leukocidin (leukocidins punch holes in white cell membranes) causes lethal pneumonia in previously-healthy people: Lancet 359: 753, 2002.
Staphylococcal endocarditis -- a destructive infection of the heart valves -- is unfortunately still common, can involve either side of the heart, and can set up on a previously-normal valve. While Staph aureus can invade the gut directly ("invasive staphylococcal enterocolitis"), it is much more common to encounter food poisoning due to strains which have produced enterotoxin B, a pre-formed toxin in un-refrigerated meat or milk products (remember chocolate eclairs and milk-shakes). Victims drool, vomit, and suffer diarrhea for several hours. Other toxin-related staphylococcal diseases are toxic-shock syndrome (GI upsets, shock, conjunctivitis, rash, liver failure, kidney failure, and loss of skin, caused by strains producing shock syndrome toxin 1; remember the relationship to super-absorbent tampons left in place too long) and the pediatric scalded skin syndrome (a blistering disease caused by strains producing epidermolytic toxin).
{05946} toxic shock syndrome, skin starting to come off
Methicillin-resistant Staph aureus are the source of much alarm. They are usually carried on the hands of health-care personnel from one patient to another. For control, see Ann. Int. Med. 114: 162, 1991 and Am. J. Dis. Child. 143: 34, 1989. Changing back to hexachlorophene stops an epidemic, while "tracking down carriers" fails). A few strains are now also resistant to vancomycin (Postgrad. Med. 110(4): 43, 2001). Over the years, again and again handwashing proves the most successful way of keeping the hated organism at bay in the hospital (VA experience -- NEJM 364: 1419, 2011). With the epidemic abating, it's not clear whether the practice of isolating people found to carry MRSA has ever been wise; it's clearly not humane (Lancet 385: 1147, 2015.) However, most "hospital staph" is still sensitive (J. Inf. Dis. 162: 759, 1990). * People are still culturing patients' nostrils or skin in the absence of any evidence of infection just to find "carriers", who are then denied transfer to other institutions and kept quarantined. This is really stupid and is now being called rightly called unethical (Arch. Phys. Med. Rehab. 83: 1028, 2002); I suspect that the practice arose in response to the threat of equally-stupid lawsuits from people who pick up real infections ("My roommate was a carrier!") The new strains that are causing the dreadful necrotizing fasciitis acquired in the community work by recruiting and then killing neutrophils (Nat. Med. 13: 1510, 2007). The necrosis of the fascia results from the ability of these microbes to invade blood vessels.
Coagulase-negative staphylococci (Staphylococcus epidermidis) are skin commensals and opportunists that infect prosthetic heart valves (very important) and intravenous lines. They have been linked to an increasing number of other infections (Ann Int. Med. 110: 9, 1989). Remember that children with the neutrophil defect "chronic granulomatous disease" have great difficulty with staphylococci (JAMA 261: 1533, 1990).
STREPTOCOCCAL INFECTIONS
Streptococci live in the throats of healthy carriers, and cause sporadic and epidemic human disease. You remember the Lancefield groups: Group A: Strep. pyogenes, with many serotypes, is the familiar pathogen of "strep throat", common skin infections, etc. Group B: Newborns (NEJM 322: 1857, 1990); less often, severely compromised adults (JAMA 266: 1112, 1991). Group D: Enterococcus (lately Strep. fecalis, now its own genus), causes urinary tract infections, as well as endocarditis after below-the-belt procedures. This bug is notoriously antibiotic-resistant (thanks to all those local docs who prescribe third-generation cephalosporins for colds....) Strep. bovis sepsis: think colon cancer Can't type: Green (α-hemolytic) "viridans" streptococci are the classic agents of bacterial endocarditis on already-damaged valves
Virulence factors listed in "Big Robbins" are the capsular polysaccharides, M-proteins, streptokinase, streptodornase, and streptolysin A. Serologic tests include antistreptolysin O, with a rising or high titer indicating recent streptococcal infection. These tests are not sensitive or specific for streptococcal disease, but are worth ordering if you suspect post-streptococcal disease (rheumatic fever, post-strep glomerulonephritis).
Spreading streptococcal infections remain important causes of morbidity and mortality, especially among the poor. Streptococcal pharyngitis ("strep throat") is a disease of young people. Despite folklore about "seeing an exudate" (supposedly "pus"; actually you're seeing both enlarged lymphoid nodules and keratin plugs in the tonsillar pits), you cannot distinguish it reliably from a viral sore throat. Complications include retro-pharyngeal abscess (quinsy -- this killed George Washington by occluding his airway). Cellulitis of the deep tissues of the neck is Ludwig's angina. Both metastatic infections and post-streptococcal immune disease should be rare if penicillin treatment is instituted. Scarlet fever ("scarlatina") is a strep throat caused by a streptococcus with the gene to make one of the erythrogenic toxins. Patients have a rash (* it spares the skin near the lips); if the rash is biopsied, the pathologist will see many PMN's. This disease is infamous for producing immune post-streptococcal sequelae. Streptococcal infections are the bane of soldiers in boot camp. New work indicates they hide out in the throats of recruits who do not receive the prophylactic penicillin (NEJM 325: 92, 1991). Streptococcal skin infections may mimic any staphylococcal infections (even impetigo), but spreading cellulitis with obvious lymphangitis ("red streaks") is more typical. Erysipelas is a severe skin infection caused by group A strep; geographic of red, thickened, indurated areas of the skin are characteristic. Unlike staph infections, there is usually little or no tissue necrosis.
infections (even impetigo), but spreading cellulitis with obvious lymphangitis ("red streaks") is more typical. Erysipelas is a severe skin infection caused by group A strep; geographic of red, thickened, indurated areas of the skin are characteristic. Unlike staph infections, there is usually little or no tissue necrosis.
The "flesh-eater bacterium" of the 1994 media hoopla is an aggressive group A streptococcus strain that produces a rapidly-spreading necrotizing erysipelas and/or myositis and/or fasciitis and/or strep toxic shock syndrome. The bug has been around for decades, but is becoming more prevalent (Lancet 344: 1111, 1994). It killed muppeteer Jim Henson. Two virulence factors are pyrogenic exotoxin A, a super-antigen that causes activation of around 15% of all T-cells and thus overwhelms the body with its own cytokines, and pyrogenic exotoxin B, a cysteine protease that actually destroys the flesh. See Science 264: 1665, 1994. More recently, exactly what factors are really involved has become more difficult to say (J. Clin. Inv. 102: 550, 1998)... stay tuned. Streptococcal toxic-shock syndrome is mistaken for "evidence of child abuse" and a little girl dies: AJFMP 19: 93, 1998.
Puerperal sepsis ("childbed fever") resulted from group A streptococci carried on the hands of medical students. * Your medical education is not complete without learning the story of Ignatius Semmelweiss. The old tale about his dying of a strep infection after a cut from an autopsy was transferred to him. It was his junior colleague who died this way, after being jabbed by a medical student. Semmelweiss himself was probably beaten to death by attendants at a mental hospital.
Phlegmasia alba dolens ("milk leg") was a group A strep infection of deep venous thrombi, called by Osler "one of the three most terrible diseases". (There's a blue counterpart -- "cerulea"). Streptococcal pneumonia, like its staphylococcal counterpart, often superinfects viral pneumonia. Regardless of the site of infection, streptococcal pus is supposed to be thin and watery "because streptococci produce DNA-ase (dornase) and fibrinolysins". Obviously, you'll still get a culture. * Toxic-shock-like syndrome is a poorly-understood illness caused by certain strep, which are catching person-to-person: J. Inf. Dis. 175: 723, 1997.
counterpart, often superinfects viral pneumonia. Regardless of the site of infection, streptococcal pus is supposed to be thin and watery "because streptococci produce DNA-ase (dornase) and fibrinolysins". Obviously, you'll still get a culture. * Toxic-shock-like syndrome is a poorly-understood illness caused by certain strep, which are catching person-to-person: J. Inf. Dis. 175: 723, 1997.
Post-streptococcal hypersensitivity diseases include rheumatic fever, post-streptococcal glomerulonephritis, and some cases of erythema nodosum. You'll hear much more about these soon. Pneumococcal infections The pneumococcus (now Streptococcus pneumoniae) was called by Osler "the captain of the men of death", and popularly, "the old man's friend". It caused lobar pneumonia, a spreading lung infection that stopped only at the interlobar fissures. This is still a common terminal infection in debilitated people, though it can strike the young and healthy (who are treated with penicillin -- "the old man's enemy"). "Big Robbins" lists pneumococcus, Friedlander's bacillus, H. flu, legionella, and beta-hemolytic streptococci as the important causes of lobar pneumonia. Of these, the first two are the most important.
Today, we are more likely to see pneumococcal bronchopneumonia, middle ear infections, sinusitis, and meningitis (very common in adults). The organism thrives (with H. flu) in the large airways of smokers. Spontaneous pneumococcal peritonitis complicates ascites in cirrhotics and nephrotic syndrome patients. Pneumococcal sepsis, with or without an obvious primary site, is deadly; it is especially common in patients who are minus their spleens for whatever reason. Basic microbiology: The pneumococcus protects itself from the body's immune system by encasing itself in a polysaccharide capsule. The body must make separate antibodies against each of the 80 or so strains of capsule to fight the infection. * Ask your internist who should get the pneumococcal vaccine. A partial list: oldsters, nephrotics, ascitics, asplenics. It is very inexpensive and could easily be given to everyone in the poor nations, to their great benefit: Lancet 369: 389, 2007. For many years, the pneumococcus was notably sensitive to antibiotics. Things are changing (NEJM 331: 377, 1994). * The legend about Alexander Fleming's dad saving little Winston Churchill from drowning and thus obtaining the money for little Alex to go to medical school is the beautiful fabrication of two American Sunday-school teachers.
NEISSERIAL INFECTIONS
{08386} neisseria
Meningococcal infections Neisseria meningitidis ("meningococcus") is the familiar gram-negative diplococcus that is carried in the nose and throat of many healthy people. Virulence factors include an enzyme that cleaves α-heavy chains (gonococci have a similar enzyme), and its walls incorporate endotoxin. Meningococcus is most noted for causing small epidemics of bacterial meningitis, especially among young people. At special risk are military recruits and close contacts of patients. Sniffles precede the serious infection. You'll protect those exposed using rifampin prophylaxis. Sepsis without meningitis is also common. It produces the dread, rapid purpura fulminans, which is especially vicious because the microthrombi cause gangrene of the extremities (somehow the meningococcus depletes protein C). Meningococcus is the classic cause of Waterhouse-Friderichsen syndrome, deadly sepsis with collapse, myocarditis (this is one of the few times you might see neutrophils all through the myocardium), DIC, and hemorrhagic necrosis of the adrenal glands. "Any febrile illness with petechiae is meningococcal sepsis until proven otherwise", since with the others, you can afford to wait a few hours. NOTE: Today, W-F is more often due to pneumococci, H. flu, and other familiar agents. Meningococcal vaccine: JAMA 279: 435, 1998. Getting people, especially adults, to take it is very difficult, though it works pretty well.
{39103} meningococcemia (note the purpura)
{39106} meningococcemia
{40212} meningococcemia
{40213} meningococcemia
{46212} meningococcemia
{07570} Waterhouse-Friderichsen syndrome, adrenal
{08953} Waterhouse-Friderichsen syndrome, histology of adrenal
 Meningococcemia / DIC
Meningococcemia / DIC
Good teaching case
Pittsburgh Pathology Cases Gonococcal infections Neisseria gonorrhoeae is the classic cause of gonococcal urethritis in the male ("gonorrhea", you know the synonyms), inflammation of the cervix and Bartholin and Skene's glands in the female, and pharyngitis and proctitis in either sex. Symptoms appear 2-7 days after the unfortunate contact. Cervical infections in the female are often asymptomatic, some men become asymptomatic carriers as well, and the microbe is easily transmitted.
{12443} gonorrhea in the male
{25537} chancre (syphilis

) and gonorrhea
 Gonorrhea
Gonorrhea
Patient photos
Health Awareness Connection The infection is prone to spread to the eye (gonococcal conjunctivitis), especially in the newborn, or into the inner reproductive organs of either sex. Women are especially prone to gonococcal salpingitis (a pus-filled oviduct is a pyosalpinx), an important cause of both death and infertility ("hydrosalpinx", "chronic salpingitis", etc.), even in the U.S. It can also cause perihepatitis (Fitz-Hugh-Curtis syndrome). Young girls, whose vaginal mucosa is not mature, may get a vaginitis, but the mature vagina and endometrium are usually spared. The male testis is also spared. "Big Robbins" claims that gonococci can be transmitted on wet towels and linen. Depending on the site, gram-negative diplococci in polys may or may not be diagnostic of gonorrhea. Gonococcal sepsis is less common than meningococcal sepsis, but is similar. Gonococcal arthritis, the result of hematogenous spread, usually involves single joints. An episode of gonococcal urethritis may also be followed by reactive arthritis (formerly "Reiter's syndrome"), which you will study later.
People with hereditary deficiencies of any of the complement factors 5-9 are especially prone to neisserial sepsis. Mention should be made here of Branhamella, a gram-negative diplococcus once thought to be a "harmless commensal", which is now known to be an important cause of pneumonia in the elderly. (The omission by the new "Big Robbins" is surprising.)
GRAM NEGATIVE RODS
Along with the enterococcus, these are today's great opportunists, infecting hospitalized patients debilitated with other diseases, or who have been treated with antibiotics that favor their growth. The most worrisome complication of infection (or even infestation, in the impaired host) is the still-lethal gram-negative sepsis, ("septic shock", etc.) which kills by endotoxin release, DIC, or spread of organisms to set up infections throughout the body. Endotoxin supposedly relaxes capillaries and results in massive production of α-TNF, which in large quantities is bad for you. All about septic shock: JAMA 266: 548, 1991; Ann. Int. Med. 113: 227, 1990; E5 is mouse anti-lipid A and HA-1A is human anti-lipid A; $$$, HA-1A flops Ann. Int. Med. 121: 1, 1994). The anti-endotoxin E5531 mimics endotoxin structure and blocks endotoxin activity: Science 268: 80, 1995; another disappointment in the clinic but used in research. * The most recent work has focused on release of IL-1 and α-TNF from macrophages as the deadly business in septic shock. An α-TNF processing inhibitor protects against the lethal effects of endotoxin (Nature 370: 174, 1994). Maybe this'll help.
Escherichia coli infections result from certain strains of the familiar fecal organism. Most urinary tract infections (i.e., cystitis, pyelonephritis) are due to E. coli. It gains access by instrumentation (honeymoon, iatrogenic), or finds someone with a large residual volume of urine (i.e., an old guy with a prostate problem). Remember Proteus, Klebsiella, Pseudomonas, Enterococcus and Candida only in the severely obstructed or impaired host. Intra-abdominal suppuration: think E. coli, Enterobacter, or Proteus. Perirectal infections: think mixed organisms, including E. coli. E. coli remains among the great causes of gram-negative sepsis. (You'll hear the term urosepsis used for this condition.) E. coli pneumonia is not rare. You'll learn in microbiology about the various strains of E. coli which cause diarrhea by various mechanisms.
only in the severely obstructed or impaired host. Intra-abdominal suppuration: think E. coli, Enterobacter, or Proteus. Perirectal infections: think mixed organisms, including E. coli. E. coli remains among the great causes of gram-negative sepsis. (You'll hear the term urosepsis used for this condition.) E. coli pneumonia is not rare. You'll learn in microbiology about the various strains of E. coli which cause diarrhea by various mechanisms. * For example, enterotoxigenic (formerly "enteropathic") E. coli (ETEC / EPEC) has special fimbriae and sits on a little pedestal of actin and myosin and sends its own signals to the enterocytes (Science 267: 1621, 1995). * Oral vaccines against enterotoxigenic E. coli strains have been in the works for years: Lancet 338: 1285, 1991; J. Inf. Dis. 177: 796, 1998; Am. J. Trop. Med. 65: 120, 2001.
Klebsiella and Enterobacter infections Klebsiella pneumoniae ("Friedlander's bacillus") is a rod with a thick, gooey polysaccharide capsule that colonizes patients upon entry to the hospital. "Friedlander's pneumonia" is a necrotizing lobar pneumonia (especially in alcoholics) or necrotizing bronchopneumonia (in people with vulnerable airways). Both produce gooey (capsules) red mucus (one of the "current jelly" things). The microbe is notoriously hard to treat with common antibiotics. * The relationship, if any, of the real Dr. Friedlander (Karl, also a German) to your course director is presently unknown.
Enterobacter is a gram-negative rod with similar behavior to Klebsiella, through less slimy. Neither bug ever seems to affect the intestines.
Proteus and Serratia infections Proteus (several species) most often produces chronic urinary tract infections. Some strains obtain energy by splitting urea into carbon dioxide and ammonia, and this generates a characteristic odor and type of kidney stone. However, Proteus can affect most any tissue of the body, and produces intractable, suppurating infections. Serratia ("the red bug" -- some strains produce a red pigment), once considered another "non-pathogen", is another important cause of various infections. * Serratia outbreak due to a scrub nurse's artificial fingernails: J. Inf. Dis. 175: 992, 1997.
Pseudomonas ("the grape bug"; "the water bug") Once considered non-pathogens, Pseudomonas aeruginosa and its kin are now hated opportunists that flourish in people exposed to antibiotics that kill other microbes. Pseudomonas infections are especially common on the burn unit, in the lungs of cystic fibrosis patients (where it mutates to a mucoid strain: Am. J. Clin. Path. 128: 32, 2007), the ears of diabetics, and the blood of those with severe neutropenia. The pus may be fluorescent, and a grape fragrance is common. Pseudomonas sepsis is often preceded and/or followed by a necrotizing pneumonia. Ecthyma gangrenosum is a severe pseudomonas soft tissue infection. A virulence factor (exotoxin A) prevents assembly of peptides on ribosomes. Another toxin kills white cells. * Future pathologists: If you see a bacterial infection centered on the blood vessels, with thrombosis and bleeding, think of a pseudomonas etiology. Certain pseudomonas strains provide fluorescein (for fountains, immunofluorescent stains, and the manufacture of eosin).
Legionella infections (NEJM 337: 682, 1997) Everyone knows the story of the 1976 American Legion convention. The microbe had been causing sporadic cases and small outbreaks of pneumonia for decades, and the organism was found to thrive in air-conditioning systems, where it enjoys the company of certain amoebas and photosynthetic bacteria. It survives the water-treatment procedure, being chlorine-resistant. Person-to-person contact hasn't been documented. The bugs are hard to stain and hard to grow (* use charcoal yeast agar), which is why they took so long to discover. Today, we see them using immunofluorescence or the Dieterle silver stain. Cigaret smoking, chronic lung disease, and being on glucocorticoids all put you at risk.* Growing in standing water makes some of the bugs more virulent, since they grow flagellae if they multiply within amoebas.
smoking, chronic lung disease, and being on glucocorticoids all put you at risk.* Growing in standing water makes some of the bugs more virulent, since they grow flagellae if they multiply within amoebas.
{26972} legionella pneumonia, H&E (this is just neutrophils in the alveoli)
{26975} legionella, Dieterle silver stain (black speckles are the bugs)
{08179} legionella
Pontiac fever is a mild febrile illness. Legionnaires' disease is a vicious bronchopneumonia (some polys, lots of mononuclear cells) which is likely to be fatal unless an appropriate antibiotic is administered. Those most at risk are smoker-drinkers.
