Parkinson's Disease, Meniere's Syndrome, Trigeminal Neuralgia and Bell's Palsy: One Cause, One Correction
By Michael T. Burcon, DC
Abstract I currently have 16 Meniere's syndrome, two Parkinson's disease, two Trigeminal neuralgia and two Bell's palsy patients under my care. They all have one thing in common: The atlas vertebra is subluxated posteriorly, which has caused the head to project forward, taking away the healthy curve of the neck. In each patient, the pelvis has twisted to take pressure off the important nerves in the upper neck and brainstem, causing one leg to appear shorter than the other; normal lumbar curvature is compromised; and finally, if not specifically adjusted, the patient compensates by developing an exaggerated curve in the thoracic spine.
I hypothesize that in each patient, kink(s) in the neck inhibited the normal flow of cerebrospinal fluid out of the skull and down the spine; this created excess pressure in the fourth ventricle, causing abnormal function of some of the structures in the midbrain. It also inhibited the flow of blood into the occipital area of the brain by kinking one of the vertebral arteries. Additionally, I suggest that the posterior atlas irritated the anterolateral aspect of the brainstem, irritating any combination of the bottom seven cranial nerves.
All 22 patients improved dramatically after one or two adjustments under cervical-specific chiropractic care. When the atlas returns to juxtaposition, the spinal cord relaxes and actually positions itself lower within the spinal column.
Key Terms: Parkinson's disease; Meniere's syndrome; Trigeminal neuralgia; Bell's palsy, posterior atlas subluxation; specific adjustment.
Introduction
Parkinson's disease (PD, Paralysis Agitans, or "Shaking Palsy") is an idiopathic, slowly progressive, degenerative central nervous system (CNS) disorder with four characteristic features: slowness and poverty of movement; muscular rigidity; resting tremor; and postural instability. Parkinson's disease is the fourth-most-common neurodegenerative disease afflicting the elderly: It affects about 1 percent of the population over 65 years old, compared with 0.4 percent of the population under 40 years old. The mean age of onset is about 57 years of age. Onset in childhood or adolescence (juvenile Parkinsonism) also occurs.1
The etiology and pathophysiology of primary Parkinsonism is loss of the pigmented neurons of the substantia nigra, locus ceruleus and other brainstem dopaminergic cell groups. The loss of substantia nigra neurons, which project to the caudate nucleus and putamen, results in depletion of the neurotransmitter dopamine in these areas.1
For 50 percent to 80 percent of patients with PD, the disease begins insidiously with a resting 4- to 8-Hz "pill-rolling" tremor of one hand. The tremor is maximal at rest; diminishes during movement; is absent during sleep; and is enhanced by emotional tension or fatigue. The hands, arms and legs usually are most affected, in that order. The jaw, tongue, forehead and eyelids also may be involved, although the voice is not affected. Many patients display only rigidity and never manifest tremor. Progressive rigidity, slowness and poverty of movement (bradykinesia) and difficulty in initiating movement (akinesia) follow.1
The face becomes mask-like and open-mouthed, with diminished blinking. Posture becomes stooped. Patients find it difficult to start walking; the gait becomes a shuffle with short steps and the arms are held flexed to the waist and fail to wing with stride. The steps may inadvertently quicken, and the patient may break into a run to keep from falling ("festination"). On examination, passive movement of the limbs is met with plastic, unvarying lead-pipe rigidity; superimposed tremor bursts may give ratchet-like cogwheel quality.1
The sensory examination usually is normal. Signs of autonomic nervous system function may be seen. Muscle strength usually is normal. Dementia occurs in about 50 percent of patients; depression also is common.1
The standard medical treatment for PD has been the administration of the drug Sinemet, which combines Levodopa (a short-acting drug that enters the brain and is converted into dopamine) and Carbidopa (which enhances Levodopa's action in the brain). Several neurosurgical techniques also exist, including thalamotomy (destruction of the ventral thalamus to control tremor); pallidotomy (destruction of the posterior ventral globus pallidus to control hyperkinetic symptoms); and deep- brain stimulation (electrode implantation for patient-controlled stimulation of the thalamus to control tremor). While medication and surgery may control symptoms temporarily, neither stops or reverses the progressive degeneration of the substantia nigra.2
