Alzheimer’s may be a Brain Infection and Amyloid Beta is an Antimicrobial
Every now and again, I have the great pleasure of stumbling upon truly groundbreaking research. That was the case here. A 2010 study found that the amyloid-beta plaques common in Alzheimer’s and thought to be merely a by-product of some defunct brain process actually may be part of the innate immune system’s response to brain bacteria. It appears that amyloid is an anti-microbial peptide and a fairly potent one at that.
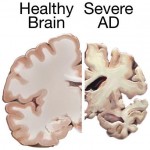
Over the last decade or so, researchers have postulated that Alzheimer’s may be a bacterial, viral, fungal or even a prion infection within the central nervous system (CNS). Nevertheless, most still believe that the amyloid buildup observed in the brain tissue of Alzheimer’s patients is an incidental and pathological marker of the growing disease. This research suggests a little re-thinking of that definition might be in order.
Amyloid is not a pathogenic by-product. It is an innate antibiotic that shares all the characteristics of the other CNS antimicrobials. It has receptors, initiates signal transduction and the cascade of expected immune system reactions against pathogens. More importantly, in direct tests, amyloid acts as an antibiotic against at least eight pathogens from candida (yeast) to streptococcus to staphylococcus, even E coli.
In the case of candida, the amyloid peptide was significantly more potent than the other known, innate CNS anti-infective. Interestingly, the highest density of amyloid and candida was found in the temporal lobe of Alzheimer’s patients. The temporal lobe is the region of the brain responsible for the most troubling cognitive deficit of Alzheimer’s, the memory disturbances, and the most severely damaged region as the disease progresses.
This research opens some entirely new directions in Alzheimer’s research. Could Alzheimer’s be related to body infections that somehow cross the blood brain barrier? Are there environmental factors that make the blood brain barrier more permeable to infection or other toxins? In our efforts to block the amyloid build-up, the target of many Alzheimer’s drugs, are we blocking the immune system’s ability to fight an infection? And certainly, by the time the amyloid plaques are visible, it is safe to assume that the infection and immune response have been on-going for years, are there markers that we have missed that appear much earlier on?
As a woman, I was most intrigued by the candida connection because 75% of all women will experience at least one yeast infection across their life time and 40% will experience more frequent infections. Some researchers suggest that chronic yeast infections caused by host immune deficiency are on the rise. Moreover, there is speculation that the high-sugar western diet and the over-use of antibiotics are to blame.
Despite this increase in yeast hyper-sensitivity in the gut and elsewhere in the body, brain or neuro-candida has been considered fairly rare and often fatal, at least in its acute stage. Indeed, it is rather difficult for most toxins to cross the blood brain barrier at all. So it is all the more striking that these researchers identified temporal lobe candida in Alzheimer’s patients and that it had likely been there chronically as evidenced by time-frame of the immune response required to create the visible amyloid plaques.
Perhaps, a more chronic, lower- intensity candida infection reaches the CNS and is almost but not quite battled successfully by the body’s innate immune system – the amyloid. Over time the innate immune system mounts a stronger and stronger defense until the very defense mechanisms begin to cause the problems we see as invasive amyloid plaques of Alzheimer’s. Interesting possibilities.
The full study: The Alzheimer’s Disease-Associated Amyloid β-Protein Is an Antimicrobial Peptide
Hormones Matter does not provide medical advice, diagnosis or treatment
No comments:
Post a Comment