Anaerobic Gram negative infections (i.e., bacteroides, fusobacterium, peptococcus, peptostreptococcus; the most notable are Bacteroides melaninogenicus above the diaphragm and Bacteroides fragilis -- often antibiotic-resistant -- below the diaphragm) These cause suppurative and spreading infections. The bad smells are famous. Many of these are caused by mixes of bugs, including gas-producers ("synergistic anaerobic gangrene"). Look for thin, bubbly, dirty-looking "dishwater" pus. Most lung abscesses are mixed aerobic and anaerobic, especially in people with rotten teeth. The anaerobic component is often unrecognized. One nice thing about these infections is that draining them exposes them to air, killing the microbes.
Hemophilus influenzae infections This coccobacillus causes infections (especially meningitis and pneumonia) in children who are not fully immune-protected (peak age 1 year; it remains the foremost cause of meningitis from 1 month to 5 years). About 600,000 die worldwide each year from H. flu (Nat. Med. 10: 1277, 2005). Older children are more prone to conjunctivitis ("pink eye"), epiglottitis ("croup") and life-threatening laryngotracheobronchitis, and H. flu lung infections are common in smokers. Occasionally, its causes suppurative infections at other sites. The most virulent strain is type B, which has a capsule. With the introduction of the Hib vaccine for toddlers, the occurrence of serious H. flu B infections has dropped 71% (JAMA 269: 221, 1993). H. aphrophilus ("doggy-breath bug") occasionally causes soft-tissue infections in humans. Hemophilus ducreyi causes chancroid, a rare sexually-transmitted disease of those with poor personal hygiene. It is rare in the U.S.
Whooping cough Bordetella pertussis does not invade, but flourishes among the cilia of the respiratory epithelium (the virulence factor permits tight adhesion). Here it produces an exotoxin that causes malaise, fever, excess circulating lymphocytes ("lymphocytosis"; the toxin apparently keeps T-cells from leaving the bloodstream and entering the tissues Am. J. Clin. Path. 114: 35, 2000), greatly exaggerated cough reflex ("whooping cough"), and local tissue damage. The key to recovery is IgA antibodies (from infection, vaccine, or * exogenous high-dose immunoglobulin: Lancet 338: 1230, 1991). Violent coughing ruptures airways, causes brain hemorrhages, etc., etc. Anecdotal evidence also relates whooping cough to longstanding bronchiectasis (incurable, running sores of the airways), but usually recovery is complete in a month or two. The classic whole-cell pertussis vaccine is noxious, and often causes pain at the injection site, but "brain damage caused by whooping cough vaccine" is almost certainly a myth, the relationship being coincidental (JAMA 261: 1641 & 1679, 1990; JAMA 271: 37, 1994). A 1980's campaign by European "alternative medical thinkers" against the whooping cough vaccine resulted in a large epidemics (notably in West Germany and Sweden, where the rates of infection reached 1 person in 1000 per year, like in the Third World: Lancet 351: 356, 1998), with a few hundred children killed or maimed (Arch. Dis. Child. 61: 382, 1986; the parents of these kids were upset with the media afterwards). So much for the bunk about "those diseases just went away, immunization had nothing to do with it" Similar small outbreaks occurred in the U.S. in the 1980's, and will occur again. A "vaccine victims compensation law" encouraged the public to attribute various bad things to the pertussis vaccine. The acellular vaccine (JAMA 269: 53, 1993) is not so immunogenic, but less likely to cause local pain (Pediatrics 97: 279, 1996). Immunity eventually wears off. Remember pertussis in adults who have a cough: Arch. Int. Med. 151: 1510, 1991; J. Inf. Dis. 182: 1409, 2000; J. Inf. Dis. 183: 1353, 2001; around 12% of coughs lasting more than two weeks turn out to be pertussis (JAMA 275: 1672, 1996).
Diphtheria Corynebacterium diphtheriae is a classic respiratory pathogen that still causes much disease. In the U.S., it occurs almost exclusively in illegal immigrants. Virulent strains are infected with a toxin-coding phage. The is a potent inhibitor of protein synthesis, and a single molecule within a cell will kill the cell. Worst-affected are heart and muscle. The bacterium does not invade, but produces surface necrosis in the airways, leading to the formation of a fibrinous pseudomembrane packed with toxin-generating organisms. If the membrane slips off, the child may choke to death. Diphtheria is now rampant in the former Soviet Union: Lancet 347: 1739, 1996.
{19946} diphtheria, tonsils
{24489} diphtheria, membrane (trachea is opened from behind)
* Frontiers of biotechnology: A "fusion toxin" is designed to kill cells that bear a particular receptor. It is composed of the ligand joined to diphtheria toxin ("diftitox"), pseudomonas toxin, or anthrax toxin. A hybrid of interleukin and diphtheria toxin shows promise in the treatment of T-cell lymphoma, and there are many other likely uses. Stay tuned. Erythrasma is a curious jock-itch / armpit-itch that fluoresces bright scarlet; it's caused by a diphtheroid. * The innumerable, banal "diphtheroids" include Corynebacterium xerosis, the guy's-armpit smell bug, and Propionibacterium acnes, the acne bug.
toxin. A hybrid of interleukin and diphtheria toxin shows promise in the treatment of T-cell lymphoma, and there are many other likely uses. Stay tuned. Erythrasma is a curious jock-itch / armpit-itch that fluoresces bright scarlet; it's caused by a diphtheroid. * The innumerable, banal "diphtheroids" include Corynebacterium xerosis, the guy's-armpit smell bug, and Propionibacterium acnes, the acne bug. Science marches onward. Br. J. Derm. 124: 596, 1991 identified 5α-androstenone and 3α-androstenol as important in men and virilized women, as did J. Chrom. 562: 647, 1991 and J. Steroid. Bioch. Mol. Bio. 40: 587, 1991. The last group considers these to be pheromones: "So far, there is some evidence that both sex pheromones may have similar functions in humans as in boars", i.e., a grown man is supposed to smell like a pig. In both sexes, there's also a major contribution from E-3-methyl-2-hexenoic acid, which as it turns out is manufactured for the purpose and even has its own transport protein from which the bacteria liberate it (Experientia 51: 40, 1995). Wow! Nature has gone to a good deal of effort to make us stinky.
ENTERIC PATHOGENS
Bacteria cause diarrhea by three known mechanisms: 1. They can invade the gut wall directly. Diarrhea results from the inflammatory exudate, and the stools will contain polys. 2. They can release enterotoxins, either into the gut or into food. Don't expect to see anatomic pathology, or polys in the stool. 3. They can attach to mucosal cells and cause them to secrete too much water ("enteroadhesive bacteria"). Don't expect to see anatomic pathology or polys in the stool in these cases, either.
E. coli Invasive strains (mostly O-group) are rare in the U.S., except in the Southwest. "Toxigenic E. coli" (also mostly O-group) produce an heat-labile enterotoxin that, like cholera toxin, makes the enterocytes pump water into the lumen. Much "Montezuma's revenge" is now attributed to these strains. Enteroadhesive E. coli are now being recognized.
Salmonella infections fall into three groups. Salmonella typhi produces typhoid fever (BMJ 333: 78, 2006; Lancet 385: 1136, 2015), fortunately very rare in the U.S. nowadays. Typhoid review NEJM 347: 1770, 2002. The transmission is by the fecal-oral route, especially when sanitation is poor. Carriers ("Typhoid Mary", many others) harbor the bugs in their gallbladders (with or without stones), and can transmit them through body excretions. They may also suffer episodes of salmonella sepsis without an obvious source. After ingestion, the organisms silently damage and penetrate the bowel epithelium, and enter the lymphoid tissue in and near the bowel. Incubation period is 1-2 weeks, during which the Peyer's patches become huge. Finally, they ulcerate and start to ooze, and the patient become symptomatic.) "Rose spots", erythematous skin lesions that blanch on pressure, are characteristic. Making the call is often difficult, and some people regard any "fever of unknown origin" lasting a week or more in a typhoid zone to be typhoid until proved otherwise. After a few weeks, the patient has either recovered or died. Especially early in the disease, blood cultures are much more likely to be positive than stool cultures. However, even blood cultures are only 50% sensitive, and the IgM serology isn't practical in the field. The new PCR technologies now seem to define the disease when diagnosis is questionable. Hepatosplenomegaly and spiking fevers are typical. There are many dreaded complications, the most famous of which is bowel perforation. The anatomic pathology is picturesque. Look for lots of macrophages in the gut; they are so turned-on by the disease that they eat red cells. The spleen is packed with macrophages, too. There is a curious lack of neutrophils, either in the lesions or the circulating blood. * Future pathologists: If the long axis of the ulcer is parallel to the long axis of the bowel, it's typhoid or yersinia; if it's perpendicular, it's tuberculosis . This was a big deal when deaths from both conditions were commonplace.
. This was a big deal when deaths from both conditions were commonplace.
* Supposedly there is no animal reservoir for typhoid, but since there are many human carriers, eliminating it will probably be impossible. The new vaccines use a potentiated Vi antigen, one of the virulence factors that distinguishes typhoid from most other salmonella organisms.
{26369} typhoid ulcers, small intestine
{49172} typhoid ulcers, small intestine
{32078} typhoid microabscess, liver | 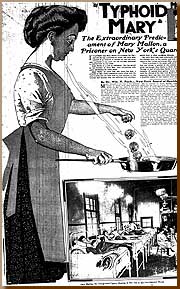 |
 Typhoid ulcers of the intestine
Typhoid ulcers of the intestine
Classic drawing
Adami & McCrae, 1914 Other salmonella cause enteric fever, i.e., a mild variant of typhoid (remember S. cholerasuis -- pig-cholera bug -- , S. typhimurium (now largely drug-resistant and quite serious), and S. paratyphi), plain food poisoning (vomiting, diarrhea), or sepsis. These organisms invade the gut mucosa. Exactly how they do their mischief is unclear. Some vicious strains in Africa invade the bloodstream and can cause up to 25% mortality where HIV, malaria, and/or TB put the patients at additional risk ("emerging disease"; Lancet 379: 2489, 2012). Raw eggs and raw poultry teem with salmonella. Salmonella concerns also caused the Federal ban on pet turtles (* selective indignation -- see the upcoming unit on "tobacco"). * The iguana connection: MMWR 41: 38, 1992; Arch. Dis. Child. 77: 345, 1997; Pediatrics 99: 399, 1997. * The 1994 Schwann Ice Cream Fiasco, in which the ingredients were contaminated in a truck used to transport unpasteurized eggs, was the largest known U.S. Salmonella outbreak, with 224,000 sick folks.* The nationwide 2008 outbreak was caused by raw Mexican peppers (NEJM 364: 918, 2011).z* Achlorhydria from any cause places people at greater risk for all the salmonella organisms. Why might this be? * Prior to the 2001 anthrax attack, the only bioterrorist attack in the US was by the Rajneeshie cult, which grew S. typhimurium at their commune and infected salad bars in Oregon in 1984 (JAMA 278: 389, 1997). The intent was to make the town sick on election day, so that the cultist candidates would win. Two cultists were sentenced to only 4 1/2 years each.
Ingesting only a few salmonella organisms will not usually produce disease. Gastric acid is an important barrier (antacid and Tagamet users take note; achlorhydrics are plagued by salmonella infections). Sickle cell patients are prone to salmonella osteomyelitis (nobody knows why). People with schistosomiasis are prone to longstanding salmonella infections (the salmonella hide out in the schistosome's coat). * Infection of atherosclerotic plaques is usually salmonella: Am. J. For. Med. Path. 23: 382, 2002. Salmonella still kills, especially children, the elderly, and the debilitated: JAMA 266: 2105, 1991.
are prone to longstanding salmonella infections (the salmonella hide out in the schistosome's coat). * Infection of atherosclerotic plaques is usually salmonella: Am. J. For. Med. Path. 23: 382, 2002. Salmonella still kills, especially children, the elderly, and the debilitated: JAMA 266: 2105, 1991.
Don't worry right now about the various antigens of salmonella organisms.
Shigella infections ("bacillary dysentery") Shigella organisms can cause disease even when only a few are ingested, and small outbreaks can occur under unsanitary conditions (yes, houseflies do transmit it: Lancet 337: 993, 1991). The organisms multiply inside enterocytes, damage the tissue of the colon, producing a fibrinous acute inflammatory picture. Incubation period is a day or two, after which the patient suffers a memorable diarrhea. Fortunately, they do not spread beyond the gut, and after treatment, the mucosa regenerates. * A recombinant E. coli that absorbs shiga toxin: Nat. Med. 6: 265, 2000.
{49213} shigella in the gut
Shigella and Yersinia enterocolitica are notorious for producing a seronegative spondyloarthritis and/or anterior uveitis if, and only if, the patient is HLA-B27 positive. Exactly how this happens remain quite controversial, with conflicting claims and no resolution in sight.
Vibrio family (Lancet 363: 223, 2004)  Cholera, caused by the freshwater bug V. cholerae bearing the CTX#&934;, remains an important cause of mortality around the Ganges, where it is endemic. Pandemics have caused tremendous mortality. The bacteria do not invade, but cause diarrhea entirely by producing an enterotoxin that activates adenyl cyclase in enterocytes. This causes secretion of interstitial fluid. The mild disease looks like any other diarrhea. The severe disease is unmistakable, with massive water loss. Fluid replacement results in complete recovery. Cholera is still rampant in much of Africa thanks to lack of access to safe drinking water and decent sanitation, and mortality remains high because of lack of access to health care (NEJM 360: 1060, 2009). Two oral vaccines are now available and we may hope they will have some impact (Lancet 379: 2466, 2012). Happily, there have been few cholera epidemics in the past two decades, except the one in Peru. * Medical history: Dr. John Snow, London's medical sleuth, ended a cholera outbreak by removing the handle from the Broad Street pump. Cholera in Peru: MMWR 40: 844, 1991. Cholera from imported coconut milk: MMWR 40: 860, 1991. Cholera returns to the U.S.: JAMA 267: 1495, 1992). Cholera and incompetent health care delivery systems kill people in the Rwandan outbreak: Lancet 345: 359, 1995. Oral vaccines are promising. Non-cholera vibrios (V. parahemolyticus, V. vulnificus and others cause skin infections and sepsis; the latter usually occurs in alcoholics who have eaten raw seafood, and vulnificus is famous for huge masses of bacteria with no inflammatory reaction. Iron overloading of the body greatly increases vulnerability (Arch. Int. Med. 151: 1606, 1991).
Cholera, caused by the freshwater bug V. cholerae bearing the CTX#&934;, remains an important cause of mortality around the Ganges, where it is endemic. Pandemics have caused tremendous mortality. The bacteria do not invade, but cause diarrhea entirely by producing an enterotoxin that activates adenyl cyclase in enterocytes. This causes secretion of interstitial fluid. The mild disease looks like any other diarrhea. The severe disease is unmistakable, with massive water loss. Fluid replacement results in complete recovery. Cholera is still rampant in much of Africa thanks to lack of access to safe drinking water and decent sanitation, and mortality remains high because of lack of access to health care (NEJM 360: 1060, 2009). Two oral vaccines are now available and we may hope they will have some impact (Lancet 379: 2466, 2012). Happily, there have been few cholera epidemics in the past two decades, except the one in Peru. * Medical history: Dr. John Snow, London's medical sleuth, ended a cholera outbreak by removing the handle from the Broad Street pump. Cholera in Peru: MMWR 40: 844, 1991. Cholera from imported coconut milk: MMWR 40: 860, 1991. Cholera returns to the U.S.: JAMA 267: 1495, 1992). Cholera and incompetent health care delivery systems kill people in the Rwandan outbreak: Lancet 345: 359, 1995. Oral vaccines are promising. Non-cholera vibrios (V. parahemolyticus, V. vulnificus and others cause skin infections and sepsis; the latter usually occurs in alcoholics who have eaten raw seafood, and vulnificus is famous for huge masses of bacteria with no inflammatory reaction. Iron overloading of the body greatly increases vulnerability (Arch. Int. Med. 151: 1606, 1991). Vicious Vibrio parahemolytus outbreak from monitored oyster beds: JAMA 284: 1541, 2000.
Helicobacter (formerly Campylobacter): Once considered a non-pathogen ("Vibrio comma"), we now attribute many cases of diarrhea to C. jejuni. The organism is not easy to grow; various strains cause disease by any of the three mechanisms outlined above. We'll study later about H. pylori in ulcer disease, or read all about it (NEJM 324: 1043, 1991) and how killing the bug is the best way to deal with ulcers (NEJM 332: 139, 1995). Yersinia enterocolitica is another newly-recognized cause of dysentery; it may account for "zoonotic appendicitis" (Br. Med. J. 303: 345, 1991). Bacillus cereus ("the fried rice bug") is another famous cause of food poisoning. Clostridium perfringens can produce food poisoning, with nausea and vomiting, following ingestion of its pre-formed toxin. For the latter two, see Lancet 336: 982, 1990. NOTE: "Gay bowel syndrome" (common in gay men during the "fast lane" era) can be caused by most of the above organisms, or by gonorrhea, giardia, amebiasis, herpes , or other viruses.
, or other viruses.
CLOSTRIDIA: An ancient family of sporulating gram-positive strict anaerobes, common in the gut and in the outside world, but rarely troublesome.
* "The earth used to belong to the anaerobes." As you remember, the rock evidence shows that oxygen first appeared in the atmosphere around 2.4 billion years ago, the result of the appearance of the cyanobacteria (update Sci. Am. 298(4): April 2008. Unlike most infectious agents, these organisms "want us dead", since they specialize in decomposing dead bodies. They produce their awful toxins only when growing under optimal circumstances and without other bacteria. This is good, because a wine-glass full of either tetanus or botulism
or botulism toxin, properly distributed, could kill the human race. (The U.S. destroyed its botulinum
toxin, properly distributed, could kill the human race. (The U.S. destroyed its botulinum toxin arsenal, which amounted to tons, in the 1960's.)
toxin arsenal, which amounted to tons, in the 1960's.)  Tetanus, caused by Clostridium tetani which produces tetanospasmin, is characterized by spasm of voluntary muscles ("lockjaw", "sardonic smile", "opisthotonos", etc.). Tetanus spores are ubiquitous (horse and cow dung teem with the organisms), but will not germinate in the human gut. If introduced into necrotic tissue in a wound (i.e., a war wound, a farm wound, a rusty nail puncture, etc.), the organisms germinate and elaborate their toxin, which cannot be neutralized once it has been bound to the inhibitory neurons of the spinal gray matter. Death results from respiratory failure. The lesion is molecular, and there is no anatomic pathology apart from the wound itself, which may look trivial. (Your mother specifically warned you about rusty nails; the rust particles probably get left in the wound and having foreign bodies helps the infection get going.) Most Americans are immune (NEJM 332: 761, 1995), and pretty much all tetanus in kids is due to parents' "philosophical objections to immunization" (Pediatrics 109: E2, 2002). By contrast, tetanus is rampant in Vietnam, and is often iatrogenic (Lancet 344: 786, 1995); in the poor nations, it often follows an abortion or a messy delivery (Lancet 354: 565, 1999.