B.J. Palmer reported the use of upper-cervical chiropractic care with PD patients as early as 1934. In his writings, he referred to patients with shaking palsy and listed improvement or correction of symptoms such as tremor; shaking; muscle cramps and/or contracture; joint stiffness; fatigue; lack of coordination; difficulty walking, or inability to walk; numbness; pain; and muscle weakness. His chiropractic care included paraspinal thermal scanning using a neurocalometer (NCM); a cervical radiographic series to analyze the upper-cervical spine; and a specific upper-cervical adjustment performed by hand. Erin L. Elster, DC, found no other references for the chiropractic management of PD patients, prior to her study on 10 PD patients in the year 2000, utilizing modern upper-cervical chiropractic care.2
Three-month re-evaluations revealed substantial improvement in subjective and objective findings in six of the 10 patients, and mild improvement in two patients. The findings of the other two patients, both over age 65, remained unchanged. According to the Unified Parkinson's Disease Rating Scale (UPDRS), six of 10 patients showed overall improvement ranging from 21 percent to 43 percent after three months of upper-cervical chiropractic care.2
Meniere's syndrome is characterized by vertigo or dizziness, and some combination of four associated symptoms: nausea, inner-ear pressure, low-frequency hearing loss and tinnitus. The cause of Meniere's syndrome is unknown and the pathology is poorly understood.1 The attacks of vertigo appear suddenly, last from a few to 24 hours, then subside gradually. The attacks are associated with nausea and vomiting. The patient may feel a recurrent feeling of fullness in the affected ear, and the hearing in that ear tends to fluctuate, but worsens over the years. Tinnitus may be constant or intermittent.
Trigeminal neuralgia (Tic Douloureux) is a disorder of the trigeminal nerve producing bouts of severe, lancinating pain lasting seconds to minutes in the distribution of one or more of its sensory divisions, most often the mandibular and/or maxillary. The cause is uncertain. Recently, surgery at autopsy suggests that this condition is essentially a compressive neuropathy of the brainstem.1
Bell's palsy is a unilateral facial paralysis of sudden onset and unknown cause. Pain behind the ear may precede the facial weakness that develops within hours, sometimes to complete paralysis. The mechanism is presumed to involve swelling and compression of the facial nerve. (1)
In addition to the upper-cervical chiropractic care based on the research of B.J. Palmer, with the assistance of Lyle Sherman, DC (later refined by William G. Blair, DC), I have added the lower-cervical research and adjustment utilized by Walter Vern Pierce, DC, into a technique that I refer to as "cervical-specific chiropractic."3
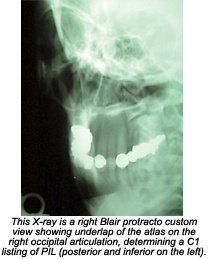
In my previous research with cases involving brainstem irritation (Meniere's disease, Trigeminal neuralgia and Bell's palsy), I discovered that the main cause was cervical trauma. The trauma forced the top cervical vertebra (atlas) to subluxate posteriorly, with laterality on the opposite side of the patient's symptoms (i.e., if the patient had fullness and gradual loss of hearing in the right ear, the atlas listing would be posterior and inferior on the left [PIL]). These same findings are substantiated by my Parkinson's research.4
Methods
My technique is based on the work of B.J. Palmer, as developed at his research clinic at Palmer Chiropractic College in Davenport, Iowa, from the early 1930s until his death in 1961.5-7 I have also studied the vertebral subluxation pattern work of B.J.'s clinic director, Lyle Sherman, DC, for whom Sherman College of Straight Chiropractic, is named.8
A detailed case history is taken on the first visit, followed by a spinal examination. First, the patient's cervical spine is graphed, using an advancement of the dual-probed NCM first used by B.J.9 Next, cervical motion palpation is performed, noting any aberrant motion of the vertebrae.
Detailed leg checks are performed on each patient visit, utilizing the work of J. Clay Thompson, DC, and Clarence Prill, DC.10 With the patient prone, an apparent short leg often is noted. The patient is instructed to turn his or her head to the right. If the short leg becomes more balanced, a right cervical syndrome is listed. The patient is then instructed to turn the head to the left. If the short leg becomes more balanced, a left cervical syndrome is listed. If both movements lengthen the short leg, a bilateral cervical syndrome is listed.
Modified Prill leg checks are used to determine the major cervical subluxation. The top four cervical vertebrae are tested as instructed by the Blair Chiropractic Society. They are referred to as "modified" because Dr. Prill uses the arms to detect imbalances, whereas Blair chiropractors use the legs. Patrick J. Sweeney, DC, and I refined the tests for the bottom three cervical vertebrae.