Tetanus, caused by Clostridium tetani which produces tetanospasmin, is characterized by spasm of voluntary muscles ("lockjaw", "sardonic smile", "opisthotonos", etc.). Tetanus spores are ubiquitous (horse and cow dung teem with the organisms), but will not germinate in the human gut. If introduced into necrotic tissue in a wound (i.e., a war wound, a farm wound, a rusty nail puncture, etc.), the organisms germinate and elaborate their toxin, which cannot be neutralized once it has been bound to the inhibitory neurons of the spinal gray matter. Death results from respiratory failure. The lesion is molecular, and there is no anatomic pathology apart from the wound itself, which may look trivial. (Your mother specifically warned you about rusty nails; the rust particles probably get left in the wound and having foreign bodies helps the infection get going.) Most Americans are immune (NEJM 332: 761, 1995), and pretty much all tetanus in kids is due to parents' "philosophical objections to immunization" (Pediatrics 109: E2, 2002). By contrast, tetanus is rampant in Vietnam, and is often iatrogenic (Lancet 344: 786, 1995); in the poor nations, it often follows an abortion or a messy delivery (Lancet 354: 565, 1999. At the turn of the millennium, around 277,000 babies die of tetanus every year from umbilical cord infections. It's now down to 58,000 or so, and an unknown number of mothers, and this is still too high (Lancet 385: 362, 2015). * See Lancet 358: 640, 2001 for an account of neonatal tetanus among the traditional Masai, where 1 child in 10 (!) dies as a result of the practice of plastering the umbilical stump with cow manure. Concerned physicians met with the tribe's "indigenous healers" and persuaded them to change the ritual to one involving milk or boilied water. This dropped the death rate to near zero. When one of the chief witch doctors in the town died, the locals immediately went back to using cow manure and the children started dying again. There is more here than just stupidity. * See MMWR 47(43): 928, 1998 for the weird story of an anti-immunization family whose child (unprotected by maternal antibody) developed neonatal tetanus. Although she considered immunization unsafe, the mother gave her child a horrible mixed anaerobic infection of the umbilical stump by plastering it with "health and beauty clay" (ironically from Death Valley). Even after the child recovered, she wouldn't have it immunized because of "concern about potential adverse effects."
 Tetanus
Tetanus
Brazilian man
CDC Botulism (Br. Med. J.
305: 264, 1992) is a paralyzing food poisoning resulting from the ingestion of pre-formed toxin of
Clostridium botulinum. Less often, the organisms can produce toxin when infecting a wound (black tar heroin injectors take note: JAMA
279: 859, 1998), or infesting the gut of a baby fed honey (all-too-common, Am. Fam. Phys.
65: 1388, 2002). This always begins as cranial nerve weakness. The motor end plates are damaged by the toxin, and although full recovery is usual, some patients are left chronically weak. Electromyographers notice a distinctive pattern. Again, death results from respiratory paralysis, and the anatomic pathology is unimpressive. ("Botulism" is named for home-prepared sausage, and today botulism infections usually result from sloppy home-canning techniques.) Eskimo botulism: West. J. Med.
153: 390, 1990. Botulism as a possible weapon of mass destruction: JAMA
285: 1059, 2001. An antibody against botulism is useful in treating the illness (NEJM
354: 462, 2006. Therapeutic uses of botulinum toxin began in the late 1980's and range from achalasia to blepharospasm to torticollis to strabismus to wrinkles.
Septic clostridial infections usually are caused by
Clostridium perfringens. They may take the form of a necrotizing cellulitis, or frank myonecrosis with gas production (
gas gangrene). The latter typically follows dirty wounds (war wounds, amateur abortions). A vicious cycle develops, with anaerobiosis promoting clostridial growth, and clostridial tissue damage further promoting anaerobiosis. The gas is produced by fermentation. Clostridial lecithinase (
alpha-toxin) released into the bloodstream cause striking hemolysis. Gas gangrene stinks, yields only a thin, watery (i.e., much-hydrolyzed) exudate, and progresses rapidly; some infections by other bacteria mimic this. Don't even expect to see an inflammatory infiltrate in gas gangrene.
Of course, clostridia are only one of several types of anaerobes that produce the foul-smelling, often mixed infections of wet gangrene. * Enteritis necroticans is basically clostridial gas gangrene of the small intestine, appearing in people who are already seriously sick or malnourished. It usually begins at the origin of the jejunum and proceeds a variable distance distally. It is common in the poor nations, where it is called "pigbel" (NEJM 342: 1250, 2000.
Pseudomembranous colitis is caused by toxin-producing
Clostridium difficile, which overgrows the gut when antibiotics are administered. Focal necrosis of the surface mucosa is followed by inflammation and fibrin exudation, which produce the "pseudomembrane" and diarrhea.
THE BACTERIAL ZOONOSES
Anthrax is caused by Bacillus anthracis, a gram-positive rod notorious for its virulence. * In the 1980's in these notes I predicted this bacterium, which survives as very durable, very infectious spores, would become a terrorist weapon. The Sverdlovsk episode: Proc. Nat. Acad. Sci. 90: 2291, 1993; Am. J. Path. 144: 1135, 1994; JAMA 281: 1735, 1999. Anthrax typically follows skin contact with contaminated animal parts. The first lesion (the "malignant pustule") is filled with dark purple, broken-down blood, and is surrounded by a spreading phlegmon. The pustule ruptures and becomes necrotic (the black "eschar" for which anthrax, i.e., "the black disease", is named). The lesion may eventually heal, or involvement of the blood may carry the disease to other organs. Inhaled spores produce anthrax pneumonia (the deadly "woolsorter's disease"). Exactly how anthrax works from the pathologist's perspective is still being puzzled out. There are three toxins (protective antigen, lethal factor, edema factor) which work in concert. I suspect that the eschar results from the action of the agent that causes loss of cytoplasmic contents; stay tuned. Review Sci. Am. 286(3): 48, 2002; update Nat. Med. 9: 996, 2003.
Listeriosis, human infection with the veterinary pathogen Listeria monocytogenes (* "the Chinese pictogram bug"), produces amnionitis and fetal inflammation ("granulomatosis infantiseptica") following asymptomatic infections of the maternal bloodstream. It is also coming to be recognized as an opportunist among the immunosuppressed. This is a bug to watch as a major pathogen of the future. An epidemic of listeriosis in Britain in which paté was suspect: Br. Med. J. 303: 773, 1991. A batch of bad chocolate milk: NEJM 336: 100, 1997. Tainted cantaloupe launches the "Listeria initiative" with far-reaching effects on the traceability of food products (MMWR 60: 1357, 2011). The cantaloupe outbreak: NEJM 369: 944, 2013.
Erysipelothrix rhusiopathae causes erysipeloid, a spreading skin infection from handling meat or (especially) seafood. 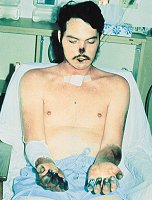 Plague needs no introduction.
Plague needs no introduction.Its history and transmission (from the rat via the flea) are famous. The etiologic agent is Yersinia pestis, which is widespread among animals in the Old World and our own West, where there are a few dozen cases of "sylvatic" ("woodland", i.e., acquired directly from animals) plague in humans yearly. Bubonic plague involves the lymph nodes draining the site of the flea bite. (The fleas typically just feasted on a rat that was dying of the disease.) The lymph nodes undergo necrosis, swell, and suppurate as the patient dies of sepsis. Pneumonic plague begins in the lungs and may be transmitted by droplet inhalation (usually the bloody cough of someone near death) with death resulting from a necrotizing pneumonia. The virulence factor that allows this is plasminogen activator (Science 315: 529, 2007). Septicemic plague has no localizing signs and kills in short order. Yersinia pestis is among the most virulent of all bacteria, with a plasminogen activator, a few different cytokine-inactivators, and even a toxin to make the flea throw up. Gerbils and plague in Kazakhstan: Science 304: 736, 2004. Update on plague: Lancet 369: 1196, 2007. It evolved a few thousand years before the plague of Justinian, from Y. pseudotuberculosis. * Great reading for the young doctor, even if you have no use for French existentialism: The Plague, by Albert Camus.
{12394} black plague!
Tularemia: 
Tula tula-remia,
Tula tula rye,
I've dressed six hundred bunnies,
I think I'm gonna die! -- Anonymous  Caused by Francisella tularenisis, a fastidious and dangerous (to the pathologist) microbe. Most cases come from handing sick rabbits ("Don't catch the slow bunnies"); the organism can enter through the skin ("even if unbroken", they say...), eye, mouth, or lungs. Don't worry about the subtypes; the histopathology is a mix of suppuration and granuloma formation (another "stellate microabscesses" disease), and the course is prolonged. Recovery with scarring is the rule.
Caused by Francisella tularenisis, a fastidious and dangerous (to the pathologist) microbe. Most cases come from handing sick rabbits ("Don't catch the slow bunnies"); the organism can enter through the skin ("even if unbroken", they say...), eye, mouth, or lungs. Don't worry about the subtypes; the histopathology is a mix of suppuration and granuloma formation (another "stellate microabscesses" disease), and the course is prolonged. Recovery with scarring is the rule.
{24488} tularemia ulcer (looks like pretty much any other acute infectious ulcer)
Pasteurella multocida infections are similar to tularemia. They usually follow dog or cat bites. Brucellosis, caught from infected goats, sheep, cattle, and dogs, is rare in the U.S. but a terrible cause of disease and chronic disability worldwide, notably in Mexico and anywhere that pasteurization isn't a strict rule. Brucella organisms are very hard to grow in the lab or to demonstrate in tissue (i.e., you will make this diagnosis serologically; sensitive but not specific). This is probably good, because the bug is dangerous to lab workers and pathologists (J. Clin. Path. 63: 90, 2010). Patients prevent with bacteremia and episodes of fever. Serology shows that many butchers and meat-workers have been infected. The infection may be acute or chronic, may involve a variety of organs (with a preference for the lymphoid tissue), produces a mix of abscesses and granulomas, and is very difficult to diagnose (especially if you do not think of it). Lymphocytes rather than neutrophils become elevated in the bloodstream. Death is very rare unless the heart becomes infected; the site is almost always the aortic valve. Brucellosis is quite catching when aerosolized and it was a component of U.S. bioweapons in the 1960's, but is seldom transmitted person-to-person. Update NEJM 352: 2325, 2005.
Glanders (caused by Burkholderia mallei, was Pseudomonas) primarily affects donkeys and horses in poorer nations. Humans contract an acute or chronic disease with mixed neutrophilic and granulomatous inflammation of mucosa, skin, and/or lungs. The bug is hard to kill with antibiotics, and can lurk for decades before becoming symptomatic. What's more, the bugs are few-and-far-between in lesions, and diagnosis is extremely easy to miss. * The first case of glanders contracted in the U.S. since 1945 happened as a result of a lab mishap: MMWR 49: 532, 2000).
Melioidosis (pseudoglanders, caused by Burkholderia pseudomallei, was Pseudomonas) is common in various mammals in Southeast Asia, and is now known to be transmissible from very contaminated drinking water (Am. J. Trop. Med. 65: 177, 2001). It has become symptomatic in Vietnam veterans up to years after their return (Hosp. Pract. 32: 219, 1997). Look for both abscesses and granulomas ("stellate microabscesses"). Both glanders and pseudoglanders are hard to treat. Leptospirosis, caused by the spirochete Leptospira interrogans carried by dogs and rats and spread by their urine (even in the alleyways of the United States: Ann. Int. Med. 125: 794, 1996; Britain Lancet 373: 978, 2009), or caught through fresh-water sports or whenever the water supply is fouled. Mild cases look like the 'flu with bad muscle aches, and/or a mild viral meningitis. An epidemic occurred as "Fort Bragg fever". Bad cases with aseptic meningitis, hepatitis, DIC, and/or renal tubular disease are called Weil's disease, rarely seen despite being "in the differential diagnosis of everything". Leptospirosis is a tough diagnosis to make. All about leptospirosis: Br. Med. J. 302: 128, 1991. Water-borne leptospirosis in Hawaii: Am. J. Pub. Health. 81: 1310, 1991. Brazil, Israel, Iran, Bangladesh all have well-established leptospirosis. Sri Lanka Am. J. Trop. Med. Hyg. 85: 572, 2011. The harder you look for it, the more you find -- it finally gets noticed in Tanzania Am. J. Trop. Med. Hug. 85: 275, 2011. Was leptospirosis the cause of the epidemic that decimated the American Indian tribes just before the Pilgrims settled? EID Journal Feb 2010.
Relapsing fever, caused by the spirochete Borrelia recurrentis and its kin, carried by ticks or lice from animal reservoirs. It produces a systemic mixed inflammatory response, and it recurs several times because of programmed genetic shifts in its antigens. These spirochetes are easy to see on peripheral smears, since they stain with Wright's stain. Rat bite fever covers two similar diseases, both with pain and infection at the site of the bite, followed by a fever and generalized rash.  Infection with Spirillum minus (sodoku) may last for a month or two. Streptobacillus moniliformis (Haverhill fever) is over quickly, but the arthritis can be troublesome.
Infection with Spirillum minus (sodoku) may last for a month or two. Streptobacillus moniliformis (Haverhill fever) is over quickly, but the arthritis can be troublesome.* Mama Rat caused the Haverhill outbreak by urinating into the milk jugs at the dairy.
Cat scratch disease (Hosp. Pract. 33(12): 37, Dec. 1998): Fever and localized lymphadenopathy (suppuration and granulomas, another "stellate microabscesses" disease) follow a cat scratch, and may persist for several months. The gram-negative rod that causes the infection was identified and named Afipia felis in the 1980's; the most common bug turns out to be Bartonella henselae (was Rochalimaea), which causes bacillary angiomatosis in AIDS (also contracted from cats, which can harbor the bug asymptomatically for years; Ann. Int. Med. 118: 388, 1993; Lancet 339: 1443, 1992; NEJM 329: 8, 1993; JAMA 271: 531, 1994). Even the literature still calls Afipia felis / Rochalimaea henselae "the cat scratch bacillus". Whether "Afipia" is a separate, rare bug still gets argued.The most troubling complication of this disease is an encephalopathy. See JAMA 259: 1347, 1988; Am. J. Dis. Child. 145: 98, 1989; Arch. Int. Med. 149: 1437, 1989; Lancet 340: 558, 1992. Antibiotic treatment usually isn't either necessary or effective; the one that works seems to be ciprofloxacin (JAMA 265: 1563, 1991). You'll make the diagnosis serologically (Western blot Am. J. Clin. Path. 108: 202, 1997). Thre is now a PCR that is more sensitive than serology for diagnosis (Am. J. Clin. Path. 115: 900, 2001).
The Whipple bacillus was first grown in the lab in 2000; it must be grown in human tissue cultures (NEJM 342: 620, 2000), and culture is still not routine. If there's any doubt, there's an immunostain (Am. J. Clin. Path. 118: 742, 2002) and a PCR (Am. J. Clin. Path. 116: 898, 2001; J. Inf. Dis. 183: 1229, 2001). It is phylogenetically closest to the actinomycetes (Lancet 338: 474, 1991; NEJM 327: 293, 1992). Its name is Tropherhyma whippelii (from trophe-, nourishment, and rhym-, barrier; Whipple's disease causes malabsorption).
Learning Objectives: The Other Bacteria Name the etiologic agent of syphilis and describe what we know about its pathogenesis and epidemiology. Describe its stages, and its congenital form, in detail. Recognize the disease clinically. Describe granuloma inguinale and chancroid, and recognize them clinically. Describe the epidemiology, etiology, pathogenesis, stages, symptoms and signs of tuberculosis
and describe what we know about its pathogenesis and epidemiology. Describe its stages, and its congenital form, in detail. Recognize the disease clinically. Describe granuloma inguinale and chancroid, and recognize them clinically. Describe the epidemiology, etiology, pathogenesis, stages, symptoms and signs of tuberculosis and leprosy
and leprosy , including their less familiar manifestations. Discuss the impact of AIDS and homelessness on TB
, including their less familiar manifestations. Discuss the impact of AIDS and homelessness on TB . Briefly describe major atypical mycobacterial infections. Describe the diseases produced by the pathogenic actinomyces family (nocardia
. Briefly describe major atypical mycobacterial infections. Describe the diseases produced by the pathogenic actinomyces family (nocardia and actinomycosis
and actinomycosis ) and the deep fungal pathogens. NOTE: For now, do not be concerned with the means of establishing these diagnoses clinically. Know the organisms and the diseases well.
) and the deep fungal pathogens. NOTE: For now, do not be concerned with the means of establishing these diagnoses clinically. Know the organisms and the diseases well.
SYPHILIS ("lues", "the great pox", "VD", etc., etc.)
{25239} spirochetes, testis, stained blue
{27989} spirochetes, optic nerve
{46491} spirochetes
{12445} primary syphilis, man
{12447} secondary syphilis, woman
 Syphilitic aneurysm
Syphilitic aneurysm
Classic patient photo
Adami & McCrae, 1914
 Syphilitic periostitis, skull
Syphilitic periostitis, skull
Classic photo
Adami & McCrae, 1914 A bad sexually transmitted disease caused by Treponema pallidum, a 10-13 micron spirochete. The treponemes are bacteria that produce chronic, generally non-fatal infections. They produce no injurious substances themselves, and the pathology is due to the body's reaction to their presence. They cannot be grown in vitro by present techniques. They do not stain with the usual stains, and silver techniques are required to visualize them in tissues. You can see the characteristic organisms on darkfield or using immunofluorescence. Spirochetes are extremely vulnerable to the environment (soap, drying, etc.), and are transmitted only by intimate personal contact. (NOTE: Syphilis is less infectious than gonorrhea, and much more infectious than AIDS. Only the primary and secondary stages are considered contagious, and even then, you need direct contact with the wet tissue) Syphilis probably came from the New World to Europe with Columbus (update Sci. Am. 298(3): 30, 2008), and the present endemic began soon afterwards. It's been suggested that Columbus may have brought back yaws, which because of the cooler climate and greater amount of clothing turned it to a sexually transmitted disease -- if this was true, the transformation was very fast. * O Rose, thou art sick,
The invisible worm
That flies through the night
In the howling storm Has found out thy bed
Of crimson joy,
And his dark, secret love
Doth thy life destroy.
Primary syphilis: One week to three months after meeting the spirochete, the patient develops a punched-out, painless, indurated ulcer (hard chancre) at the site of inoculation, followed by painless swelling of the regional nodes. This heals in a few weeks, and often goes unnoticed. The surface of the chancre contains plenty of infectious spirochetes. Wear gloves, and consider swabbing the lesion for a darkfield exam.
{12352} primary syphilis
{14265} primary syphilis
Microscopically, the lesion is obliterative endarteritis ("onionskinning", etc., i.e., the endothelium of the vessels proliferates and swells, causing infarction), and a dense perivascular infiltrate composed mostly of plasma cells. This is not really a biopsy disease. You will find plasma cells and maybe little granulomas in the regional nodes.
Secondary syphilis: Weeks to a few months after the chancre goes away, the patient usually develops a fleeting, variable rash over the skin and mucosal surfaces. Do not expect every patient to remember the rash. This is one of the few rashes that often affects the palms and soles -- others to remember are Rocky Mountain spotted fever , toxic shock syndrome, and Kawasaki disease. "Condylomata lata" ("flat venereal warts") are localized forms of the rash seen on the lips, genitals, and/or anal region. They are extremely infectious.
, toxic shock syndrome, and Kawasaki disease. "Condylomata lata" ("flat venereal warts") are localized forms of the rash seen on the lips, genitals, and/or anal region. They are extremely infectious.
{12282} secondary syphilis
{14268} secondary syphilis
{14271} secondary syphilis
{14275} secondary syphilis, condylomata lata
{25541} secondary syphilis
{25543} secondary syphilis
Again, the lesions teem with spirochetes, and (especially the weepy ones) are highly infections. Biopsy shows similar changes to a chancre. Virtually all patients will be seropositive, and will remain so until treated.
Tertiary syphilis: One of the most gruesome diseases of humankind, now fortunately rare. Involvement of the proximal aorta (compromise of the vasa vasora) causes aortic insufficiency and weakness of the aortic wall, which will dilate (i.e., form an aneurysm) and eventually rupture. Look for "tree barking" (longitudinal stretch marks) of the aortic intima. * Morgagni's "Seats and Causes of Disease", the first published autopsy series, includes an account of a CSW who died of a ruptured aortic aneurysm while providing CS. His medicolegal investigation absolved her client, who had run out of the building very upset, from the suspicion of murder.
{26603} syphilis of the aorta
 Tabes dorsalis, myelin stain
Tabes dorsalis, myelin stain
Dorsal columns at bottom
Classic drawing, Adami & McCrae, 1914
Neurosyphilis (which can supposedly occur "at any state", but we usually think of as being tertiary) takes four major forms: 1. General paresis ("general paralysis of the insane"), a dementing disease with hypomanic behavior and psychosis (loss of brain cells producing the "windswept cortex", etc.) General paralysis
Of the insane
Baffles analysis,
Treatment is vain.
Never more rallies his
System or brain. -- (early 20th century)
2. Meningovascular syphilis, fibrosis of the meninges, leading perhaps to headache or even hydrocephalus 3. Tabes dorsalis, a sensory syndrome (agonizing chronic pain, loss of proprioception) involving the dorsal columns of the spinal cord 4. Gummas, which mimic brain tumors clinically and radiologically Syphilis rarely causes stroke today (Stroke 20: 230, 1989).
Gummas are syphilitic granulomas with gummatous (basically the same as "coagulative") necrosis, and of course plenty of plasma cells. These are common in the liver and testes (where they cause little trouble, though the organs will be distorted, i.e., "hepar lobatum") and the sub-periosteum (where they cause severe chronic pain). Destruction of the bridge of the nose ("saddle nose") is also common. Involvement of other sites is rare. Although killing the organisms is easy, the organ damage will of course remain. * Other problems faced by the advanced luetic include glomerulonephritis, anergy, etc., etc. The (Jarisch-)Herxheimer reaction is type III immune injury precipitated following treatment by the release of antigens from dead spirochetes. Nowadays this may be a surprise after the patient receives antibiotics for something else (Am. J. Gastro. 94: 1694, 1999). Shockingly unethical studies done early in the 20th century in our own Old South demonstrated that a third of infected patients recover, a third remain seropositive without symptoms, and a third get some form of tertiary syphilis.
Congenital syphilis: infection of the unborn child. The most striking features of this awful disease are:
- "saber shins" and other bony deformities
- "mulberry molars", "Hutchinson's teeth", "screwdriver incisors", i.e., dental deformities
- gummas destroying the bridge of the nose and/or the hard palate
- pulmonary consolidation ("pneumonia alba", white pneumonia -- the term is also used for adult TB
 ; the tubercle bacilli disseminate through the airways)
; the tubercle bacilli disseminate through the airways)
- "hepar lobatum", enlargement and severe distortion of liver architecture due to gummas, and related splenomegaly
- rash resembling bad secondary syphilis, often with sloughing of skin on palms and soles
- mental retardation, nerve deafness, blindness, etc., etc.
- necrotizing inflammation of the umbilical cord ("necrotizing funisitis") has recently been re-recognized as virtually pathognomonic of syphilis (JAMA 261: 1788, 1989).
- any other sign of secondary or tertiary syphilis
At birth, the child's skin and secretions are highly infectious.
The spirochete does not cross the placenta until the fifth month of pregnancy, making prevention easy if the mother receives prenatal care. Of course, congenital syphilis is still a devastating problem in the poor nations (Arch. Dis. Child. 63: 1393, 1988) and the U.S. underclass (Am. J. Pub. Health. 81: 1316, 1991; Arch. Path. Lab. Med. 118: 44, 1994; * order silver stains on stillborns with big livers).
{25547} born with congenital syphilis
{53731} born with congenital syphilis, lacks nasal septum
{25548} born with congenital syphilis, gumma in palate
Despite a decline in the incidence of new syphilis cases when antibiotics came into use and contact tracing became routine, syphilis enjoyed a tremendous resurgence during the "free love" era thanks to "the pill" (which supplanted condoms until people wised up) and changing morals (Lancet 2: 166, 1989). Once again, it's declining, and is now primarily an underclass disease (J. Inf. Dis. 180: 1159, 1999). * You will learn how to make the serologic diagnosis of syphilis in "Microbiology". Syphilis PCR: J. Clin. Microb. 39: 1941, 2001. The classic screening tests depend on the fact that syphilitics make antibodies to beef heart (cardiolipin, Wassermann antigen, VDRL, etc.) There are many "biologic false positives", especially in patients with lupus, infectious mononucleosis, lupus anticoagulant, and other systemic diseases involving lymphocytes; * some "biologic false positives" are even attributed to pregnancy. Fluorescent tests, and the newer immunologic techniques, are more expensive but more specific, and are useful for confirmation of a positive screening test. In my opinion, it is malpractice not to follow up a positive RPR with one of the more specifci tests. Probably the only false-positives are in Lyme disease and a few lupus patients. After cure, the serologic tests usually revert to normal; it is difficult to tell a "serofast" patient from one who has been reinfected. Fortunately, syphilis is still easily treated with penicillin or other antibiotics.
and a few lupus patients. After cure, the serologic tests usually revert to normal; it is difficult to tell a "serofast" patient from one who has been reinfected. Fortunately, syphilis is still easily treated with penicillin or other antibiotics. * CNS syphilis requires more intensive therapy "because of the blood-brain barrier". It now appears that the spirochete invades the brain much earlier than we used to think, so some physicians recommend higher doses of antibiotics even for the early disease (Arch. Int. Med. 109: 849 & 855, 1988).
 In 1932, it was not at all clear whether the current treatments for syphilis (arsenic, bismuth, mercury, malaria
In 1932, it was not at all clear whether the current treatments for syphilis (arsenic, bismuth, mercury, malaria , etc.) weren't worse than the disease itself. To answer this question, the US Public Health Service began randomizing infected African-American men (mostly poor sharecroppers) in the Deep South to a treatment-vs.-no-treatment group, of course without informed consent. Around 600 men were eventually enrolled. They agreed to regular exams, to provide lab specimens, and to be autopsied in the end. In return they received a yearly cash payment and free burial expenses. By 1936, it was quite clear that the benefits of treatment outweighed the adverse effects (see JAMA 107: 856, 1936). For some reason, the study was continued, the controls were not treated unless they became symptomatic, and this state of affairs went on even after penicillin was discovered to be an easy cure (see NEJM 236: 243, 1947). The study and its methods were no secret, but not even the National Medical Association (which represents the African-American medical community) raised a word of protest. Probably the real purpose of this study was to help develop today's syphilis blood tests (J. Nat. Med. Assoc. 87: 56, 1995) using a group of known positives. The "Tuskegee Syphilis Experiment" ended, and the moral outrage from all quarters suddenly began, only in 1969 when one of the researchers, after being stonewalled for five years by institutionalized medicine, finally got an Associated Press reporter's attention. For a balanced summary of the whole business, see Lancet 1(7817): 1438, 1973; also NEJM 289: 730, 1973. The appalling facts speak for themselves, and for me bring back bad memories of the era, both of the Old South and of what today we call "medical paternalism". I take some comfort in noticing that there's been no similar fiasco in the US since the social changes of the early 1970's. Other treponematoses, caused by organisms that look identical to the syphilis
, etc.) weren't worse than the disease itself. To answer this question, the US Public Health Service began randomizing infected African-American men (mostly poor sharecroppers) in the Deep South to a treatment-vs.-no-treatment group, of course without informed consent. Around 600 men were eventually enrolled. They agreed to regular exams, to provide lab specimens, and to be autopsied in the end. In return they received a yearly cash payment and free burial expenses. By 1936, it was quite clear that the benefits of treatment outweighed the adverse effects (see JAMA 107: 856, 1936). For some reason, the study was continued, the controls were not treated unless they became symptomatic, and this state of affairs went on even after penicillin was discovered to be an easy cure (see NEJM 236: 243, 1947). The study and its methods were no secret, but not even the National Medical Association (which represents the African-American medical community) raised a word of protest. Probably the real purpose of this study was to help develop today's syphilis blood tests (J. Nat. Med. Assoc. 87: 56, 1995) using a group of known positives. The "Tuskegee Syphilis Experiment" ended, and the moral outrage from all quarters suddenly began, only in 1969 when one of the researchers, after being stonewalled for five years by institutionalized medicine, finally got an Associated Press reporter's attention. For a balanced summary of the whole business, see Lancet 1(7817): 1438, 1973; also NEJM 289: 730, 1973. The appalling facts speak for themselves, and for me bring back bad memories of the era, both of the Old South and of what today we call "medical paternalism". I take some comfort in noticing that there's been no similar fiasco in the US since the social changes of the early 1970's. Other treponematoses, caused by organisms that look identical to the syphilis spirochete, but which are not sexually transmitted
spirochete, but which are not sexually transmitted * Bejel: A chronic disease of desert communities, in which syphilis-like lesions begin on the mucosal surfaces Yaws: Lancet 381: 763, 2013. A once-dreaded jungle disease with skin ulcers. Bone involvement (gummas) is usual in the late stages. The disease is cured easily by penicillin, and the disease is now nearly extinct and could be eradicated with azithromycin (a single dose cures; NEJM 372: 693 & 703, 2015). The etiologic agent is Treponema pertenue.
{08199} yaws
{08200} yaws
* Pinta: A rural Latin American disease, which produces only skin disfigurement. The etiologic agent is Treponema carateum. Trench mouth and chronic gingivitis, familiar problems, now appear to be caused (at least in part) by micro-organisms in this category (NEJM 325: 539, 1991).
* Word buffs: Somebody has surely told you that the name syphilis is derived from the title character in a poem by an Italian Dr. Fracastorius. What you may not have heard is that the poem is all double-meanings, and that the character's name comes from Greek words sys (pig, cognates "sow", "swine", and "sooo-ey!") and philios (a word that can mean either "romantic love" or "just good friends".)
LYME DISEASE: The recently-discovered dread infection, acquired from ixodes ticks that have feasted on infected deer mice. Update Lancet
379: 461, 2012; NEJM
370: 1724, 2014.
Reforestation and a wholesome interest in outdoor activities have had the unfortunate effect of introducing humankind to this spirochetal zoonosis. Everybody knows by now that the micro-organism is acquired from a tick (Ixodes) bite. The tick gets it from little mammals (especially deer mice), in other settings from marine birds (really; Nature 362: 340, 1993). * The longer the tick stays attached, the more likely you are to get sick. If I found an engorged tick on me, I'd simply treat myself for Lyme disease (J. Inf. Dis. 175: 996, 1997)
Nobody talks about this, but the disease resembles syphilis both in its etiology and its pathology. The first complaint is likely to be a spreading, ring-like erythematous rash ("erythema migrans"), perhaps relapsing, around a site of a (remembered or forgotten) tick bite? This is primary Lyme disease, and the lesion is called erythema chronicum migrans. Of course, its spread represents the spread of the spirochete. Later, the spirochete can cause all manner of problems in the secondary and tertiary stages. The patient may have
both in its etiology and its pathology. The first complaint is likely to be a spreading, ring-like erythematous rash ("erythema migrans"), perhaps relapsing, around a site of a (remembered or forgotten) tick bite? This is primary Lyme disease, and the lesion is called erythema chronicum migrans. Of course, its spread represents the spread of the spirochete. Later, the spirochete can cause all manner of problems in the secondary and tertiary stages. The patient may have
- "arthritis";
- cranial nerve palsies (Lyme "flagellin" mimics an axon protein);
- non-suppurative meningitis;
- encephalitis;
- myocarditis;
- stillbirth?
Much of the havoc is mediated by immune response to the creature. Antibodies against its flagellum cross-react with an axonal protein, etc., etc. People who have a particular HLA molecule that matches the OspA outer surface protein are prone to an autoimmune arthritis (molecular mimicry) that does not remit after antibiotic treatment (Science 281: 703, 1998).
If you get tissue, the lesions will show inflammation with an infiltrate mostly of lymphocytes and (especially) plasma cells. Get a serology (lots of false negatives especially early: JAMA 282: 62, 1999); ask about a history of tick bite? Many cases of this currently-fashionable disease may not really be Lyme disease (i.e., diagnostic false positives) but who cares? Go ahead and treat patients you think might have it. The disease is treatable, yet is gruesome if untreated. See Science 260: 1579, 1993. Lyme disease vaccines: NEJM 339: 2090, 1998; these turned out not to be a great success.
EXOTIC BACTERIAL INFECTIONS that you might actually see in the clinic someday....
Rhinoscleroma: A chronic, slowly progressive disease of the upper airways caused by Klebsiella pneumoniae rhinoscleromatis. Review: South Med. J. 81: 1580, 1988. This potentially lethal disease is rare in the U.S., but common in Latin Americans and new immigrants from "south of the border", as well as Eastern Europe, and the Middle East. Since the disease presents as chronic rhinitis in young adults, it probably is under-diagnosed. Clinicians look for broadening of the nose ("Hebra's nose"); pathologists look for Mikulicz's foamy macrophages, which contain bacilli that require silver staining for good visualization. Today's therapy includes both long-term antibiotic therapy and laser surgery.
* Ozena: More common than rhinoscleroma, this chronic infection of the upper airway is due to Klebsiella ozaenae or mixed infections. Patients have "atrophic rhinitis". Granuloma inguinale (* "in the alley"): An uncommon, chronic sexually-transmitted disease caused by the intracellular pathogen Calymmatobacterium donovani. Symptomatic C. donovani infections is mostly a man's disease. Sores develop and spread on the penis and wherever it rubs ("kissing lesions"). If untreated, mutilation of the penis and groin results. The histology is a mixture of abscesses and granulomas. The organisms are easiest to see on Giemsa or silver stains ("Donovan bodies").
Chancroid ("soft chancre"): An uncommon, acute sexually-transmitted disease caused by Hemophilus ducreyi, which produces an ulcer similar to a syphilitic chancre, but without the induration. Poor personal hygiene seems to allow the infection to develop. If it get established, it spreads to regional nodes (which can turn into buboes), and to touching skin. Read all about it: Br. Med. J. 298: 64, 1989.
* Hemobartonellosis (Carrion's disease): Infection of erythrocytes by Bartonella bacilliformis. The major problem is a hemolytic anemia. Skin lesions may develop in untreated cases. The disease is limited to highlands of Peru, the habitat of its sandfly vector.
TUBERCULOSIS ("TB", "the white plague" -- covered twice in both "Big Robbins" and "R&F", and it deserves the attention). All about TB, especially for Clinicians: Lancet
362: 877, 2003.

I know the color of that blood; it is arterial blood; I cannot be deceived. That drop is my death-warrant. I must die.
* Keats's era believed that red, fresh blood was arterial, and dark, altered blood was venous.
|
Tuberculosis remains one of the world's major diseases and is presently resurgent (thanks to AIDS, homelessness, lack of access to health care, the "right" to be noncompliant with therapy, and sheer I-don't-care) in the U.S. (Postgrad. Med. 84(1): 58, July 1988; Arch. Int. Med. 148: 1843, 1988; Am. Rev. Resp. Dis. 141: 1236, 1990; Am. Rev. Resp. Dis. 143: 257 & 717, 1991; Nature 356: 473, 1992) and Third World (Lancet 338: 557, 1991; JAMA 273: 220, 1995). Catching TB at the crack house: NEJM 364: 730, 2011. The etiologic agents are Mycobacterium tuberculosis ("M. tuberculosis hominis"), historically spread by coughing, and Mycobacterium bovis ("M. tuberculosis bovis"), historically spread through cow's milk. They are waxy mycobacteria that are hard to kill with disinfectants and survive drying. (Ultraviolet light supposedly kills them more effectively.) They also grow slowly, so it will probably take your "TB culture" several weeks to turn up positive even in fulminant disease. Invisible on standard microscopic slides, both bacilli are respectfully called "red snappers" because of their characteristic staining by the Ziehl-Neelsen acid-fast technique. (However, they are usually scarce in sputums and in tissue sections; most pathologists prefer to do acid-fast stains using the non-specific fluorescent dye auramine O, and a culture's still the most sensitive and specific, albeit slowest, way to make the diagnosis.)
{13809} red snappers
Many, if not most, people living in today's world have met the TB bacillus, but most never become sick. You know that the tuberculin ("Mantoux") skin test turns positive in any normal person whose T-cells have met the tubercle bacillus. Many TB bacilli are killed when cell mediated immunity and caseous necrosis begin, but there are usually survivors, and the bacterium can live indefinitely in the caseous necrosis
necrosis begin, but there are usually survivors, and the bacterium can live indefinitely in the caseous necrosis inside the tiny granulomas that result from primary infection with the organism. Any person who tests tuberculin positive presumably has at least one such granuloma in his or her body, and therefore is at risk for developing the active disease. For a review of what we know about the pathogenesis of tuberculosis, see Antimicrob. Agents Chemother. 47: 833, 2003. One reason the lesions tend to be firm ("like cheese") is that the fibers of the organ are spared, the cells themselves being killed by cell-mediated immunity rather than neutrophils.
inside the tiny granulomas that result from primary infection with the organism. Any person who tests tuberculin positive presumably has at least one such granuloma in his or her body, and therefore is at risk for developing the active disease. For a review of what we know about the pathogenesis of tuberculosis, see Antimicrob. Agents Chemother. 47: 833, 2003. One reason the lesions tend to be firm ("like cheese") is that the fibers of the organ are spared, the cells themselves being killed by cell-mediated immunity rather than neutrophils.
Tuberculosis remains primarily a disease of poverty, crowding, malnutrition, and lack of health care. Blacks (American, African; see Ann. Int. Med. 116: 896, 1992) and American Indians (including Eskimos) are much more susceptible than whites. This is probably due to natural selection for resistance among Europeans. * The first identified gene for susceptibility: JAMA 279: 226, 1998.We are just now studying the neutrophil response to TB; there are two proteins that enable neutrophils to fight TB, and Afro-Europeans have less of these than white Europeans or Asian-Europeans (J. Clin. Inv. 117: 1988, 2007).
Immunosuppression from any cause predisposes to TB infection. Remember especially alcoholism, Hodgkin's disease, and immunosuppressive treatment with glucocorticoids. Most striking of all is probably the extremely high rate of active TB in silicotics. Diabetics and renal failure patients are also at some extra risk, and clinical folklore also lists previous gastrectomy for some reason -- I doubt this. Tuberculosis used to be the major occupational hazard of physicians, and up to 20% of medical students would need to go on leave to be treated. Certain situations predispose to catching TB, including being a mine worker (Am. J. Pub. Health. 101: 524, 2011) and hanging out in the crack house (NEJM 364: 730, 2011). It's still fairly commmon among America's homeless: Am. J. Pub. Health. 101: 546, 2011). World-wide, around 1.7 million people die of TB every year, or 1.3 if you don't count AIDS patients (WHO, 2011), down from three million in 1990. Every one of these people could be saved if we could get modern treatment to them, and get them to take it. The scandal of TB in South Africa: Lancet 335: 1126, 1990.