Atlas (C1) is tested by instructing the patient to "gently and steadily raise both feet." The doctor resists by holding the heels of the feet with his open hands. If the short leg stays short or becomes shorter, it is listed as a positive test for nerve interference at the level of C1. It is postulated that the flexion and extension of the leg correlates to the flexion and extension of the head, 50 percent of which occurs at the atlas.
Axis (C2) is tested by instructing the patient to "gently and steadily pull the feet together," while the doctor resists foot rotation. The rotation of the feet correlates to the rotation of the head, 50 percent of which occurs at axis. The third cervical vertebra is tested by having the patient pull his or her legs together; C4 is tested by having the patient pull the legs apart.
The fifth cervical is tested by having the patient raise both arms while the doctor holds the biceps. The patient raises his or her arms while the doctor holds brachioradialis muscles to test C6, and pushes the arms down while the doctor holds the triceps to test C7.
Three cervical X-rays are then taken to get listings for the segments that test positive and to check for contraindications to adjusting: lateral, A-P open-mouth and nasium. The lateral is used to check for a posterior kink in the lower cervicals; the A-P is used to check for translation, usually the result of a "T-bone" automobile accident; and the nasium is used to determine the atlas listing, utilizing the Blair theory of upper-cervical subluxation. There are only four atlas listings in Blair work. Dr. Blair's research demonstrated that there is no pure lateral movement at C1. The atlas will tend to articulate properly on one condyle while partially slipping off from the other.11
If the atlas subluxates anteriorly, it must move superiorly, due to the "rocker" shape of the articulation. If it tracks on the left, the atlas will show an overlap on the right articulation on the nasium. This is listed as an "ASR" (anterior and superior on the left). If it tracks on the right, it will overlap on the left ("ASL"). Anterior listings are more common and tend to be less symptomatic than posterior listings.
Typically, a posterior atlas subluxation is the result of head, neck or upper-back trauma. If the atlas subluxates posteriorly, it must also move inferiorly. If it tracks on the right, it will underlap on the left. This listing is "PIR" (posterior and inferior on the right). If it tracks on the left, it underlaps on the right, and is listed as "PIL."
I postulate that one reason a patient can have a problem on the opposite side of his or her posterior listing is that this is the side at which the atlas is not articulating properly with the occiput. Over time, this can cause irritation in that area, leading to inflammation and eventually scarring. I feel the vertebral artery often is kinked on that side, adding to the problem. One thing I'll never forget from cadaver dissection is how every structure seemed to be fighting for its space within the human body. This was especially true at the surprisingly small junctions between the skull and the upper cervicals, and the junction between the base of the neck and the thorax.
No adjustment is given on the first visit. A pattern of subluxation must be established on the second visit; patients are checked on subsequent visits. If the pattern has not returned, no adjustment is given. The atlas is always the first segment adjusted. The technique used varies, depending on radiographic analysis. If the major misalignment is translation, a side-posture toggle-recoil technique is used ("hole in one"). If the major component of the subluxation is posteriority, a prone position is used. A drop mechanism is used on all adjustments. If, after the atlas holds, positive tests persist in other cervical segments, those vertebrae are adjusted. Again, both side-posture and prone positions are used on the lower cervicals. Patients rest for 15 minutes after every adjustment, then are checked. Patients are released only after their legs present balanced.
The UPDRS is used on every visit to graph any improvement in symptoms. Thirty-one separate areas are graded, covering mentation, behavior and mood, activities of daily living and motor examination. Each area is graded 0 for no problem; 1 for a mild problem; 2 for a moderate problem; 3 for a severe problem; or 4 for a persistent problem.
Case Reports
Case #1
History: A 74-year-old retired male truck driver diagnosed with Parkinson's in 1994. He broke his right collarbone and left wrist falling off a ladder (about eight feet) onto the right side of his head in 1991. He was diagnosed with Meniere's syndrome in 1985 and Bell's palsy in 1983. He suffered a low-speed auto accident in 1974.
Medications included Permax and Singmet. He plays golf occasionally and bowls regularly.
Examination: Patient presented with tremor of left hand and jaw and reported restlessness and inability to sleep. He was disappointed because he and his wife could not go to Florida this winter, which they had been doing for several years. UPDRS totaled 44 points; inability to rise out of a chair was the highest score (3).