TB bacilli love oxygen and prefer to grow where it is most abundant (i.e., at the apical and subapical regions of the lungs). M. bovis infections, acquired through drinking infected milk, usually start in the tonsils or Peyer's patches.
How does the TB bacillus make a person sick? The answer continues to elude medical science. The organism produces no endotoxin, exotoxin, or histolytic enzyme. But the lipid factors that are required for virulence (* wax D, * muramyl dipeptide) are also potent stimuli for cell-mediated immunity. * Cord factor, another virulence factor, prevents fusion of lysosomes and phagosomes in macrophages, allowing the devoured bacillus to grow undisturbed. Tissue damage seems to start at around 2-4 weeks after exposure to the bacillus (when the tuberculin skin test also turns positive). Granulomas form around the bacilli, and these usually develop central caseation . (TB granulomas are called tubercles, and if they are caseating in the center, soft tubercles). Both Langhans ("classic TB") and foreign-body giant cells are common. Whatever the chemistry and cell physiology may be, the body's reaction to the hated tubercle bacillus probably does most of the damage. Caseation
. (TB granulomas are called tubercles, and if they are caseating in the center, soft tubercles). Both Langhans ("classic TB") and foreign-body giant cells are common. Whatever the chemistry and cell physiology may be, the body's reaction to the hated tubercle bacillus probably does most of the damage. Caseation is evidence of some immunity; AIDS patients often have confluent granulomas with no "soft center".
is evidence of some immunity; AIDS patients often have confluent granulomas with no "soft center".
For the patterns of tuberculosis in the lungs, see the respiratory section of these notes. Miliary TB most heavily involves the adrenals, bone marrow, endometrium, epididymis, fallopian tubes, liver, meninges, prostate, and spleen.
{11012} miliary TB in the lung
{11015} miliary TB in the lung
{21147} miliary TB
{21148} miliary TB
{32807} TB meningitis (worst around the circle of Willis)
Progressive isolated organ TB most often involves:
- adrenals
- cervical lymph nodes
- fallopian tube
- epididymis
- kidney
- meninges around the base of the brain
- vertebral marrow Pott's disease -- collapses the spine; look for "psoas abscesses" that drain through groin; Pott's today: Chest 95: 598, 1989.
 Patients with secondary TB typically have the slow onset of fatiguability, malaise, fever (* check in the afternoon), weight loss, and night sweats.
Patients with secondary TB typically have the slow onset of fatiguability, malaise, fever (* check in the afternoon), weight loss, and night sweats. When the larger airways are involved, cough and hemoptysis occur. TB in other organs can be confused with many other diseases. Miliary TB is often subtle. Death results from pulmonary TB from exsanguinating hemoptysis or asphyxiation.
In the U.S., we monitor TB by skin testing, with recent converters sometimes treated (this is going out of fashion in many places today). PITFALL: The most severe TB cases, and many immunosuppressed patients, have cutaneous anergy. Unless you have ruled out anergy (how do you do that?), your very sick patient's negative skin test proves nothing. We still need to culture the organism to be certain of the diagnosis. TB infections can be (and are) controlled as needed using antibiotics, except in moribund patients (Thorax 43: 591, 1988). The real challenge is making the diagnosis. BCG ("bacille Calmette-Guérin") vaccine is given in the Third World to produce the same immunity as does a primary infection. If the patient later meets the TB bacillus, the body will be ready to wall off the intruders immediately. * It protects kids, but is probably worthless in protecting adults (J. Inf. Dis. 207: 1115, 2013). * Some U.S. physicians insist on treating people who have positive tuberculin skin tests because of previous BCG vaccination overseas. It's common to be positive because of this Am. Rev. Resp. Dis. 146: 752, 1992. The prevailing wisdom is that a positive from BCG alone reverts to negative after 5 years. I don't know why people assume this is the norm. Ask your infectious disease expert. BCG is occasionally reconsidered as an option for house staff physicians where TB is a major problem (Am. Rev. Resp. Dis. 143: 490, 1991, stay tuned for more). * Especially in the era of neonatal HIV infection, in countries where babies receive BCG at birth, it's important to determine at once whether a mycobacerial infection is caused by tuberculosis itself or by BCG. Thankfully, new PCR techniques can do this quickly (J. Clin. Micro. 46: 2241, 2008). * BCG is an important treatment for early bladder cancer.
TB is much more common in the U.S. than it was in 1970's. There are 22,000 new active TB cases found in the U.S. each year (Postgrad. Med. 84(1): 58, July 1988). Watch for M. bovis infections among food faddists who oppose the pasteurization of milk -- it is only a matter of time until there is an outbreak. Wild animals can transmit M. bovis to dairy herds: Lancet 338: 1243, 1991. M. bovis is back as an AIDS opportunist, mostly in Mexican immigrants: Medicine 72: 11, 1993. Remember that TB is a major underlying cause of amyloidosis A. Drug-resistant TB emerges: Science 255: 148, 1992; Nature 358: 538, 1992. At the time, "multiple drug resistant TB" was defined (and still is) to be resistant to isoniazid and rifampin. We now have XDR-TB (extremely drug resistant TB), which emerged from South Africa and is spreading (NEJM 356: 656, 2007; ). * A patient with infectious multi-drug-resistant tuberculosis exercises her "right" to travel on the airlines and cough all over her fellow-passengers, infecting six of them (NEJM 334: 933, 1996).
Both classic TB and TB of the lymph nodes (the latter is common in children) are now treated with short chemotherapy (Br. Med. J. 301: 359, 1990; Am. Rev. Resp. Dis. 143: 697, 700 & 707, 1991). * "How much money is your health worth?" The U.S., where poor schoolkids still can't get eyeglasses, talked in the 1990's about requiring space-suits for health-care workers so they won't catch TB. The cost would be between $7 million and $18 million to prevent one case. See Ann. Int. Med. 121: 37, 1994; NEJM 331: 169, 1994.
ATYPICAL MYCOBACTERIAL INFECTIONS
Close kin to the familiar "red snappers" are a host of "atypical mycobacteria" that cause hard-to-treat infections that seem to strike at random. Worth recognizing: Mycobacterium kansasii, M. intracellulare, and M. avium. Vicious lung infections. Some hosts are immunocompromised (especially COPD cases; the latter two are notable AIDS pathogens), while others have no apparent reason for being susceptible. Atypical mycobacterial infections may occur in people with normal immune systems, in which they usually behave like TB but slower ("granulomatous atypical mycobacterial infection"). In the immunocompromised, it's often "progressive systemic" disease involving many systems, with the bacteria living within the abundant macrophages with little tissue reaction. * Hot-tub MAI: Chest 111: 242, 1997. Beware.* Kansasii in AIDS: Arch. Path. Lab. Med. 127: 554, 2003.
 Atypical mycobacteria
Atypical mycobacteria
Lung pathology series
Dr. Warnock's Collection M. scrofulae: causes cervical adenitis, "scrofula", "the King's evil" (* Shakespeare's Macbeth  ), etc. (TB bacilli can cause the same thing.) * M. ulcerans and M. marinum cause non-healing ulcers. The former is an "emerging infectious disease", especially in the poor nations. Neither are caught person-to-person. The former was finally discovered to have its hiding-place in a water insect (Science 319: 1747, 2008). The latter grows in home fish-tanks. * M. fortuitum and M. chelonei cause deep skin abscesses. * There's a hereditary problem in which patients are extremely susceptible to atypical mycobacteria. The problem seems to be inability to make α-TNF appropriately: Lancet 345: 79, 1995.
), etc. (TB bacilli can cause the same thing.) * M. ulcerans and M. marinum cause non-healing ulcers. The former is an "emerging infectious disease", especially in the poor nations. Neither are caught person-to-person. The former was finally discovered to have its hiding-place in a water insect (Science 319: 1747, 2008). The latter grows in home fish-tanks. * M. fortuitum and M. chelonei cause deep skin abscesses. * There's a hereditary problem in which patients are extremely susceptible to atypical mycobacteria. The problem seems to be inability to make α-TNF appropriately: Lancet 345: 79, 1995.
LEPROSY ("Hansen's disease"; Lancet
345: 697, 1995; Lancet
353: 655, 1999; Lancet
363: 1209, 2004)
 www.leprosy.org
www.leprosy.org
Some good photos
A dread, chronic, poorly-transmissible disease, caused by Mycobacterium leprae. Big Robbins' estimate of 10 million cases worldwide is low. M. leprae (lepra bacillus) is an acid-fast (* Fite stain's best) rod that grows only within host cells (not in the lab, i.e., you are going to make this diagnosis clinically or on biopsy). Antibodies are useless against the micro-organism (and you can't order a "leprosy serology"), but cell-mediated immunity keeps the organism at bay in most people who meet it. * Trivia: The only other animal affected in nature is the nine-banded armadillo. The "lepromin" skin test (analogous to the tuberculin) is positive at 24 hours (Fernandez reaction) and once again at 3-4 weeks (Mitsuda reaction). In tuberculoid leprosy, there is a brisk cell-mediated immune response to the organism, have a positive 48 hour lepromin skin test, and end up with some good granulomas and only a few leprosy bacilli. (You won't see as many granulomas as in TB , and they won't be as sharp.) In lepromatous leprosy, cell-mediated immunity is inadequate, and the lepromin test is negative. The deficient response may be specific for leprosy (i.e., there is tolerance), or a reflection of generalized failure of cell-mediated immunity (i.e., anergy, at least to the leprosy bacillus, perhaps the result of longstanding leprosy).
, and they won't be as sharp.) In lepromatous leprosy, cell-mediated immunity is inadequate, and the lepromin test is negative. The deficient response may be specific for leprosy (i.e., there is tolerance), or a reflection of generalized failure of cell-mediated immunity (i.e., anergy, at least to the leprosy bacillus, perhaps the result of longstanding leprosy). A patient with tuberculoid leprosy who eventually becomes anergic because of the infection will transform to lepromatous leprosy.
The tendency nowadays is to classify leprosy not by immune response, but by bacterial load (that's what you're treating, doctor). We distinguish paucibacillary and multibacillary leprosy.
The lepra bacillus grows only in the cooler parts of the body, i.e., the skin and cutaneous nerves (J. Path. 157: 15, 1989), upper airways, testes, hands and feet. * Leprosy is a spectacular example of degenerate evolution. A quarter of its DNA is pseudogenes that have counterparts as functional genes in TB bacilli (Nature 409: 1007, 2001); it no longer needs to use these since it has adopted a new lifestyle -- less catching but more protected.
bacilli (Nature 409: 1007, 2001); it no longer needs to use these since it has adopted a new lifestyle -- less catching but more protected.
Tuberculoid leprosy patients often have a few good granulomas, and they may contact the epidermis. You will see more macrophages, though, in lepromatous leprosy. Look for depigmentation. There is more damage to the peripheral nerves than in lepromatous leprosy, this is largely irreversible, and this causes most of the problems. T-cells seem to destroy bacterial-infected schwann cells; the mechanisms are just becoming clear (J. Imm. 166: 5883, 2001).Pain sense and the ability to sweat tend to be lost first. "Trauma to the anesthetic parts of the body" is blamed for the loss of these parts; this pathologist seriously questions this, preferring to believe that the same mechanism that destroys the nerves locally also causes poor wound healing. The numb areas do tend to be the ones where there are non-healing ulcers. This all remains quite a baffling business, since the actual skin reactivity seems to be unaffected.
Lepromatous leprosy patients have masses of histiocytes that do not form good granulomas (why not?). Pathologists describe "lepra cells" (foamy-looking macrophages packed with lepra bacilli) and "globi" (masses of bacilli). The severe disfigurement ("leonine facies") and tissue damage due to these masses.
{05975} lepromatous leprosy, lepra foam cells
{05978} lepromatous leprosy, acid-fast stain showing bugs
{12393} leprosy, hands
{13343} leprosy, lepromatous (leonine facies)
* For some reason, the masses of foamy macrophages never grow quite to the epidermis ("free" or "grenz" zone). In the tuberculoid form, however, granulomas can and often do touch the epidermis -- look for depigmentation. * Erythema nodosum leprosum is a serious type III immune injury syndrome that occurs acutely in the subcutis of leprosy patients. The treatment of choice is thalidomide, the famous teratogen, that also suppresses production of TNF-α and modulates other interleukins. * The re-introduction of thalidomide into clinical medicine in the late 1980's sparked political furors, bans, and so forth "because it might be given to a pregnant leper", etc., etc. (Lancet 343: 432, 1994). The militants in the U.S. held the drug up in the US until 1997, at least ten years after the benefits were obvious (Br. Med. J. 315: 699, 1997). I think this was merely an attempt to make political capital at the expense of sick people in genuine need. Of course, there is no such outcry over Accutane or methotrexate, medicines that the activists might actually need for themselves. Thankfully the shouting seems to be over, and thalidomide is now a mainstay of therapy for leprosy, myeloma, AIDS wasting, and graft-vs-host disease; and I predict it will find use in the management of Crohn's and rheumatoid arthritis.
* Arthritis seems to be common in leprosy and resembles rheumatoid arthritis (Br. Med. J. 298: 1423, 1989).
Leprosy is very weakly transmissible (by sneezes), and in almost all cases there has been extensive contact with a victim of lepromatous leprosy during childhood. However, its victims (and imagined victims) have inspired fear and loathing, and do so to this day (i.e., children's sick jokes). Drug treatment is effective but takes several years to work, and there are political and economic obstacles to its widespread use. * Minocycline (!) for leprosy: Br. Med. J. 304: 91, 1992. * Curiously, we lack reports of AIDS exacerbating leprosy (Br. Med. J. 298: 364, 1989). * A single dose of rifampin following massive exposure to leprosy prevents the disease: BMJ 336: 761, 2008.A vaccine is in 3rd-stage clinical trials; of course BCG also gives some protection. * Forensic anthropologists have found the remains of many lepers, and much of medieval and early-modern medicine deals with the subject. No one knows exactly why leprosy waxed and waned so dramatically in various communities; it would vanish inexplicably for centuries in an area, then come back brutally. The most likely explanation seems to me to be the protective effect of bovine TB (Lancet 369: 808, 2007).
Remember that leprosy is a major underlying cause of amyloidosis A. Maybe 30% of lepers eventually succumb to amyloidosis.
NOCARDIOSIS
Infection with "Nocardia", a low-virulence, filamentous, gram-positive, weakly acid-fast bacterium. Immunosuppressed patients develop lung infections with Nocardia asteroides. The usual histology is multiple lung abscesses without granulomas. The infection is probably missed much of the time, since the organisms are invisible both on H&E and on "routine acid fast stains". "Immunologically normal" people can develop Nocardia brasiliensis skin infections ("mycetomas", a generic name for hard-to-treat, nodular "fungal" skin infections, especially common on the feet in countries where shoes are a luxury). The problem is common in Latin America but rare in the U.S. Today, Nocardia is being cultured from central venous catheters, on which it is able to form a biofilm.
ACTINOMYCOSIS
Chronic fibrosing, pus-producing infections due to an anaerobic "Actinomyces" bacterium, usually Actinomyces israelii. Actinomyces are normal commensal organisms in the tonsils and in tooth crud. They can only infect necrotic tissue, i.e., they overgrow after surgery or in a pre-existing abscess.
The classic form is "lumpy jaw" (cervicofacial actinomycosis), with running sores in the mouth, and on the face and neck. Or the peritoneal cavity may become involved after rupture of the gut ("abdominal actinomycosis"). Or lung abscesses may be the problem ("thoracic actinomycosis", especially in those with rotten teeth). Actinomycosis of other sites follows bites or punch injuries (Arch. Int. Med. 148: 2668, 1988). Systemic actinomycosis is rare but does occur (Infection 17: 154, 1989). Pelvic actinomycosis was a complication of the old-fashioned intra-uterine devices (NEJM 323: 183, 1990).
Smears of actinomycosis pus show naked-eye "sulfur granules" (large yellow actinomyces colonies). The radially-oriented bacteria at their edges earned the actinomyces the unfortunate name "ray fungi".
{06115} actinomyces colony
{10904} endometrial actinomycosis
NOTE: Nocardia and actinomyces
and actinomyces are bacteria. They are "fungi" in the same sense that whales are fish, i.e., they are not, but are often discussed as if they were.
are bacteria. They are "fungi" in the same sense that whales are fish, i.e., they are not, but are often discussed as if they were.
CANDIDIASIS ("moniliasis", "yeast infection")
Now, instead of saying to patients that they have sacroiliitis, I tell them that they are allergic to candida. -- Kevin Barraclough MD, "Bullshitting", BMJ 327: 171, 2003
The most common serious human fungal disease. Candida albicans is the usual agent. You are familiar with the pseudohyphae, from which bud off small yeasts. Candida albicans is a normal commensal, which overgrows when the normal flora are killed by antibiotics, or when there is lots of glucose around (i.e., in diabetes, in the vagina during pregnancy or when "on the pill") or when patients are immunocompromised. It's also one of the causes of the annoying "nail fungus". * Other candida organisms include Candida tropicalis, and the never-trivial Candida glabrata ("torulopsis").
Candidiasis on the mucosal surfaces (mouth, vagina) appears as white patches ("thrush"). You can scrape them off and confirm the diagnosis microscopically. Patients are usually normal folk who have had overgrowth for some reason. Candida also causes infection of wet skin (groin, between toes, "jungle rot"; sports docs: distinguish candida "jock rot" from more banal fungi by the presence of "satellite lesions"). * Candidiasis of the esophagus usually means serious immune compromise.
Immunocompromised patients are prone to candida infections of any organ. Set-ups include patients who already have thrush, or preemies, or people with indwelling lines (venous catheters, peritoneal dialysis).
{00416} candida in urine
{05283} thrush
{27362} candida yeast and pseudohyphae
* Occult systemic candidiasis is still a fad diagnosis in many circles ("The Yeast Connection", etc.), where it is considered the cause of most, if not all, physical and emotional problems. If this is true, it has resisted every attempt to demonstrate it objectively: NEJM 323: 1766, 1991.
 Candida
Candida
Male patient photos
Health Awareness Connection

MUCORMYCOSIS ("mucor", "zygomycosis", "phycomycosis")
Infection by such bread molds as Rhizopus. The spores germinate best at low pH, and the hyphae then invade vessels. Typical victims are ketoacidosis patients, the extremely immunosuppressed, and the most un-hygienic of IV drug addicts (NEJM 323: 1923, 1990). Because the spores most often land in the nose, the head and face are most often involved. Necrosis of tissue perpetuates the process. Look for wide hyphae with wide-angle branching, invading blood vessels. The prognosis is poor, since patients are already very sick, the bugs are hard to kill, and the involved tissue is underperfused and already dead or dying. * Future pathologists: Heads up. Methenamine silver isn't as good for spotting mucor as PAS; this is the reverse of the other nasty fungi.
{06091} mucormycosis (good ninety-degree angle branching)
* Traditional teaching is that Candida is the only fungus that does not typically enter the body via a primary infection in the lungs. Supposedly even a North or South American blasto skin infection got there by way of the lungs. I believe this is bunk. I've been unable to find any person or source that can explain the traditional belief.