Thermograph reading was 3¡ cold at the bottom of the cervicals, increasing to 5¡ at the top. Patient had a three-quarter-inch short left leg; half-inch right cervical syndrome (RCS); and positive modified Prill tests on C1, C2 and C5.
Lateral X-ray revealed a severe kink at C4/5, AP showed the axis to be body-left, and nasium determined the atlas to be PIR.
Intervention and Outcome: Patient presented with a pattern of subluxation on the second visit. Atlas was adjusted with patient in prone position with the chin tucked toward the chest. Knife-edge contact was made lateral to the spinous process of the axis with the doctor standing on the right side of the table. Line of drive was mostly posterior to anterior (P-A), somewhat inferior to superior I-S. Patient's hand tremor ceased immediately with the adjustment.
After a 15-minute rest, there still was no evidence of tremor, which was noted as constant on his first visit. I had the patient attempt to get out of a chair without assistance - he could not. I repeated the leg checks; the only positive test was for C5. I challenged the segment on the right, and the short leg went shorter. The challenge while standing on the left balanced the legs.
I did a Pierce technique adjustment on C5, standing on the left side of the table, using a knife-edge contact below the spinous process. The adjustment was mostly P-A, some I-S, using the drop mechanism. Again, the patient was allowed to rest for 15 minutes. There still was no tremor, and this time, he was able to lift himself out of a chair without help.
Case #2
History: A 21-year-old female college student employed as a receptionist in a medical office. She had been taking Tegretol and Neurotin for the previous year after being diagnosed with Trigeminal neuralgia. She was doing poorly in school, which she attributed to the effects of medication use.
She was diagnosed with scoliosis at age 9. Her mother reported that her delivery was difficult. She denied being in any auto accidents, but she did play contact sports in high school.
Examination: Leg checks showed a three-quarter-inch right pelvic negative (RPN), one-inch bilateral cervical syndrome, and positive C1 and C5 Prill tests. She had limited range of motion on bilateral cervical rotation and left-lateral cervical flexion.
Her left ear was noticeably higher than her right. X-ray showed a PIL atlas, body left axis and posterior C5.
Intervention and Outcome: Subjective findings included lightheadedness from medications; stabbing, burning and throbbing right maxillary pain; and low-back pain. I adjusted her atlas PIL using the side-posture toggle-recoil technique. She reported dizziness on her next visit. I adjusted C5 after it tested positive for nerve interference.
On her third visit, I adjusted her sacrum; on her fourth visit, she presented balanced and pain-free and was not adjusted. She discontinued her medications and held her atlas adjustment for eight months. She lost her adjustment when she received a neck massage. Her second atlas adjustment has held for 16 months.
Case #3
History: A 46-year-old married Caucasian female diagnosed with Trigeminal neuralgia (left mandibular); Sjogren's syndrome; irritable bowel syndrome; erythema multiforme; allergies; and Raynaud's phenomon. She reported whiplash stemming from a rear-end automobile collision in 1998.
Examination: A half-inch right pelvic positive (RPP) and positive Prill tests for C1 and C5 were noted, as was limited range of motion for left lateral cervical flexion. X-rays showed evidence of atlas PIR and C5 posterior subluxations. She was hoarse, which was later diagnosed as a staff infection of her lungs.
Intervention and Outcome: The atlas and C5 were adjusted on the first visit. The fifth cervical and fifth lumbar were adjusted on the second visit. The axis and sacrum were adjusted on the third visit, and C5 and the sacrum on the fourth. She presented balanced and pain-free on the fifth visit, after two months of specific care. She is still holding her balance after two months.
Case #4
History: A 78-year-old male who woke up with right facial paralysis. He was an existing patient being treated for cervicalgia and severe motion restriction of the cervicals. His chief complaint was that he could no longer look over his shoulder to back out of his driveway.
He was also experiencing low-back pain and some problems with his right shoulder and right hip. He was being medicated for high blood pressure and had a history of a minor stroke.
Examination: One-inch LPP with positive Prill C5 and C1 tests were noted. X-rays showed a PIL atlas and posterior fifth and sixth cervicals. Apparent stenosis of the entire spine was noted.
Intervention and Outcome: I adjusted his C5 P-A and atlas PIL using an adjusting instrument. He said he was feeling only somewhat better after his 15-minute rest, but called the next morning to report that the paralysis was mostly gone. It was completely gone after three days and has not returned in the last two years.