ASPERGILLOSIS
Invasive fungus infection, usually by Aspergillus fumigatus or niger, the familiar, ubiquitous fungi with septate, narrow-angle branching hyphae and characteristic fruiting bodies (* which resemble a holy water sprinkler used by some denominations -- "aspergillum"). More pathogenic than mucor, it also invades blood vessels. "Big Robbins" describes "colonizing aspergillus (aspergilloma)" as if it were a wad of harmless fungus growing in an old TB cavity. Since these lungs often have no other evidence of previous TB, and since these patients do cough up blood, it seems more likely that the fungus has invaded a blood vessel, then colonized the ischemic tissue. Everyone believes in invasive aspergillosis, a common, life-threatening, hard-to-diagnose infection among the immunosuppressed.
cavity. Since these lungs often have no other evidence of previous TB, and since these patients do cough up blood, it seems more likely that the fungus has invaded a blood vessel, then colonized the ischemic tissue. Everyone believes in invasive aspergillosis, a common, life-threatening, hard-to-diagnose infection among the immunosuppressed. There are several different tissue reactions, depending on how immunocompromised the patient is. Macrophages tend to attack the spores, while neutrophils attack the hyphae (Am. J. Clin. Path. 127: 349, 2007).
* Is nothing safe? Aspergillus and other horrid fungi from taking a shower Cin. Inf. Dis. 35: E86, 2002. Does make sense. Also fusariosis Clin. Inf. Dis. 33: 1871, 2001.
{00413} aspergillus, brain
{06077} aspergillus, brain
{06085} aspergillus, vessel; silver stain
{10670} aspergillosis, lung
{10673} aspergillosis, lung
{11018} aspergillosis, lung; silver stain
{37661} aspergillosis, brain
People also get allergic to aspergillus, i.e., to airborne spores, which can produce type I (asthma), type III (organic pneumoconiosis), and/or type IV (more organic pneumoconiosis) immune injury. Of course, people can and do become allergic to their own infectious agents, and people who already have fungus balls tend to become allergic to them. And aspergillus commonly infects people who already have allergic asthma. Both are called allergic aspergillosis (Postgrad. Med. J. 64 Supp. 4: 96, 1988).
* Aspergillus flavus produces aflatoxin, the famous carcinogen.
 Aspergilloma
Aspergilloma
Lung pathology series; follow the arrows
Dr. Warnock's Collection
 Hyphal fungi and candida
Hyphal fungi and candida
Lung pathology series
Dr. Warnock's Collection 
CRYPTOCOCCOSIS ("crypto")
An opportunistic fungal infection by a yeast that abounds in pigeon droppings. The yeast has a huge, gooey polysaccharide capsule (the basis for the India Ink test), and it reproduces by narrow-based budding.
The most common site of infection is the meninges, and the underlying cerebral cortex may be infected via the Virchow-Robin spaces and turned into swiss cheese. Order a latex agglutination test on spinal fluid if you even vaguely suspect cryptococcosis. Any other organ can be involved as well (* "crypto" of the prostate: Ann. Int. Med. 111: 125, 1989).
In the immunosuppressed patient, there is usually no inflammatory reaction, and the disease comes on slowly.

BLASTOMYCOSIS ("blasto", "North American blasto", "Chicago disease"): JAMA
261: 3159, 1989; Lancet
1: 25, 1989 (still good); South. Med. J.
92: 289, 1999.
Infection by Blastomyces dermatitidis, a yeast found primarily in the Mississippi River valley, especially on riverbanks. Recognize these yeasts by their large size, thick walls and single, broad-based buds. One good way to catch the bug is to mess around in a beaver dam. Subclinical infection is now known to be common, though not nearly so common as histoplasmosis (Am. J. Med. 89: 470, 1990). The host response is generally a mix of suppuration and loose granuloma formation. Skin infections (for some reason considered to be "always secondary to lung infection") feature a chronic dermatitis, with overgrowth of the epidermis ("pseudoepitheliomatous hyperplasia") that will almost always be mistaken clinically for cancer.
(Am. J. Med. 89: 470, 1990). The host response is generally a mix of suppuration and loose granuloma formation. Skin infections (for some reason considered to be "always secondary to lung infection") feature a chronic dermatitis, with overgrowth of the epidermis ("pseudoepitheliomatous hyperplasia") that will almost always be mistaken clinically for cancer.
Making the diagnosis is tricky. Culture will take about 5 weeks, so cytology (brushings, washings) plus serology are probably in order whenever you are trying to diagnose "pneumonia" or "lung cancer" (Chest 121: 768, 2002). "Blasto" is a primary infection, and not much seen in immunocompromised patients; it is now turning up as a pathogen in AIDS. It responds poorly to anti-fungal drugs, though some infections have been successfully treated. * It is a common cause of death in pet dogs. * Its known virulence factor (BAD1) causes macrophages to pump out lots of TGF-β and thus suppress their own production of TNF-α: J. Immunol. 168: 5746, 2002).
{00443} blastomycosis in tissue
{10667} blastomycosis in the lung (my case)
{00460} blastomycosis in AIDS patient (fungus is black)
 Histoplasmosis
Histoplasmosis and blastomycosis
and blastomycosis
Lung pathology series
Dr. Warnock's Collection 
PARACOCCIDIOMYCOSIS ("South American blastomycosis")
A fungal infection caused by a huge yeast, Paracoccidioides brasiliensis, that produces many spores at the same time ("multiple buds", "mariner's wheel").
{24491} South American "blastomycosis" of the face
Most victims are male agricultural workers, especially in the Amazon basin. The victim usually has picked his teeth with a piece of jungle wood. (The common claim, repeated in "Big Robbins", that oral lesions have spread from the lungs seems silly to this pathologist.) The mouth, and sometimes the lungs, are the usual sites of involvement. * Women during child-bearing years are immune, since estrogens turn the yeast into a non-pathogenic hyphal form.

COCCIDIOIDOMYCOSIS ("San Joaquin Valley fever") NEJM
332: 1077, 1995
Infection by Coccidioides immitis, an organism fortunately confined to parts of the U.S. southwest. The fungus appears in tissue as a large spherule, often filled with endospores. Most famous for occurring in the San Joaquin valley of central California, a variant strain is very abundant in the Phoenix-Tucson area of Arizona.
The infection most often takes the form of a severe chest cold with joint pains, but it proves lethal in some cases. Blacks and especially Filipinos are especially susceptible to this infection, and this was a major killer of army recruits early in the 20th century. Navy SEALs: J. Inf. Dis. 186: 865, 2002. Of course, other immunosuppressed patients are at extra risk.
{24221} coccidioidomycosis
{24224} coccidioidomycosis
HISTOPLASMOSIS ("histo")
Infection by Histoplasma capsulatum, a tiny non-encapsulated (i.e., misnamed) yeast. The organism is found primarily in the U.S., in the Mississippi River valley, and it is ubiquitous in Kansas City. The organism is inhaled from bird (especially starling) or bat guano (caves are full of it: JAMA 260: 2510, 1988), or from soil where these have been deposited. Only the spores produced by the mycelium are contagious (i.e., you cannot possibly catch "histo" from a patient).
{10364} histoplasmosis in macrophages
{06065} histoplasmosis
{06068} histoplasmosis
When most people meet the histoplasma fungus, they develop only a mild fever and chest cold. If the person goes to the doctor and gets a diagnosis, it is primary pulmonary histoplasmosis. Latent histoplasmosis is the residue of an old, healed infection. Tiny calcified granulomas are found in the lungs, and often in the spleen and even the liver. If you really looked, you'd probably find tiny, old histoplasmosis lesions in a majority of autopsies in Kansas City. They may or may not contain stainable or viable histoplasma. Chronic pulmonary histoplasmosis is a cavitating, granulomatous disease of the lungs, while disseminated histoplasmosis kills the immunosuppressed and those who, for some reason, cannot mount an immune response. The diagnosis is generally a surprise at autopsy. "Histo" in AIDS: Am. J. Med. 86: 141, 1989. Single organ histoplasmosis has been reported for many locations, notably the adrenal glands (Ann. Int. Med. 110: 87, 1989). A "histoplasmoma" is a calcified histoplasmosis granuloma, while "sclerosing mediastinitis" is the result of serious histoplasmosis in the chest. The similarity to TB should be obvious, and the pathogenesis ("histo" produces no tissue toxin but is hated by the T-cells -- Am. Rev. Resp. Dis. 138: 578, 1988), gross pathology, and clinical pictures are virtually identical. Histoplasmosis in AIDS: J. Inf. Dis. 158: 623, 1988. Histoplasmosis endocarditis: South. Med. J. 100: 208, 2007. Today, there's a urine test for histoplasmosis antigen that works reasonably well (Am. J. Clin. Path. 128: 18, 2007.) * Trivia: African histoplasmosis is caused by Histoplasma dubosii.
should be obvious, and the pathogenesis ("histo" produces no tissue toxin but is hated by the T-cells -- Am. Rev. Resp. Dis. 138: 578, 1988), gross pathology, and clinical pictures are virtually identical. Histoplasmosis in AIDS: J. Inf. Dis. 158: 623, 1988. Histoplasmosis endocarditis: South. Med. J. 100: 208, 2007. Today, there's a urine test for histoplasmosis antigen that works reasonably well (Am. J. Clin. Path. 128: 18, 2007.) * Trivia: African histoplasmosis is caused by Histoplasma dubosii.
OTHER DEEP FUNGI
Mycetomas ("Madura foot", "maduromycosis") is a deep infection of the skin and subcutaneous tissues, usually of the foot. In addition to the bacterium Nocardia brasiliensis, certain fungi may be involved (Arch. Path. Lab. Med. 113: 476, 1989).
Sporotrichosis produces superficial or deep spreading infections following a prick from a rose or bayberry thorn. Look for "cigar bodies", the fungi, which are often hard to find. 
* Chromomycosis produces skin lesions that resemble blastomycosis. This is primarily a Mexican and Caribbean infection.
THE SUPERFICIAL FUNGI: You'll study ringworm, tinea versicolor, etc., in "Micro". Don't worry about them just now! Occasionally one can "go deep" in the immunocompromised.
 Trichosporonosis
Trichosporonosis
White piedra organisms
Pittsburgh Pathology Cases {08148} ringworm
{12118} tinea pedis
{12268} tinea pedis
{14208} tinea pedis
{12182} tinea versicolor
{12267} tinea corporis
{14220} tinea corporis
{12270} tinea cruris
{14229} tinea unguum
{14232} tinea capitis
{14233} tinea capitis, black dots
The yellow rain business (Science 214: 1008, 1981, Science 217: 31, 1982; Science 218: 1202, 1982; Nature 308: 485, 1984, Nature 309: 205 & 207, 1984)In the early 1980's, the Reagan administration accused the Soviets of spraying biological weapons on Hmong tribespeople and Khmer Rouge soldiers in remote area of Laos and Cambodia. During the height of the flap, Reagan's State Department alleged that thousands of civilians had been slaughtered in this way.Accounts were horrorific. Airplanes sprayed a substance, and people collapsed, bleeding from multiple orifices.The substance was supposed to be yellow, and to fall in large drops, like rain. Samples of material supposed to be "yellow rain" were analyzed in government labs. They were found (by the current assays, and often close to the detection limit) to contain trichothecenes, powerful fungal poisons. Was this Soviet biologic warfare?Yes!
- It is hard to dismiss the very dramatic accounts of the spraying of poisons and the mass sickness and death.
- The Soviets supposedly had developed a mycotoxin spray to control forest pests.
- The government showed reporters a Soviet gas mask that had trichothecenes on it.
No!
- It is hard to know how much trust to give accounts from refugees who may be asylum-seekers.
- So far, nobody from the former Soviet Union has talked about doing this.
- Some of the material was simply the feces of bees, who in these areas sometimes leave the hives for mass defecations; "yellow rain" is now known to occur naturally as far away as Malaysia. (Nature 341: 191, 1989).
- Trichothecenes are nerve poisons but the animal models don't include bleeding.
- Trichothecene has a half life of ten minutes in humans, but the "survivors" in whom it was found had been "attacked" up to 18 days earlier.
- Newer assays show trichothecenes, including T-2 (the really bad one) are rather common in various environments.
- Mycotoxins are an inefficient way to kill people. It takes about 35 mg to kill a grownup, and they're very expensive.
- Nobody has an autopsy series or even a bunch of bodies with the same findings.
- Americans who actually visited the Hmong in their regular homes couldn't find anybody who claimed to know about biological weapons being used against them.
- It is hard to explain why the Soviets would use these very illegal weapons, and outrage the international community, when there are already effective, lethal, much cheaper war gases.
I remain undecided as to whether chemical weapons were used by the Soviets in their wars in Southeast Asia.
Learning Objectives: "Critters" For each of the infections covered in this unit, explain:
- where it is endemic;
- how it is spread;
- its pathogenesis;
- how to recognize it.
Recognize in a photomicrograph the infectious agents of each of the following:
- "amebic dysentery"
- cryptosporidiosis
- giardiasis
- trichomonas
- pneumocystosis
- malaria
 (no need to speciate)
(no need to speciate)
- African sleeping sickness (no need to speciate)
- schistosome
 eggs (distinguish 3 species)
eggs (distinguish 3 species)
Recognize each of the parasitic worms, given a scale and some clinical clues. NOTE: We are
not concerned with your learning taxonomies or intricacies of life cycles for these organisms, or the nuances of parasite identification (e.g., how many spots on a bancrofti's tummy, etc., etc.). You'll learn as much of this as you need in "Med Micro". For Pathology, you
do need to know how and where these infections are contracted, and what they do to their victims. Knowing the rough sizes of the organism will help you recognize them in pictures* * Fear of the public toilet. The parts that several people touch may be contaminated with worm eggs of various kinds (Brazil abstract 95241825), transmissible hepatitis A (Eur. J. Epidem.
14: 187, 1998), rotavirus (Eur. J. Epidem.
11: 587, 1995), no doubt many others. Do wash your hands after. INTRODUCTION TO THE NON-FUNGAL EUKARYOTIC INFECTIOUS AGENTS ("critters")
The protozoan and helminthic (worm) infections are among the foremost causes of sickness and death worldwide. We have the knowledge to control most of these diseases. Even more than with other categories of diseases, the problems with getting this implemented are political, economic, and behavioral. Protozoa ("first life") is a misnomer for unicellular animals. (The opposite is metazoa, multi-cellular eukaryotes. Work with ribozymes has greatly blurred the border between the living and the non-living.) "Protozoa" are not only eukaryotes, but highly specialized. Luminal protozoa Amebiasis
Amebic meningoencephalitis
Balantidium infestation
Cryptosporidiosis
Isosporidiosis
Sarcocystosis
Giardiasis
Trichomoniasis
Pneumocystosis
Blood and tissue protozoa Malaria
Babesiasis
African trypanosomiasis
Intracellular protozoa Chagas's disease
Leishmaniasis
Toxoplasmosis
Both parasitic protozoans and parasitic worms have developed intimate relationships with the biology of their hosts. (* Ignore "Big Robbins" on "design"; even before Darwin's work, it was pretty obvious that parasites evolved right along with their hosts.) The most successful parasites (giardia, amoebas) cause their hosts little or no grief. Virulence factors of the others remain largely unknown, and details of host response are generally unclear, too. These critters don't belong in your body, but their presence doesn't always make you sick. The word infestation can be used whenever they are on board, whether or not they produce symptoms.
AMEBIASIS
{08289} entamoeba histolytica (smear, trust us)
{08405} entamoeba histolytica
{11130} ameba, colon; three of them ate red cells
{26396} amebiasis ulcers in the colon
{46272} amebas, they have eaten red cells
{46273} amebic liver abscesses, trust me
This is infestation / infection with Entamoeba histolytica, primarily a colonic disease. Patients have acute or chronic diarrhea ("amebic dysentery"). Usually the amoeba is a commensal, and symptoms are unusual. The organism is typically acquired in the Third World (Latin America, India) or by certain male homosexual practices (J. Inf. Dis. 159: 808, 1989; most gay amoebas are non-virulent). Around 40 million people become seriously sick each year (J. Inf. Dis. 164: 825, 1991). Ingested cysts (the form able to survive in the outside world) are activated in the stomach, releasing active trophozoites. Many years may elapse between inoculation and symptomatic disease. Future lab doctors: The four little nuclei of E. histolytica impart the famous "Remington shaver" appearance. Nasty amoebas move rapidly ("explosively") and phagocytize red blood cells. Even among such amoebas, some strains are much nastier than others. Virulent amoebas drill holes ("amebophores") in host cells, using a virulence protein. Detecting such strains: J. Inf. Dis. 164: 825, 1991.
The colon (especially the right side) is affected. The amoebas penetrate the crypts, burrow down, stop at the muscularis mucosae, and spread out; the undermining creates the "Erlenmeyer flask" ulcer. Eventually the mucosa sloughs, and diarrhea becomes severe. The ulcers are, as you would expect, full of fibrin and debris as well as amoebas. However, don't expect to see any inflammatory response. Sometimes there is a profusion of granulation tissue, simulating a tumor ("amoeboma"). Rarely, the bowel perforates.
The most serious complications are extra-intestinal. In around half of clinical cases, amoebas make their way to the liver, where "abscesses" (misnomer) are really expanding areas of necrosis without a significant inflammatory response. The old-time gourmet pathologists compared the material in an amoebic abscess to "anchovy paste". It's apopsosis (Lancet 361: 1025, 2003). They may become superinfected by bacteria, rupture into the peritoneum, pericardium, pleura, or wherever, and/or spread by the bloodstream to the lungs or brain.
Note: The lab can distinguish E. histolytica from some non-pathogenic amoebas (* E. nana, E. coli, others) by morphology. The latter are proof of significant fecal-oral contamination. However, as noted, most E. histolytica strains are probably non-pathogenic, and even the presence of virulent strains in stool does not indicate that this is the cause of the patient's symptoms. * There's a current pop idea that infestation with amoebas is an important cause of "functional bowel syndrome". It is probably not true (Lancet 349: 89, 1997).
BALANTIDIUM COLI
{08398} balantidium
This very large ciliated intestinal parasite occasionally causes illness worldwide. It's caught from pig feces. The pathology and clinical syndrome are pretty much the same as in amebic colitis.
AMEBIC MENINGOENCEPHALITIS
Naegleria fowleri live in stagnant ponds, especially in the warmer states. The amoebas enter through the CNS through the nasal mucosa, cribriform plate, and first cranial nerves. Around 5 days after exposure, they produce a purulent, necrotizing, hemorrhagic infection of the brain and its coverings. A healthy pond-swimming kid can be dead in a few days.
* Expect poison from standing water.
Acanthamoeba ("Hartmanella"; I call it "the Salerno butter cookie bug") is a related organism that can cause chronic meningoencephalitis in immunosuppressed people, and can also cause corneal infections ("keratitis") in contact-lens users (JAMA 261: 343, 1989; Am. J. Ophthalm. 106: 628, 1988; 107: 331, 1989).
* Balamuthia mandrillaris is a baboon amoeba that occasionally affects people (brain, skin) chronically. The tissue reaction is a fooler for "malignant lymphoma with granulomas" (J. Inf. Dis. 179: 1305, 1999) or "just plain granulomas (Lancet 362: 220, 2004). Pathologists see Arch. Path. Lab. Med. 128: 466, 2004.

GIARDIASIS: The world's most ubiquitous gut protozoan
{00440} giardia
{08395} giardia
{09756} giardia (gut lumen)
Giardia lamblia, an intestinal flagellate that affects various wild animals, can be acquired from drinking stream-water (Colorado is famous), drinking tap-water (the Soviet Union, especially Leningrad, is famous), or engaging in male homosexual practices. Giardia concentrates in the duodenum and sends cysts out in the stool. Most giardia infestations never become symptomatic. But the bug sometimes causes indigestion (stinky "purple burps"), diarrhea, and even malabsorption, by coating the gut and damaging the villi. Low IgA, general hypogammaglobulinemia, or immunosuppression (Am. J. Gastroent. 84: 450, 1989) makes giardia infection more severe. We suggest a high index of suspicion for giardiasis (Arch. Int. Med. 149: 939, 1989), and a duodenal aspiration as the best means of searching. In smears, giardia shows a cute "ghost face". In sections, you'll see mostly sickle-shaped structures. * Fun to know: Giardia is supposedly the only common eukaryote without mitochondria (Nat. 429: 236, 2004).
CRYPTOSPORIDIOSIS (Clin. Lab. Med.
11: 873, 1991; Lancet
345: 1128, 1995)
{15548} cryptosporidium
{27368} cryptosporidium, acid-fast stain
 Cryptosporidiosis
Cryptosporidiosis
Tom Demark's Site This newly-discovered but common disease (Milwaukee 1993 NEJM 331: 161, 1994) produces outbreaks of mild, self-limited diarrhea, especially in children.The tiny, acid-fast organism is a common veterinary pathogen and veterinary commensal. The creatures sit in the brush border of the gut and enjoy the free food. Acid-fast staining of the stool shows the cyst stage. It can be fatal in a malnourished child. And AIDS and AIDS-related complex patients get a longstanding diarrhea that can also be fatal. * Swimming pool cryptosporidiosis: Am. J. Pub. Health 82: 742, 1992, Maine apple cider fiasco JAMA 272: 1592, 1994; volunteers NEJM 332: 855, 1995). Nosocomial cryptosporidiosis (spread by a bewildered patient by way of the ice machine): Br. Med. J. 302: 277, 1991). 1/3 of peace corps volunteers turn positive: Arch. Int. Med. 149: 894, 1989)
Isosporidia belli is a related organism seen in AIDS patients. It causes diarrhea and malabsorption (isosporiasis). * Sarcocystosis is an uncommon, mild infection acquired from eating undercooked beef or pork. It produces intestinal problems that last for a few weeks. The animals catch it from human feces. There are several other related illnesses caused by protozoans.
TRICHOMONIASIS (
Trichomonas vaginalis)
{46498} trichomonas, smear
This 15 micron flagellate is a very annoying, though nonlethal, sexually-transmitted pathogen. Most patients who harbor trichomonas are not symptomatic. The agent is best-known for producing vaginitis in women during reproductive years. Men get urethritis and prostatitis. In both sexes, itching, burning, and discharge are seen. The discharge in vaginitis is scanty and frothy, and often malodorous; it is usually not purulent. Gynecologists talk about "strawberry vagina", etc. Future gynecologists: The diagnosis is clinched by finding the bugs in a wet mount, or on Pap smear.
PNEUMOCYSTIS PNEUMONIA (
Pneumocystis carinii; the official name is now P. jirovecii yee-row-vet-zee)
{00431} pneumocystis, silver stain
{00456} pneumocystis, silver stain with H&E counterstain
 Pneumocystis
Pneumocystis
Lung pathology series
Dr. Warnock's Collection This ordinarily-harmless organism (formerly a "protozoan", the DNA shows a closer relationship to fungi) affects the lungs, and seldom any other organ. The cysts are 4-6 across. Trophozoites, around 2-4 across, grow on the pneumocytes and probably damage them. The alveoli fill with organisms and cell debris. Since the organisms do not stain on H&E, the exudate appears "honeycomb", "frothy" or "foamy". Today, you will usually make the diagnosis following bronchial lavage. After recovery, the debris can lie around for weeks. It was first known as the cause of plasma cell interstitial pneumonitis in malnourished kids. In AIDS patients, the inflammation is scanty or nonexistent, and the organisms float in "froth" within the alveoli, and at autopsy, a pattern of diffuse alveolar damage is often seen. The macrophage receptor necessary to fight pneumocystis has been identified; it is gone in AIDS: Nature 355: 155, 1991.
In less-impaired hosts, we now know that pneumocystosis can cause a mild respiratory illness (NEJM 324: 246, 1991). Rarely, in the immunocompromised host, pneumocystis can cause extrapulmonary disease (NEJM 326: 999, 1992).
 Pneumocystis
Pneumocystis
Silver stain
WebPath Photo MALARIA
{13700} malaria, peripheral blood
{46249} malaria, brain; note pigment
 Plasmodium vivax
Plasmodium vivax
Text and photomicrographs. Nice.
Human Pathology Digital Image Gallery
Infestation by any of four Plasmodium species. This disease causes tremendous morbidity, especially among young children, especially in the poor nations of Africa and Asia. (At least 1 million kids die of malaria every year just in Africa; Science 261: 605, 1993). The WHO rates malaria as the world's worst primary health problem. Plasmodia are intracellular parasites carried by female Anopheles mosquitoes. Humans are the intermediate host (i.e., the parasites have sex inside the mosquito, not inside us.) You'll learn the whole life cycle in "Micro". Sporozoites from the mosquito travel to the human's liver, where they multiply. Merozoites from the liver enter erythrocytes, where they multiply to produce trophozoites and then schizonts. The schizonts disrupt the red cells. Gametocytes, produced occasionally in the red cells, re-infect the mosquito.
Most of the symptoms are due to the involvement of red blood cells, which are lysed in unison. Plasmodium malariae produces fever spikes at 72 hour intervals ("benign quartan malaria"), and often lies latent for years. Plasmodium ovale and Plasmodium vivax produce fever spikes at 48 hour intervals ("benign tertian malaria").
 Malaria
Malaria
WebPath Photo Plasmodium falciparum produces fever spikes at 48 hours ("malignant tertian malaria") and is bad. (1) This form of malaria, unlike the others, can affect red cells of any age; (2) Infestation makes red cells adherent to endothelial cells (biochemistry Proc. Nat. Acad. Sci.
93: 3497 & 3503, 1996) and prone to plug vessels. * Thinkers: Why are the cycles exact multiples of 24 hours?
The symptoms and signs can easily by understood by those familiar with basic disease processes. Massive hemolysis correlates with the paroxysms of fever, chilling, and so forth. Organisms in the liver can cause hepatomegaly. The spleen is generally enlarged, often huge and fibrotic in falciparum malaria. The phagocytic cells are infected. Look here for hemozoon, the Prussian-blue negative iron pigment of malaria; formation of this pigment is likely to deplete marrow iron stores. In really bad malaria, there is plugging of brain vessels by parasitized red cells. * Around these, you might see "ring hemorrhages". * "Dürek's granulomas" (misnomer) are inflammatory reactions here, with glial stuff. Increased intracranial pressure kills in lethal cerebral malaria: Lancet 337: 573, 1991. Update on the pathophysiology: NEJM 372: 1126, 2015.
"Blackwater fever" (usually seen in falciparum malaria) results from vigorous hemolysis, and renal failure resulting from hemoglobinuria. * Don't worry now about immune glomerulopathies (membranous, membranoproliferative I)
* Blood bankers and geneticists: Plasmodium vivax ignores cells that are Duffy-negative. Hgb S causes the parasite to leave the red cell. G6PD deficiency gives protection also. * Since there's no vaccine triumph yet, the best news in malaria control recently is insecticide-impregnated netting. And this is good news -- its use seems to cut total young-child mortality by about 20% in the worst malaria zones (Lancet 357: 1241, 2001). The newest resistant strain calls for new drugs, but no one is willing to make these for a world that cannot pay: Science 256: 1135, 1992. The scandal of the World Health Organization's approach to malaria, promoting drug regimens that are known not to work: Lancet 363: 237, 2004. The 1990's malaria vaccine (Lancet 337: 998, 1991; Science 252: 715, 1991) was developed by a Columbian physician without peer review or red tape; he merely cloned the three best epitopes. It's no panacea, but it apparently helps (Science 267: 237, 1995; NEJM 336: 86, 1997; J. Inf. Dis. 175: 921, 1997). The new one that we all hope will work uses intact falciparum sporozoites (NEJM 361: 468, 2009). * Medical history buffs: Before penicillin, it was fashionable to give syphilis patients a dose of malaria, since the fever or cytokines supposedly killed the spirochetes. Whether or not it worked, it made physicians kinder to these patients -- it's easier to be nice if you think you really have something to offer Am. J. Psych. 152: 661, 1995.
patients a dose of malaria, since the fever or cytokines supposedly killed the spirochetes. Whether or not it worked, it made physicians kinder to these patients -- it's easier to be nice if you think you really have something to offer Am. J. Psych. 152: 661, 1995.
TOXOPLASMOSIS (
Toxoplasma gondii)
{06202} toxoplasmosis in a smear
{08235} toxoplasmosis
{08277} toxoplasmosis
{15472} toxoplasmosis of brain
{23494} toxoplasmosis; world's puniest granulomas
A crescent-shaped coccidian parasite of cats. It incidentally infects many animals. Eggs are shed in cat feces, and if ingested, can infect most mammals. The organisms are intracellular. Small crescentic "tachyzoites" (3-6 ) may be seen, and so can "cysts" (really, loaded host cells) full of "bradyzoites". Leave the diagnosis of "toxo" in tissue to us. Pathologists talk about "monocytoid B-cells", with dented nuclei are clear borders. The human infection, which is very common worldwide (around half of people in the U.S. have antibodies) is caught from cat droppings or eating raw meat from an incidentally-infected animal, or by transmission across the placenta. Unfortunate toxoplasma organisms infecting a human host can only complete their life cycle if the human is eaten by a cat, lion, saber-tooth tiger, etc. They would prefer to infect mice. No, AIDS victims need not banish their pet cats (JAMA 269: 76, 1993).
The human response to toxoplasmosis varies with age and immune status. Adults with normal immunity suffer only a mild, infectious-mononucleosis-like illness. Don't expect to see organisms in tissue section. If you must establish the diagnosis, animal inoculation studies are necessary. In fetuses, newborns, or the (even mildly) immunocompromised, toxoplasmosis is a devastating infection, capable of severely damaging the eyes and brain. The process continues following birth, and it's wise to screen newborns for it (NEJM 330: 1858, 1994).
OTHER PROTOZOANS
Babesiasis (* Piroplasmosis, babesiosis; NEJM 366: 2397, 2012)
{46497} babesia in a red cell
An endemic, usually trivial disease in the Nantucket/Martha's Vineyard area (and other places in Europe and North America) caused by Babesia microti. It is carried from its animal reservoir by ticks (Ixodes dammini) which are active in the summertime. The organisms grow in red cells but produce no pigment. They can travel in blood transfusions, and they can hang around in your blood indefinitely even if you're "treated" (NEJM 339: 160, 1998). The infection is almost always subclinical unless the patient has been splenectomized or is severely diabetic. New babesiosis-like bug in northern California: NEJM 332: 298, 1995.
African Trypanosomiasis ("sleeping sickness")
{08241} African trypanosomes in a blood smear
Dread infections caused by hemoflagellate trypanosomes and carried by tsetse (Glossina) flies. Trypanosoma (brucei) gambiense: West African sleeping sickness. Humans are probably the only reservoir. This disease leads to meningoencephalomyelitis and brain damage after several years. * "Winterbottom's sign" in this variant: Large posterior cervical nodes.
Trypanosoma (brucei) rhodesiense: East African sleeping sickness. This form has an important reservoir in cattle (Lancet 358: 635, 2001) and wild antelopes, and has a shorter time course (weeks) before brain damage.
A "red rubber chancre" (local proliferation of the organism) is common, but not invariable, at the inoculation site; * rarely, an acute illness with DIC occurs when first meeting the organism. Continuing, genetically-programmed changes in the organisms' antigens protect it from the immune system and correlate with recurring fevers. Ultimately, both T-cell and B-cell mediated immunity become impaired. For some reason, there is a striking but ineffective B-cell hyperplasia (lymphadenopathy, big spleen, plasma cells, Russell bodies).
At autopsy, a heavy chronic inflammatory infiltrate, with many plasma cells, is seen in the brain. There is preferential loss of neurons and proliferation of glia. There is also widespread loss of myelin. * Exactly how we fight trypanosomes on our own is a longstanding mystery that's only now being clarified: Science 268: 204 & 284, 1995). * Historically, the treatment of the CNS form (arsenicals) has been almost as bad as the disease. Prednisone therapy seems to help considerably (Lancet 1: 1246 & 2: 573, 1989).
Chagas's disease ("American trypanosomiasis"; update on a very complicated problem Circ. 115: 1009, 2007; Lancet 375: 1388, 2010; Science 333: 934, 2011). Chagas disease in Peru's shantytowns: Lancet 372: 16, 2008.
{08299} reduvid bug
{26573} Chagas's disease smear; don't worry about telling it from its African counterpart here
{26576} Chagas's heart, tremendous dilatation
{26579} Chagas's disease, heart histology (lymphocytes)
{26582} Chagas's disease, heart histology (lymphocytes and parasites)
Trypanosoma cruzi is carried by the reduvid "kissing" bug, which infests poor homes in much of Latin America; its range extends into South Texas. Natural reservoirs exist among armadillos and other wildlife. In the human, the trypanosome appears in the blood (the "C" shape is typical). After entry, it cycles between a leishmania form for intracellular multiplication, eventually causing cells to burst and release more trypomastigotes to infect bugs. Following inoculation, there is likely to be inflammation of the eye and lymphadenopathy on the same side ("Ramona's sign"), followed in a few weeks by systemic signs. In both acute and chronic forms, death results from cardiac involvement (rhythm disturbances, pump failure). However, brain involvement and esophageal paralysis ("mega-esophagus") and colonic paralysis ("megacolon") are also important. The latter result from neuron damage and are not reversible. The disease can pass to the unborn child, producing brain damage or abortion.
The mechanism of injury in chronic Chagas disease seems to be autoimmunity, since the heart is massively infiltrated with killer T cells, and there are only a few microbes. Older study: Am. Heart J. 94: 301, 1999. See Circulation (above) for new evidence that the protozoan must persist to allow the disease to continue. * Charles Darwin was attacked in South America. His cardiomyopathy may have been chronic Chagas's disease. * Ask a microbiologist about xenodiagnosis; it requires a "clean" reduvid bug. There are about 15,000 deaths yearly from Chagas; the disease is difficult to treat (the drugs only work in the acute phase), and it's spreading by new routes. See Lancet 373: 1820, 2009. Chagas in in the US, though seldom transmitted; the bugs are in most of the southern half of the US (JAMA 313: 1196, 2015) and evidence of infection is found in occasional blood donors, many of whom are outdoors people.
Leishmaniasis (Am. Fam. Phys. 69: 1455, 2004.) A variety of clinical syndromes caused by various species of a small (1-5 micron) protozoan which is endemic in wild animals. They look like two blue dots. They are carried by sand-flies (Phlebotomus) species, and all have important animal reservoirs. Kala-azar ("black fever", Operation Desert Storm "Baghdad boil"; L. donovani; Lancet 303: 336, 1991) involves massive infiltration of spleen, liver, nodes, marrow. Untreated, hematopoiesis eventually fails resulting in death. There are half a million cases of this dread disease yearly, most of then in India or South America. * A breakthrough came in 2002, with the introduction of oral miltefosine for treatment of this dread infection (NEJM 347: 1739, 2002).
{08393} mucocutaneous leishmaniasis
{11466} leishmaniasis, "oriental sore"
{08230} Leishmania in macrophages
{06211} Kala-Azar, bone marrow smear; can you find the one cell that is infected?
{46243} Kala-Azar, histology
{08423} leishmaniasis, "oriental sore"
 Leishmania in smear
Leishmania in smear
Wikimedia Commons
Cutaneous leishmaniasis ("tropical sore") is a mild, self-healing lesion in warm countries of both worlds. Eventually, the organisms are controlled by granuloma formation. Mucocutaneous leishmaniasis is common in South America. The pathology is primarily chronic, non-healing ulcers. Diffuse cutaneous leishmaniasis occurs when there is extreme T-cell dysfunction, and look clinically much like lepromatous leprosy . * There is a skin test ("leishmanin") to detect immunity. It does not turn positive for 3 months, and is negative in the sickest patients. * A new variant from Honduras: Lancet 337: 67, 1991.
. * There is a skin test ("leishmanin") to detect immunity. It does not turn positive for 3 months, and is negative in the sickest patients. * A new variant from Honduras: Lancet 337: 67, 1991.
INTRODUCING THE WORMS *
{31826} worms in apple
* The earthworm is a familiar symbol of humility and mortality. Shakespeare: Men have died from time to time, and worms have eaten them, but not for love. William Blake: I have said to the worm, 'You are my mother and my sister.' Ed Poe: The play is the tragedy, "Man",/ And the hero, the Conqueror Worm."
In the following infestations, peripheral blood eosinophilia can be a helpful tipoff (remember "tropical eosinophilia"), but it is not very sensitive and not very specific:
- ascariasis
- filariasis
- onchocerciasis
- strongyloidiasis
- trichinosis
- visceral larva migrans
Reminder: Wherever there are lots of eosinophils, look for Charcot-Leyden crystals, composed of a strongly-alkaline protein from eosinophil granules. This goes double if you are checking stools for exotic worms.
INTESTINAL ROUNDWORMS
{08309} ascaris in child's intestine
{24673} ascaris
 Ascaris
Ascaris
WebPath Photo Ascaris lumbricoides (* recall the "lumbrical" muscles of the hand?) is a big roundworm up to a foot long. Larvae hatch from ingested eggs in the stomach, travel through the lungs, are coughed up and swallowed, and settle in the gut. Ascariasis causes three kinds of problems. Everyone is allergic to ascaris worm, and these organisms can cause dyspnea ("tropical eosinophilic pneumonia", etc.) as they pass through the lungs. The worm burden can be so heavy that they occlude the gut. Excited worms can plug a bile duct, perforate the appendix, pierce the bowel, and so forth. * King Richard III had ascaris worms: Lancet 382: 888, 2013.
Trichuriasis ("whipworm") This generally-harmless little (5 cm) worm has no tissue phase, merely dwelling in the gut with its little head in a crypt. Its eggs are ingested with fecal contamination. Heavy infections occur under conditions of poor sanitation, and can be fatal.
* Anisakis ("whaleworm")An up-and-coming infectious agent from seafood, which can render a person quite allergic. You eat the larvae, which are rather durable and can probably survive microwaving and household refrigeration. Anisakis is a known cause of seafood allergy, and a "usual suspect" in "idiopathic anaphylaxis", "idiopathic urticaria" (Br. J. Derm. 139: 822, 1998), "occupational asthma", "eosinophilic gastroenteritis" (Allergy 53: 1148, 1998), vague GI complaints, and even Crohn's.
Enterobiasis ("pinworm") Enterobius vermicularis is a small (1 cm) worm that causes night-itch when the female worm migrates to the anal skin for nightly egg-laying. Mama Pinworm wants the child to scratch here, then put fingers into their own mouths and the mouths of their family membrrs. Unlike most roundworms, the life-cycle is entirely within the intestine. The infection is contagious in households. The familiar Scotch-tape test demonstrates diagnostic eggs.
{39229} pinworm egg; this is the only egg worth knowing for a family physician
* Long blamed for "causing some cases of appendicitis", the worm also takes the blame for an unknown number of cases of pelvic inflammatory disease by migrating up the vagina and uterine cavity to the oviducts.