Case #5
History: This 88-year-old female suffered frequent episodes of vertigo, tinnitus and nausea for 45 years. She was in a moderate car accident a few years before onset, in which she was a passenger and was not wearing a seat belt. During episodes, she walked around her home holding onto the walls, trying to keep her head level at all times. She reported numerous falls over the years, some resulting in broken bones.
She was diagnosed with Meniere's disease at the University of Michigan Hospital in Ann Arbor and Memorial Hospital in Chicago. She tried a variety of medications to help sleep, but saw no reduction of symptoms. Surgical history of colostomy and right radical mastectomy was noted.
Examination: Subject reported severe dizziness; blindness in the left eye; fullness in the right ear; pain and stiffness of the neck; and numbness in the left thumb. She was unable to lift her left arm above her shoulder. She exhibited limited range of motion with left lateral flexion and left rotation of the head. Edema was noted below the posterior base of the occiput.
Leg checks showed a one-inch RPP and a one-inch left cervical syndrome. Modified Prill check elicited positive test for C1 subluxation. Cervical X-rays revealed narrowed disc spaces at multiple levels, particularly evident at C6 and C7. Minimal marginal spurring and bony overgrowth of facet margins were noted. The atlas was subluxated posterior and inferior on the left articulation, underlapped on the right. The fifth cervical was inferior and posterior.
Intervention and Outcome: Immediately following specific toggle-recoil adjustment of the atlas, the patient reported complete alleviation of vertigo and dizziness. When she awoke the following morning, the tinnitus also was gone. She held this adjustment and was symptom-free for two years.
After suffering a minor stroke, closely followed by three compression fractures caused by osteoporosis, the subluxation returned and a second adjustment was given. This adjustment has held for the past year.
Discussion
All of my Parkinson's, Meniere's, Trigeminal neuralgia and Bell's palsy patients have suffered trauma to the upper back, neck and/or head, and they all presented with posterior atlas subluxations with laterality on the opposite side.
It is my theory that the pressure exerted by the subluxated atlas causes a combination of problems including, but not limited to, degenerative posture changes caused by carrying the skull too far anterior; decreased blood supply to the occipital portion of the brain; pressure on the nuclei of cranial nerves V (trigeminal) and VIII (vestibulocochlear); nerve-root irritation of cranial nerve VIII4; paralysis of the branches to the M. tensor veli palatini, which opens the Eustachian tubes;12 and/or compression preventing normal cerebrospinal fluid flow downward from the fourth ventricle into the spinal subarachnoid space, resulting in hydrocephalus. Conclusion
Anyone who has had trauma to the upper body, neck and/or head, or been diagnosed with any disease related to a problem with the brainstem, should be evaluated by an upper-cervical-specific chiropractor.
References
- The Merck Manual, 16th edition. Berkow RR. N.J.: Merck Research Laboratories, Merck & Co. Inc., 1999.
- Elster EL. Parkinson's disease: upper cervical chiropractic management of Parkinson's disease patients, Today's Chiropractic, July-August 2000.
- Pierce WV. Results, CHIRP, Inc., Dravosburg, Penn., 1981.
- Burcon MT. Upper cervical protocol for ten Meniere's patients, Journal of Vertebral Subluxation Research; passed peer review and waiting publication.
- Palmer BJ. The Subluxation Specific, The Adjustment Specific. Davenport, Iowa: Palmer School of Chiropractic, 1934.
- Palmer BJ. Chiropractic Clinical Controlled Research. Volume XXV. Davenport, IA: The B.J. Palmer Chiropractic Clinic, 1951.
- Palmer BJ. History in the Making. Volume XXXV. Davenport, IA: Palmer School of Chiropractic, 1957.
- Sherman L. Neurocalometer-neurocalograph-neurotempometer research. Eight BJ Palmer Chiropractic Clinic Cases. Davenport, IA: Palmer School of Chiropractic' 1951.
- Burcon MT. BJ's $50,000 timpograph, Chiropractic Economics, Nov/Dec 1995.
- Prill CE. The Prill Chiropractic Spinal Analysis Technique, 2001.
- Addington EA. Overview of Blair Cervical Technique, Council on Chiropractic Practice, Chandler, AZ, October 2-3, 1995.
- Hamersma H. A New Look at Meniere's Syndrome. The Ear, Nose and Throat Institute of Johannesburg, Florida Park, Gauteng, South Africa.
No comments:
Post a Comment