Hookworm (Nature 337: 114, 1989)
{08122} hookworm portal of entry
{08123} hookworm larva
{08124} hookworm jaws
Necator and Ancylostoma are small (1 cm) worms that bite into the duodenal mucosa and nibble on blood cells. The infection is acquired from the soil, where the larvae must mature. They enter through the body, typically through the soles of the feet (i.e., this is why you've been told to wear shoes outdoors), pass through the lungs, and are coughed up and swallowed. The usual problem in heavy infestation is iron deficiency. Hookworm was once ubiquitous in the American Southeast; both "New World" and "Old World" hookworms can be caught in either hemisphere, wherever the soil is moist and warm.
Strongyloidiasis
{00398} strongyloides in the gut
{15737} strongyloides
{15738} strongyloides
{32024} strongyloides
Strongyloides stercoralis is a tiny (1 mm) intestinal worm that is endemic in much of the world, including Appalachia. The larvae generally must mature in the soil, but in immunosuppressed (iatrogenic, malnutrition) patients can mature in the gut and produce potentially lethal "hyperinfection". The hyper-infected patient may suffer malabsorption (from the worm burden on the gut mucosa), cough (from larvae travelling through the lungs), or even repeated bouts of sepsis or CNS infection. Though rare, it's good to know you have the creature on board before a bone marrow transplant; the big cancer centers now screen everyone (Cancer 100: 1531, 2004).
* Capillariasis is a Filipino roundworm, contracted from eating uncooked fish.
TISSUE ROUNDWORMS
Visceral larva migrans This occult infection (i.e., no eggs or parasites in the stool) is produced when larvae of Toxocara, acquired from dogs or cats, travel among human viscera in a vain search for a place to develop into adults. The abdominal organs and/or lungs are hardest hit, but most organs, including brain and eyes, can be involved. Patients present with various confusing symptoms and signs. Lots of circulating eosinophils may suggest the diagnosis, which can be confirmed serologically. Cutaneous larva migrans is a similar process, localized to the skin. Oh, gross!
{15756} larva migrans
Dracunculosis ("Guinea worm"; MMWR 40: 5 & 245, 1991)
{08304} dracunculus
{08397} dracunculus
Dracunculus medinensis is a big worm up to 12 cm long. The intermediary host is the fresh-water cyclops, and infection probably results from exposure to contaminated water. Humans are required for the life-cycle, and because of its ecology (the person must urinate in stagnant water; the worm must reproduce each year), this is another disease that could probably be eliminated from the world -- this time without a vaccine, but simply by public health surveillance. See below.
After migrating, the guinea worm larva encysts in the skin, causing a painful nodule. * Some have thought that the "fiery serpents" mentioned in the Hebrew scriptures were dracunculiasis. If the worm dies, secondary infection is the rule. Beware of tetanus !
!
During the 1990's, around 5-10 million people are currently miserable with dracunculosis. Endemic foci exist both in Africa and in India-Pakistan. Eradicating the worm is now well-underway, and today is seems to exist only in areas of Africa where political instability makes eradication impossible (Lancet 373: 1159, 2009; Lancet Inf. Dis. 9: 149, 2009). One of the leaders in this world-wide effort was former US president Jimmy Carter (Lancet 361: 1108, 2009). The single-snake (i.e., medical) "caduceus" probably derives from the ancient practice of wrapping the worm around a stick to extract it without killing it (and leaving dead stuff behind to get infected). * Before the "white flag" (or flags in general) became the standard, a staff with two ribbons was carried by those desiring a truce or parley. As a symbol for heralds, ambassadors, and messengers, this important symbol became conflated (in the USA and Canada) with the doctor's emblem to produce the two-snake caduceus, which reappeared in modern times as the symbol of the telegraph company. The classical personifications of the two forms of the caduceus are, respectively: One snake and maybe a gnarl in the wood: Rod of Asclepias (Aesculapius), whose portfolio was healing and medicine; Two snakes and maybe wings: Caduceus of Hermes (Mercury), whose portfolio included heralds, messengers, fast-talkers, stealthy operators, thieves, and profiteers. 'Nuff said? For more, see Lancet 364: 416, 2004.
Trichinosis
{08214} trichinella
{08215} trichinella
{15750} trichinella
Infection by Trichinella spiralis follows ingestion of uncooked meat with live cysts. Everyone knows the hazards of eating raw pork; bear meat and wild boar meat are also famous. Remember that smoked meat is not cooked, and beware exotic ethnic delicacies (cougar jerky J. Inf. Dis. 174: 663, 1996; bear is also notorious).
The larvae are released from cysts by digestion of the wall, and a mild GI upset is likely to follow. The worms breed in the gut, dying after they release larvae into the lacteal. In people, the worms encyst in individual striated muscle cells, beyond the reach of the immune system. They cause myalgia and sometimes cardiac failure. The organisms prefer well-oxygenated (i.e., busy) muscle, and are happiest in the heart, diaphragm and extraocular muscles. Eosinophilia is an important tipoff, and should prompt questions about eating habits. The diagnosis can be confirmed serologically or by biopsy. * Outbreak in Serbian Bosnia in 1996 traced to one meat company: Am. J. Med. 107: 18, 1999. Many people had cardiac involvement, but most made good recoveries.
FILARIASIS
{08390} filaria
Lymphatic filariasis Infection by Wucheria bancrofti or Brugia malayi, carried as larvae by mosquitoes. These problems are widespread in the tropics. The larvae travel by way of the bloodstream. The mature worms (living or dead) harm the patients by plugging lymphatics, and producing granulomas and scarring which further obstruct the lymphatic channels. Heavy infestation results in chronic lymphedema ("elephantiasis") of the genitals and less often of the extremities. The immune response varies greatly even within a community (Lancet 337: 1005, 1991). Most people mount a good allergic response to these worms. A systemic illness with a high eosinophilic count is common. The WHO has targeted this disease for elimination, and treating entire communities once a year greatly decreases its prevalence (Lancet 351: 152, 1998). Right now, a popular intervention is simply to fortify the local salt supply with diethylcarbamazine (Am. J. Trop. Med. 65: 865, 2001, from the CDC). * Fun to know: Diethylcarbamazine was first developed by Stephen Hawking's father (Lancet 385: 1069, 2015.)
During the past few years, donation of medications by GlaxoSmithKline (albendazole) and Merck (ivermectin) has resulted in tremendous gains (Lancet 373: 529, 2009). During 2007, 546 million people received medication -- what percentage of the world's population is that?
 Filaria
Filaria
WebPath Photo
Onchocerciasis ("river blindness"; Br. Med. J. 304: 1285, 1992) Infection by Onchocerca volvulus (up to 50 cm), a worm whose larvae are transmitted by black flies in Africa and Latin America. The vectors must breed in the water and are poor fliers. The disease is transmitted only near the rivers.
The mother worm lives in the skin and discharges larvae into the surrounding tissues. Severe dermatitis results, and elephantiasis occurs in extreme cases. Even worse, the larvae often invade the eye chambers, producing blindness which often affects most adults in entire communities.
* The living worm somehow sequesters itself from the immune system. The Mazzotti reaction is extreme inflammation when antigens become exposed after therapy kills the worms. Ivermectin was a major breakthrogh in worm therapy (Lancet 341: 130, 1993); for some reason, it causes the worms to migrate away from the skin and eyes to die. * The worst pathology is actually caused by commensal bacteria that live in the worms, and enable them to reproduce and injure tissue (Br. Med. J. 326: 207, 2003); the tetracyclines are now in use to kill these bacteria, with good results.
As president of the World Bank, Robert McNamara (formerly the architect of the Vietnam fiasco) became aware of onchocerciasis while visiting Africa, and coordinated an international, multi-organization, non-bureaucratic and highly effective effort to eliminate it. Merck's donation of ivermectin to the world's poor has resulted in a massive decrease in the prevalence of onchocerciasis. Thanks.
Minor tropical filariae "Big Robbins" correctly notes that these worms seldom cause devastating illness. However, it is always disturbing to see an African Loa loa worm travelling under someone's conjunctiva. * Future pathologists: Look for filaria on the feather-edge of the peripheral bloood smear; you are likely to miss them if you look in the "good part".
Zoonotic filaria Dirofilaria, the dog heartworm, can grow (but can't mature) in a human heart. Usually it embolizes from the right side of the heart into the lung, where it produces a coin lesion that will require surgery to rule out cancer. * People may also become infested with certain raccoon filaria.
TAPEWORMS ("Cestodes")
Everyone remembers tapeworms from grammar school biology. Less well-known are the larval cestodiasis syndromes, in which larval forms invade human tissues ("Man as definitive host"). Intestinal tapeworm infections: Humans as intermediate hosts Taenia saginata ...beef tapeworm Taenia solium ... pork tapeworm Hymenolepis nana... dwarf tapeworm Diphyllobothrium latum... fish tapeworm After the person eats the appropriate uncooked food, these creatures attach to the bowel wall. They are usually asymptomatic, but may plug the bowel or (in the case of fish tapeworm) cause disease by taking up all available vitamin B12.
Cysticercosis (Lancet 362: 547, 2003): Humans as definitive host; the infection is actually acquired (by both humans and pigs) from eating food contamined with eggs from feces (your own or somebody else's). In some of the poor nations, pigs are actually used for human waste disposal, which keeps the epidemic going.
{09793} cysticercosis from brain
{43801} cysticercosis from brain
 Cysticercosis
Cysticercosis
Pittsburgh Pathology Cases If a human ingests the egg of a pig tapeworm (his own worm, or someone else's), it will hatch into a larva that will invade the tissues, preferring the brain. The worm encysts as a white 1-1.5 cm sphere with a scolex inside. While the organism can be killed with medicine and is probably dead already, the remains won't just disappear. Cysticercosis is the most common cause of epilepsy in many developing countries, especially in Latin America (Lancet 338: 549, 1991; article describes a new blot for making the diagnosis; ELISA blood test flops: Arch. Neurol. 49: 633. 1992).
Echinococcus ("Hydatid disease"; Arch. Surg. 124: 741, 1989; Lancet 362: 1295, 2003)
{08256} echinococcus worm
{08275} echinococcus cyst in brain
{24665} echinococcus cyst in liver
{08255} echinococcus, babies from a cyst plus lots of hooklets that fell off
{08411} echinococcus babies
These tapeworms live in the intestines of dogs, which are usually symptomatic. The infections are transmitted between wolves and caribou, Eskimo sled dogs and moles, Scottish sheepdogs and sheep, etc. * Reykjavik, Iceland banned all dogs within the city limits because of echinococcus.
When a person ingests the eggs, they hatch, and the larvae go to the liver and anyplace else, where they can grow into large (>10 cm) cysts. The cyst compresses organs and can cause severe morbidity. If the cyst ruptures, anaphylaxis is likely to result (J. For. Sci. 38: 978, 1993. Physicians with needles take notice.) If the cyst ruptures, one of the internal daughter cysts can become a primary cyst.
TREMATODES ("flukes")
Fascioliasis ("sheep liver fluke") Fasciola hepatica, the big "liver fluke", a 4 cm flatworm, is common in the tropics throughout the world. Usually a parasite of sheep and cattle, people acquire it from eating watercress contaminated with eggs. The worm lives in the biliary tree, where it produces fibrosis and often episodes of obstruction. While the disease is self-limited, treatment is advisable to prevent worse fibrosis.
Clonorchiasis ("Chinese liver fluke") Clonorchis sinensis inhabits the Orient. Infection is acquired from eating poorly-cooked fish (i.e., sushi). It is undergoing a resurgence in China thanks for increased fresh-water fishing. Heavy infestations produce deformity and scarring of the liver. This parasite places its host at risk for cholangiocarcinoma (cancer of the bile ducts).
* Opisthorchiasis: the Polish cat liver fluke. I've never seen one. You may hear C. sinensis called O. sinensis.
Fasciolopsiasis A 7 cm long flatworm that lives in the small bowel, causing various intestinal symptoms. The reservoir is the pig, with people sometimes serving as an alternative host. When the eggs reach the water, they reproduce in certain snails.
Paragonimiasis ("Oriental lung fluke")
{32034} paragonimus
This is a 12 mm flatworm that inhabits the lung and causes widespread morbidity in the Far East. The worm acts as a foreign body, producing repeated bacterial infection leading to serious disease. The worm's life cycle requires both a snail and a crustacean. Humans acquire the infection from eating the latter, uncooked. Larvae hatch in the gut, pass through the wall and reach the lungs. Coughed-up eggs are swallowed and passed into the feces. You can catch the critter in the U.S., too. Please be sure your crabs and crayfish are cooked. See Chest 121: 1368, 2002.
 Schistosomiasis ("blood flukes"; Sci. Am. 298(5): May 2008)
Schistosomiasis ("blood flukes"; Sci. Am. 298(5): May 2008)
{06215} mama and papa schistosome
{15739} mama and papa schistosome
{08236} mansoni eggs
{08298} mansoni egg
{08211} hematobium, egg in bowel
{09863} hematobium, bladder (granuloma with eggs in the center)
{08250} hematobium
{10676} japonicum eggs
 Schistosomiasis
Schistosomiasis
Pittsburgh Pathology Cases
Three worms that inhabit the veins of humans and cause problems when their eggs elicit a tissue reaction. Around 200 million people are affected worldwide; many are crippled and around 200,000 die each year; the number has been stable for two decades (2011). Mama Schistosome, in Papa Schistosome's enduring embrace, lays 500 eggs per day. This might be the fastest metabolism in a multicellular organism. The life cycle of blood flukes is complex and requires particular snails. The infection is acquired from contact with contaminated water. Eggs are equipped with razor-sharp spines to cut their way into the intestine.
Schistosomiasis is in the differential diagnosis of most things, and you should learn where it can be contracted: S. mansoni: Africa, Latin America, Puerto Rico (should soon be eliminated: Am. J. Trop. Med. 60: 313, 1999) S. hematobium Egypt & thereabouts S. japonicum China, Philippines
The patient's complaints depend on where the organism likes to locate: S. mansoni: hepatic fibrosis and cirrhosis S. hematobium bladder fibrosis and carcinoma S. japonicum: hepatic fibrosis and cirrhosis
Mansoni and japonicum produce primarily hepatic fibrosis by laying eggs in the portal veins. When portal hypertension supervenes, the eggs will embolize to the lungs to produce pulmonary hypertension and a miserable death. Hematobium infestation eventually leads either to obstructive kidney failure or squamous cell carcinoma of the (metaplastic) bladder epithelium. Actually, any schistosome can produce a host of syndromes depending on where it localizes. Even CNS involvement is not rare. Salmonella can find a chronic nidus in the coat of a schistosome. * We don't know for certain why the body doesn't reject the "foreign" schistosome. The worm does coat itself with some of the host's tissue antigens. Everyone memorizes schistosome eggs for "trivia" contests: S. mansoni: oval egg, large lateral spine S. hematobium: oval egg, large terminal spine S. japonicum: round egg, small lateral spine
Katayama fever is an allergic illness that results when the schistosome larvae first penetrate human skin and enter the bloodstream. When travellers who have never met the schistosome before acquire a heavy load, a spectacular eosinophilic pneumonitis can develop and last for several weeks (Am. J. Med. 109: 718, 2000). There hasn't been much progress on a vaccine since the initial enthusiastic reports (Science 251:630, 1991; why it still isn't working Sci. Am. May 2008). Don't confuse the deadly schistosomiasis with "swimmer's itch", caused by bird schistosomes penetrating the skin. (They don't get very far.)

BIGGER CRITTERS
You'll learn about fire ants (wheal-flare-pustule, J. Allerg. Clin. Imm. 93: 8447, 1994; lethal AJFMP 19: 137, 1998), bees and wasps, spiders (house spiders leave you with a pair of wheal-and-flares, brown recluses get you a skin graft, black widows simulate tetanus ), lice, scabies (itchy finger-and-toe webbing, more), flesh-dwelling flies (tropical "myiasis"), ticks (remember "tick paralysis", caused by the ongonig attachment of a pregnant female tick, producing a neurotoxin -- this is the one non-infectious complication of a tick bite), scorpions, and poisonous snakes in clinic. Scabies and lice: Lancet 355: 819, 2000.
), lice, scabies (itchy finger-and-toe webbing, more), flesh-dwelling flies (tropical "myiasis"), ticks (remember "tick paralysis", caused by the ongonig attachment of a pregnant female tick, producing a neurotoxin -- this is the one non-infectious complication of a tick bite), scorpions, and poisonous snakes in clinic. Scabies and lice: Lancet 355: 819, 2000.
{08248} crab lice
Final note: I think most scientists have agreed for decades that it would be good (for the long run) to reduce or eliminate antibiotic use to promote the growth of farm animals. This has been politically impossible in the US until recently, but it may be catching on (thank for once, Mickey D's). See Science
301: 1027, 2003. * Fun to know: Here are some real zebras that produce episodes of fever of unknown origin that can baffle physicians for your whole life:
- hyper IgD syndrome
- Muckle-Wells (autosomal dominant, a pyrin family mutation)
- tumor-necrosis factor receptor associated periodic syndrome (TRAPS; dominant mutation at the gene, Arth. Rheum. 48: 2386, 2003)
- chronic infantile neurological cutaneous and articular syndrome (CINCA, yet another pyrin family mutation)
- nodulosis, arthropathy, and osteolysis syndrome
- PFAPA: periodic fever with aphthous stomatitis, pharyngitis, and cervical adenitis
If you have the opportunity, read Rudyard Kipling's famous alternative-history science fiction story, "The Eye of Allah" -- medieval Arab scientists invent the microscope and discover the true nature of infectious disease. Roger Bacon and his friends wonder whether this knowledge is too dangerous for humankind.
BIBLIOGRAPHY / FURTHER READING
I urge anyone interested in learning more about the pathology of infectious disease to consult these standard textbooks.
In my notes, the most helpful current journal references are embedded in the text. Students using these during lecture strongly prefer this. And because the site is constantly being updated, numbered endnotes would be unmanageable. What's available online, and for whom, is always changing. Most public libraries will be happy to help you get an article that you need. Good luck on your own searches, and again, if there is any way in which I can help you, please contact me at scalpel_blade@yahoo.com. No texting or chat messages, please. Ordinary e-mails are welcome. Health and friendship!


 I am active in HealthTap, which provides free medical guidance from your cell phone. There is also a fee site at www.afraidtoask.com.
I am active in HealthTap, which provides free medical guidance from your cell phone. There is also a fee site at www.afraidtoask.com.


 I'm still doing my best to answer everybody. Sometimes I get backlogged, sometimes my E-mail crashes, and sometimes my literature search software crashes. If you've not heard from me in a week, post me again. I send my most challenging questions to the medical student pathology interest group, minus the name, but with your E-mail where you can receive a reply. Numbers in {curly braces} are from the magnificent Slice of Life videodisk. No medical student should be without access to this wonderful resource.
I'm still doing my best to answer everybody. Sometimes I get backlogged, sometimes my E-mail crashes, and sometimes my literature search software crashes. If you've not heard from me in a week, post me again. I send my most challenging questions to the medical student pathology interest group, minus the name, but with your E-mail where you can receive a reply. Numbers in {curly braces} are from the magnificent Slice of Life videodisk. No medical student should be without access to this wonderful resource.  I am presently adding clickable links to images in these notes. Let me know about good online sources in addition to these:
I am presently adding clickable links to images in these notes. Let me know about good online sources in addition to these:  My team:
My team: My home pageMore of my notes
My home pageMore of my notes
No comments:
Post a Comment